Transcription
Medicare Advantage planwith prescription drugsEvidence ofcoverage 2022UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)Toll-free 1-866-480-1086, TTY 7118 a.m. - 8 p.m. local time, 7 days a weekwww.myUHCMedicare.comY0066 EOC R6801 011 000 2022 C
January 1 – December 31, 2022Evidence of coverageYour Medicare Health Benefits and Services and Prescription DrugCoverage as a Member of our planThis booklet gives you the details about your Medicare health care and prescription drug coveragefrom January 1 – December 31, 2022. It explains how to get coverage for the health care servicesand prescription drugs you need.This is an important legal document. Please keep it in a safe place.This plan, UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP), is insured throughUnitedHealthcare Insurance Company or one of its affiliates. (When this Evidence of Coveragesays “we,” “us,” or “our,” it means UnitedHealthcare. When it says “plan” or “our plan,” it meansUnitedHealthcare Dual Complete Choice (Regional PPO D-SNP).)UnitedHealthcare does not discriminate on the basis of race, color, national origin, sex, age, ordisability in health programs and activities.UnitedHealthcare provides free services to help you communicate with us such as letters in otherlanguages, Braille, large print, audio, or you can ask for an interpreter. Please contact ourCustomer Service number at 1-866-480-1086 for additional information (TTY users should call711). Hours are 8 a.m. - 8 p.m. local time, 7 days a week.UnitedHealthcare ofrece servicios gratuitos para ayudarle a que se comunique con nosotros. Porejemplo, cartas en otros idiomas, braille, letra grande, audio o bien, usted puede pedir unintérprete. Comuníquese con nuestro número de Servicio al Cliente al 1-866-480-1086, paraobtener información adicional (los usuarios de TTY deben comunicarse al 711). Los horarios deatención son de 8 a.m. a 8 p.m., hora local, los 7 días de la semana.Benefits, premium, deductible, and/or copayments/coinsurance may change on January 1, 2023.The formulary, pharmacy network, and provider network may change at any time. You will receivenotice when necessary.OMB Approval 0938-1051 (Expires: February 29, 2024)
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)Table of Contents2022 Evidence of coverageTable of contentsThis list of chapters and page numbers is your starting point. For more help in finding informationyou need, go to the first page of a chapter. You will find a detailed list of topics at the beginningof each chapter.Chapter 1Getting started as a member. 1-1Explains what it means to be in a Medicare health plan and how to use thisbooklet. Tells about materials we will send you, your plan premium, yourUnitedHealthcare member ID card, and keeping your membership record up todate.Chapter 2Important phone numbers and resources. 2-1Tells you how to get in touch with our plan (UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)) and with other organizations includingMedicare, the State Health Insurance Assistance Program (SHIP), the QualityImprovement Organization, Social Security, Medicaid (the state healthinsurance program for people with low incomes), programs that help peoplepay for their prescription drugs, and the Railroad Retirement Board.Chapter 3Using the plan’s coverage for your medical services.3-1Explains important things you need to know about getting your medical care asa member of our plan. Topics include using the providers in the plan’s networkand how to get care when you have an emergency.Chapter 4Medical Benefits Chart (what is covered and what you pay). 4-1Gives the details about which types of medical care are covered and notcovered for you as a member of our plan. Explains how much you will pay asyour share of the cost for your covered medical care.Chapter 5Using the plan’s coverage for your Part D prescription drugs. 5-1Explains rules you need to follow when you get your Part D drugs. Tells how touse the plan’s List of Covered Drugs (Formulary) to find out which drugs arecovered. Tells which kinds of drugs are not covered. Explains several kinds ofrestrictions that apply to coverage for certain drugs. Explains where to get yourprescriptions filled. Tells about the plan’s programs for drug safety andmanaging medications.Chapter 6What you pay for your Part D prescription drugs.6-1
