Transcription
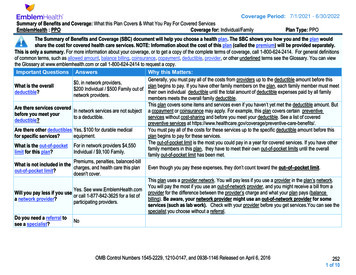
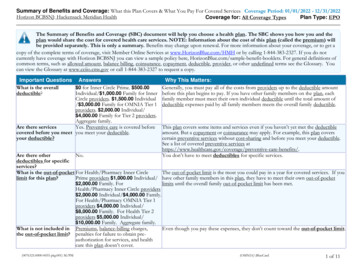
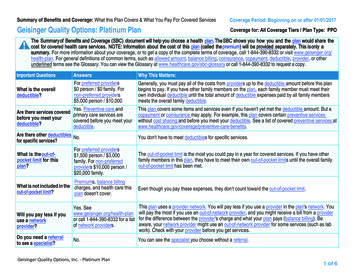
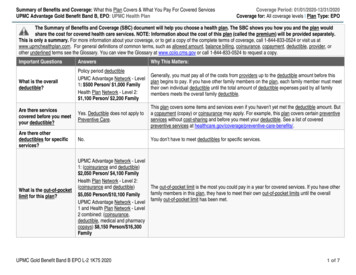
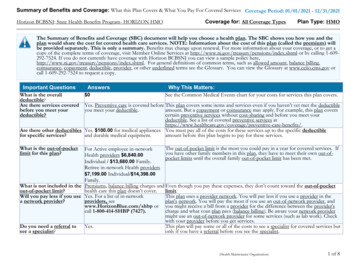
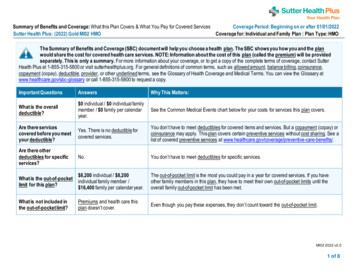
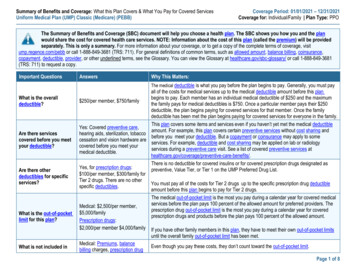
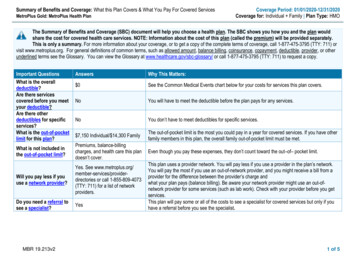
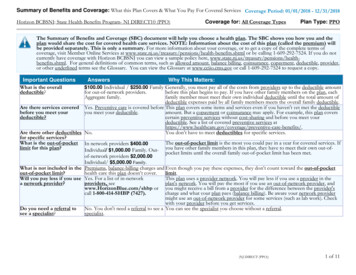
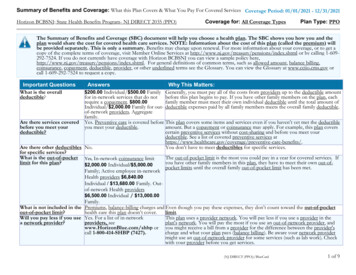
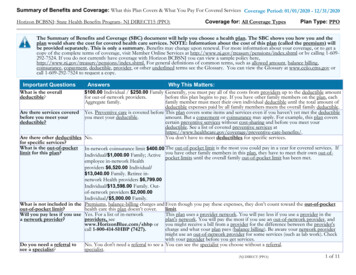
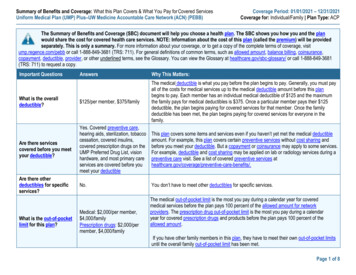
Summary of Benefits and Coverage: What this Plan Covers & What You Pay for Covered ServicesUniform Medical Plan (UMP) Plus–UW Medicine Accountable Care Network (ACN) (PEBB)Coverage Period: 01/01/2021 – 12/31/2021Coverage for: Individual/Family Plan Type: ACPThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the planwould share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be providedseparately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visitump.regence.com/pebb or call 1-888-849-3681 (TRS: 711). For general definitions of common terms, such as allowed amount, balance billing, coinsurance,copayment, deductible, provider, or other underlined terms, see the Glossary. You can view the Glossary at healthcare.gov/sbc-glossary/ or call 1-888-849-3681(TRS: 711) to request a copy.Important QuestionsAnswersWhy This Matters:What is the overalldeductible? 125/per member, 375/familyThe medical deductible is what you pay before the plan begins to pay. Generally, you must payall of the costs for medical services up to the medical deductible amount before this planbegins to pay. Each member has an individual medical deductible of 125 and the maximumthe family pays for medical deductibles is 375. Once a particular member pays their 125deductible, the plan begins paying for covered services for that member. Once the familydeductible has been met, the plan begins paying for covered services for everyone in thefamily.Are there servicescovered before you meetyour deductible?Yes. Covered preventive care,hearing aids, sterilization, tobaccocessation, covered insulins,covered prescription drugs on theUMP Preferred Drug List, visionhardware, and most primary careservices are covered before youmeet your deductibleThis plan covers some items and services even if you haven’t yet met the medical deductibleamount. For example, this plan covers certain preventive services without cost sharing andbefore you meet your deductible. But a copayment or coinsurance may apply to some services.For example, deductible and cost sharing may be applied on lab or radiology services during apreventive care visit. See a list of covered preventive services /.Are there otherdeductibles for specificservices?No.You don’t have to meet other deductibles for specific services.What is the out-of-pocketlimit for this plan?Medical: 2,000/per member, 4,000/familyPrescription drugs: 2,000/permember, 4,000/familyThe medical out-of-pocket limit is the most you pay during a calendar year for coveredmedical services before the plan pays 100 percent of the allowed amount for networkproviders. The prescription drug out-of-pocket limit is the most you pay during a calendaryear for covered prescription drugs and products before the plan pays 100 percent of theallowed amount.If you have other family members in this plan, they have to meet their own out-of-pocket limitsuntil the overall family out-of-pocket limit has been met.Page 1 of 8