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)Table of ContentsChapter 7Asking us to pay our share of a bill you have received for covered medicalservices or drugs. 7-1Explains when and how to send a bill to us when you want to ask us to pay youback for our share of the cost for your covered services or drugs.Chapter 8Your rights and responsibilities. 8-1Explains the rights and responsibilities you have as a member of our plan. Tellswhat you can do if you think your rights are not being respected.Chapter 9What to do if you have a problem or complaint (coverage decisions,appeals, complaints).9-1Tells you step-by-step what to do if you are having problems orconcerns as a member of our plan.· Explains how to ask for coverage decisions and make appeals if you arehaving trouble getting the medical care or prescription drugs you think arecovered by our plan. This includes asking us to make exceptions to the rulesor extra restrictions on your coverage for prescription drugs, and asking us tokeep covering hospital care and certain types of medical services if you thinkyour coverage is ending too soon.· Explains how to make complaints about quality of care, waiting times,customer service, and other concerns.Chapter 10Ending your membership in the plan. 10-1Explains when and how you can end your membership in the plan. Explainssituations in which our plan is required to end your membership.Chapter 11Legal notices.11-1Includes notices about governing law and about non-discrimination.Chapter 12Definitions of important words. 12-1Explains key terms used in this booklet.Questions? Call Customer Service at 1-866-480-1086, TTY 711, 8 a.m. - 8 p.m. local time,7 days a week
Chapter 1Getting started as a member
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-1Chapter 1: Getting started as a memberChapter 1Getting started as a memberSection 1Introduction.3Section 1.1 You are enrolled in UnitedHealthcare Dual Complete Choice(Regional PPO D-SNP), which is a specialized Medicare AdvantagePlan (Special Needs Plan).3Section 1.2 What is the Evidence of Coverage booklet about?. 3Section 1.3 Legal information about the Evidence of Coverage.4Section 2What makes you eligible to be a plan member?.4Section 2.1 Your eligibility requirements. 4Section 2.2 What are Medicare Part A and Medicare Part B?. 5Section 2.3 What is Medicaid?.5Section 2.4 Here is the plan service area for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP). 6Section 2.5 U.S. Citizen or Lawful Presence. 6Section 3What other materials will you get from us?. 6Section 3.1 Your UnitedHealthcare member ID card – Use it to get all covered careand prescription drugs. 6Section 3.2 The Provider Directory: Your guide to all providers in the plan’snetwork. 7Section 3.3 The Pharmacy Directory: Your guide to pharmacies in our network. 8Section 3.4 The plan’s List of Covered Drugs (Formulary).8Section 3.5 The Part D Explanation of Benefits (the “Part D EOB”): Reports with asummary of payments made for your Part D prescription drugs.9Section 4Your monthly premium for the plan.9Section 4.1 How much is your plan premium?.9Section 4.2 There are several ways you can pay your plan premium. 11Section 4.3 Can we change your monthly plan premium during the year?.12Section 5Please keep your plan membership record up to date.12Section 5.1 How to help make sure that we have accurate information about you 12Section 6We protect the privacy of your personal health information. 13
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-2Chapter 1: Getting started as a memberSection 6.1 We make sure that your health information is protected. 13Section 7How other insurance works with our plan.13Section 7.1 Which plan pays first when you have other insurance?. 13
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-3Chapter 1: Getting started as a memberSection 1IntroductionSection 1.1You are enrolled in UnitedHealthcare Dual Complete Choice(Regional PPO D-SNP), which is a specialized Medicare AdvantagePlan (Special Needs Plan)You are covered by both Medicare and Medicaid:· Medicare is the Federal health insurance program for people 65 years of age or older, somepeople under age 65 with certain disabilities, and people with end-stage renal disease (kidneyfailure).· Medicaid is a joint Federal and state government program that helps with medical costs forcertain people with limited incomes and resources. Medicaid coverage varies depending onthe state and the type of Medicaid you have. Some people with Medicaid get help paying fortheir Medicare premiums and other costs. Other people also get coverage for additionalservices and drugs that are not covered by Medicare.You have chosen to get your Medicare health care and your prescription drug coverage throughour plan, UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP).There are different types of Medicare health plans. UnitedHealthcare Dual Complete Choice(Regional PPO D-SNP) is a specialized Medicare Advantage Plan (a Medicare “Special NeedsPlan”), which means its benefits are designed for people with special health care needs.UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP) is designed specifically forpeople who have Medicare and who are also entitled to assistance from Medicaid.Coverage under this Plan qualifies as Qualifying Health Coverage (QHC) and satisfies thePatient Protection and Affordable Care Act’s (ACA) individual shared responsibility requirement.Please visit the Internal Revenue Service (IRS) website at: s-and-Families for more information.Because you get assistance from Medicaid, you will pay less or nothing for some of your Medicarehealth care services. Medicaid may also provide other benefits to you by covering health careservices and prescription drugs that are not usually covered under Medicare. You will also receive“Extra Help” from Medicare to pay for the costs of your Medicare prescription drugs.UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP) will help manage all of thesebenefits for you, so that you get the health care services and payment assistance that you areentitled to.UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP) is run by a private company. Likeall Medicare Advantage plans, this Medicare Special Needs Plan is approved by Medicare. Theplan also has a contract with the Texas Medicaid program to coordinate your Medicaid benefits.We are pleased to be providing your Medicare health care coverage, including your prescriptiondrug coverage.Section 1.2What is the Evidence of Coverage booklet about?
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-4Chapter 1: Getting started as a memberThis Evidence of Coverage booklet tells you how to get your Medicare medical care andprescription drugs covered through our plan. This booklet explains your rights and responsibilities,what is covered, and what you pay as a member of the plan.The words “coverage” and “covered services” refer to the medical care, services and prescriptiondrugs available to you as a member of the plan.It’s important for you to learn what the plan’s rules are and what services are available to you. Weencourage you to set aside some time to look through this Evidence of Coverage booklet.If you are confused or concerned or just have a question, please contact our plan’s CustomerService (phone numbers are printed on the cover of this booklet).Section 1.3Legal information about the Evidence of CoverageIt’s part of our contract with youThis Evidence of Coverage is part of our contract with you about how the plan covers your care.Other parts of this contract include your enrollment form, the List of Covered Drugs (Formulary),and any notices you receive from us about changes to your coverage or conditions that affect yourcoverage. These notices are sometimes called “riders” or “amendments.”The contract is in effect for months in which you are enrolled in the plan between January 1, 2022and December 31, 2022.Each calendar year, Medicare allows us to make changes to the plans that we offer. This meanswe can change the costs and benefits of the plan after December 31, 2022. We can also choose tostop offering the plan, or to offer it in a different service area, after December 31, 2022.Medicare must approve our plan each yearMedicare (the Centers for Medicare & Medicaid Services) must approve our plan each year. Youcan continue to get Medicare coverage as a member of our plan as long as we choose to continueto offer the plan and Medicare renews its approval of the plan.Section 2What makes you eligible to be a plan member?Section 2.1Your eligibility requirementsYou are eligible for membership in our plan as long as:· You have both Medicare Part A and Medicare Part B (Section 2.2 tells you about Medicare PartA and Medicare Part B)· -- and -- you live in our geographic service area (Section 2.4 below describes our service area).· -- and -- you are a United States citizen or are lawfully present in the United States· -- and -- you meet the special eligibility requirements described below.
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-5Chapter 1: Getting started as a memberSpecial eligibility requirements for our planOur plan is designed to meet the needs of people who receive certain Medicaid benefits. (Medicaidis a joint Federal and state government program that helps with medical costs for certain peoplewith limited incomes and resources.) To be eligible for our plan you must be eligible for Medicarecost-sharing assistance under Medicaid.Please note: If you lose your Medicaid eligibility but can reasonably be expected to regain eligibilitywithin 6 month(s), then you are still eligible for membership in our plan (Chapter 4, Section 2.1 tellsyou about coverage during a period of deemed continued eligibility).Section 2.2What are Medicare Part A and Medicare Part B?When you first signed up for Medicare, you received information about what services are coveredunder Medicare Part A and Medicare Part B. Remember:· Medicare Part A generally helps cover services provided by hospitals (for inpatient services,skilled nursing facilities, or home health agencies).· Medicare Part B is for most other medical services (such as physician’s services, homeinfusion therapy, and other outpatient services) and certain items (such as durable medicalequipment (DME) and supplies).Section 2.3What is Medicaid?Medicaid is a joint Federal and state government program that helps with medical costs for certainpeople who have limited incomes and resources. Each state decides what counts as income andresources, who is eligible, what services are covered, and the cost for services. States also candecide how to run their program as long as they follow the Federal guidelines.In addition, there are programs offered through Medicaid that help people with Medicare pay theirMedicare costs, such as their Medicare premiums. These “Medicare Savings Programs” helppeople with limited income and resources save money each year.You can enroll in this plan if you are in one of these Medicaid categories:·Qualified Medicare Beneficiary Plus (QMB ): You get Medicaid coverage of Medicarecost-share and are also eligible for full Medicaid benefits. Medicaid pays your Medicare PartA and Part B premiums, deductibles, coinsurance and copayment amounts for Medicarecovered services. You pay nothing, except for Part D prescription drug copays (ifapplicable).·Qualified Medicare Beneficiary (QMB): You get Medicaid coverage of Medicare cost-sharebut are not eligible for full Medicaid benefits. Medicaid pays your Medicare Part A and PartB premiums, deductibles, coinsurance and copayment amounts only for Medicare coveredservices. You pay nothing, except for Part D prescription drug copays (if applicable).·Specified Low-Income Medicare Beneficiary (SLMB ): Medicaid pays your Part Bpremium and provides full Medicaid benefits. You are eligible for full Medicaid benefits. At
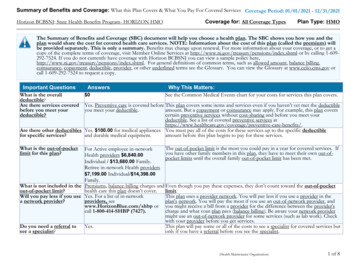
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-6Chapter 1: Getting started as a membertimes you may also be eligible for limited assistance from your state Medicaid agency inpaying your Medicare cost share amounts. Generally your cost share is 0% when the serviceis covered by both Medicare and Medicaid. There may be cases where you have to pay costsharing when a service or benefit is not covered by Medicaid.Section 2.4Here is the plan service area for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)Although Medicare is a Federal program, our plan is available only to individuals who live in ourplan service area. To remain a member of our plan, you must continue to reside in the plan servicearea. The service area is described below.Our service area includes these states: Texas.If you plan to move out of the service area, please contact Customer Service (phone numbers areprinted on the cover of this booklet).When you move, you will have a Special Enrollment Period that will allow you to switch to OriginalMedicare or enroll in a Medicare health or drug plan that is available in your new location.It is also important that you call Social Security if you move or change your mailing address. Youcan find phone numbers and contact information for Social Security in Chapter 2, Section 5.Section 2.5U.S. Citizen or Lawful PresenceA member of a Medicare health plan must be a U.S. citizen or lawfully present in the United States.Medicare (the Centers for Medicare & Medicaid Services) will notify UnitedHealthcare DualComplete Choice (Regional PPO D-SNP) if you are not eligible to remain a member on this basis.UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP) must disenroll you if you do notmeet this requirement.Section 3What other materials will you get from us?Section 3.1Your UnitedHealthcare member ID card – Use it to get all covered careand prescription drugsWhile you are a member of our plan, you must use your UnitedHealthcare member ID card for ourplan whenever you get any services covered by this plan and for prescription drugs you get atnetwork pharmacies. IMPORTANT – If you have Medicare and Texas Medicaid Health and HumanServices Commission (Medicaid), make sure to show your UnitedHealthcare member ID card andyour state Medicaid ID card whenever you access services. This will help your provider billcorrectly. Here’s a sample UnitedHealthcare member ID card to show you what yours will look like:
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-7Chapter 1: Getting started as a memberCustomer Service Hours: XXX - XXX, XXX - XXX, XXX XXX - XXXELMPHealth Plan (99999): 999-99999-99Member ID: 999999999-00 Group Number:Member:SAMPLE A MEMBERPayer ID:99999SACopay: PCP XXSpec XXH9999-999-999ER XXRxBIN:RxPCN:RxGrp:999999999999999XXXPlan NameFor MembersWebsite:Customer Service:Other Number:Other Number:SAELMPFor Providerswww.website.url1-999-999-9999 TTY 7111-999-999-9999 TTY 7111-999-999-9999 TTY 711www.website.urlMedical Claim Address: P.O. Box 99999, XXXXXX, XX 99999-9999UHC1-999-999-9999For Pharmacists 1-999-999-9999Pharmacy Claims P.O. Box 99999, XXXXXX, XX 99999-9999Client Alts0Internal & External TeamDate: 04.26.21Client Contact:Art Director/Designer: catchfireProject DetailsName: ID Card Template DesignStage: FINALFile Name: MAPD ID Card Back Template Design.inddColorCMYKDimensionsFlat: 3.4” x 2.15”Software: InDesign CCDo NOT use your red, white, and blue Medicare card for covered medical services while you are amember of this plan. If you use your Medicare card instead of your UnitedHealthcare member IDcard, you may have to pay the full cost of medical services yourself. Keep your Medicare card in asafe place. You may be asked to show it if you need hospital services, hospice services, orparticipate in routine research studies.Here’s why this is so important: If you get covered services using your red, white, and blueMedicare card instead of using your UnitedHealthcare member ID card while you are a planmember, you may have to pay the full cost yourself.If your UnitedHealthcare member ID card is damaged, lost, or stolen, call Customer Service rightaway and we will send you a new card. (Phone numbers for Customer Service are printed on thecover of this booklet.)Section 3.2The Provider Directory: Your guide to all providers in the plan’snetworkThe Provider Directory lists our network providers and durable medical equipment suppliers. Thisdirectory may also identify which providers participate in Texas Medicaid Health and HumanServices Commission (Medicaid). You may see any provider in the directory for plan coveredservices, even if they do not participate in Texas Medicaid Health and Human ServicesCommission (Medicaid). Please contact Texas Medicaid Health and Human Services Commission(Medicaid) for more information on participating Texas Medicaid Health and Human ServicesCommission (Medicaid) providers.What are “network providers”?Network providers are the doctors and other health care professionals, medical groups, durablemedical equipment suppliers, hospitals, and other health care facilities that have an agreementwith us to accept our payment and any plan cost-sharing as payment in full. We have arranged forthese providers to deliver covered services to members in our plan. The most recent list ofproviders and suppliers is available on our website at www.myUHCMedicare.com.
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-8Chapter 1: Getting started as a memberWhy do you need to know which providers are part of our network?As a member of our plan, you can choose to receive care from out-of-network providers. Our planwill cover services from either in-network or out-of-network providers, as long as the services arecovered benefits and medically necessary. However, if you use an out-of-network provider, yourshare of the costs for your covered services may be higher. See Chapter 3 (Using the plan’scoverage for your medical services) for more specific information.Because our plan is a Regional Preferred Provider Organization, if no contracted network provideris readily available within your plan service area you can access care at in-network cost-sharingfrom an out-of-network provider. Call Customer Service to let us know you need to see an out-ofnetwork provider, or to get help finding an out-of-network provider.If you don’t have your copy of the Provider Directory, you can request a copy from CustomerService (phone numbers are printed on the cover of this booklet). You may ask Customer Servicefor more information about our network providers, including their qualifications. You can alsosearch for provider information on our website. Both Customer Service and the website can giveyou the most up-to-date information about changes in our network providers. (You can find ourwebsite and phone information on the cover of this booklet.)Section 3.3The Pharmacy Directory: Your guide to pharmacies in our networkWhat are “network pharmacies”?Network pharmacies are all of the pharmacies that have agreed to fill covered prescriptions for ourplan members.Why do you need to know about network pharmacies?You can use the Pharmacy Directory to find the network pharmacy you want to use. There arechanges to our network of pharmacies for next year. An updated Pharmacy Directory is located onour website at www.myUHCMedicare.com. You may also call Customer Service for updatedprovider information or to ask us to mail you a Pharmacy Directory. Please review the 2022Pharmacy Directory to see which pharmacies are in our network.If you don’t have the Pharmacy Directory, you can get a copy from Customer Service (phonenumbers are printed on the cover of this booklet). At any time, you can call Customer Service to getup-to-date information about changes in the pharmacy network. You can also find this informationon our website at www.myUHCMedicare.com.Section 3.4The plan’s List of Covered Drugs (Formulary)The plan has a List of Covered Drugs (Formulary). We call it the “Drug List” for short. It tells whichPart D prescription drugs are covered under the Part D benefit included in our plan. The drugs onthis list are selected by the plan with the help of a team of doctors and pharmacists. The list mustmeet requirements set by Medicare. Medicare has approved the plan’s Drug List.
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-9Chapter 1: Getting started as a memberIn addition to the drugs covered by Part D, some prescription drugs are covered for you under yourMedicaid benefits. You can learn more about prescription drug coverage under your Medicaidbenefits by contacting your Medicaid health plan or Texas Medicaid Health and Human ServicesCommission (Medicaid) listed in Chapter 2 of this booklet. Your Medicaid health plan or TexasMedicaid Health and Human Services Commission (Medicaid) may also be able to provide aMedicaid Drug List that tells you how to find out which drugs are covered under Medicaid.The Drug List also tells you if there are any rules that restrict coverage for your drugs.We will provide you a copy of the Drug List. To get the most complete and current informationabout which drugs are covered, you can visit the plan’s website (www.myUHCMedicare.com) orcall Customer Service (phone numbers are printed on the cover of this booklet).Section 3.5The Part D Explanation of Benefits (the “Part D EOB”): Reports with asummary of payments made for your Part D prescription drugsWhen you use your Part D prescription drug benefits, we will send you a summary report to helpyou understand and keep track of payments for your Part D prescription drugs. This summaryreport is called the Part D Explanation of Benefits (or the “Part D EOB”).The Part D Explanation of Benefits tells you the total amount you, others on your behalf, and wehave spent on your Part D prescription drugs and the total amount paid for each of your Part Dprescription drugs during each month the Part D benefit is used. The Part D EOB provides moreinformation about the drugs you take, such as increases in price and other drugs with lower costsharing that may be available. You should consult with your prescriber about these lower costoptions. Chapter 5 (What you pay for your Part D prescription drugs) gives more informationabout the Part D Explanation of Benefits and how it can help you keep track of your drugcoverage.The Part D Explanation of Benefits is also available upon request. To get a copy, please contactCustomer Service (phone numbers are printed on the cover of this booklet).Section 4Your monthly premium for the planSection 4.1How much is your plan premium?As a member of our plan, you pay a monthly plan premium unless you qualify for “Extra Help” withyour prescription drug costs. You will not pay a monthly Plan premium (prescription drug planpremium) if you qualify for “Extra Help”. People with Medicare and Medicaid automatically qualifyfor “Extra Help”. Because you qualify for "Extra Help", for 2022 the monthly premium for our plan is 0.In some situations, your plan premium could be moreIn some situations, your plan premium could be more than the amount listed above in Section 4.1.This situation is described below.
2022 Evidence of Coverage for UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP)1-10Chapter 1: Getting starte
You have chosen to get your Medicare health care and your prescription drug coverage through our plan, UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP). There are different types of Medicare health plans. UnitedHealthcare Dual Complete Choice (Regional PPO D-SNP) is a specialized Medicare Advantage Plan (a Medicare "Special Needs