Important QuestionsAnswersWhy This Matters:What is not included inthe out-of-pocket limit?Medical: Premiums, balancebilling charges, prescription drugcosts, member coinsurance paidto out-of-network providers andnon-network pharmacies,amounts paid for services thisplan doesn’t cover, amounts paidby the plan, amounts paid forservices over a benefit limit, andamounts that are more than themaximum dollar amount paid bythe plan.Even though you pay these costs, they don’t count toward the out-of-pocket limit.Will you pay less if youuse a network provider?Do you need a referral tosee a specialist?Prescription drugs: Costs formedical services and drugscovered under the medical benefit,prescription drugs and productsnot covered by the plan, amountspaid by the plan, and amountsexceeding the allowed amount forprescription drugs paid to nonnetwork pharmaciesYes. Visit the UMP website atump.regence.com/pebb or call 1888-849-3681 (TRS: 711) for a listof network providers. For a list ofnetwork pharmacies, visit thePrescription drugs webpage atump.regence.com/pebb/benefits/prescriptions or call 1-888-361-1611(TRS: 711).No.This plan uses a provider network. You will pay less if you use a provider or pharmacy in theplan’s network. You will pay the most if you use an out-of-network provider or an out-of-networkpharmacy, and you might receive a bill from a provider or pharmacy for the difference betweenthe provider’s or pharmacy’s charge and what your plan pays (balance billing). Be aware, yournetwork provider might use an out-of-network provider for some services (such as lab work).Check with your provider before you get services.UMP does not require a referral from your primary care provider to see a specialist.*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 2 of 8
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.Common Medical EventWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most) 0 for office visit with aprimary care network50% coinsuranceproviderPrimary care provider must be contractedwith UMP Plus–UW Medicine ACN to avoidcost-sharing.15% coinsurance50% coinsuranceNot applicable. 050% coinsuranceYou may have to pay for services that aren’tpreventive. Ask your provider if the servicesneeded are preventive. See a list of coveredpreventive services athealthcare.gov/coverage/preventive- carebenefits/.15% coinsurance50% coinsuranceNot applicable15% coinsurance50% coinsuranceCertain tests aren’t covered and other testsrequire preauthorization.PreventivePreventive: 0%Preventive: 0%Value TierValue Tier: 0-30 daysupply:5% coinsurance or 10,whichever is lessTier 1: 0-30 day supply:10% coinsurance or 25, whichever is lessValue Tier: 5%coinsuranceServices You May NeedPrimary care visit to treat aninjury or illnessIf you visit a health careprovider’s office orclinicIf you have a testIf you need drugs totreat your illness orconditionMore information aboutprescription drugcoverage is available alist visitPreventive care/screening/immunizationDiagnostic test (x-ray, bloodwork)Imaging (CT/PET scans,MRIs)Tier 1 drugsTier 2 drugsTier 2: 0-30 day supply:30% coinsurance or 75, whichever is lessCost-share depends onTier 1: 10% coinsuranceTier 2: 30% coinsuranceLimitations, Exceptions, & OtherImportant InformationNo coverage for prescription drugs with anover-the-counter alternative. Tier 1 does notinclude high-cost generic drugs. Cost-sharedepends on whether you get up to 30 days,60 days, or 90 days at a time. You canreceive up to a 90-day supply for someprescriptions. Preauthorization may berequired. Note: Postal Prescription Services(PPS) is the plan’s only network mail-orderpharmacy. Prescriptions purchased throughother mail-order pharmacies will not becovered.No coverage for prescription drugs with anover-the-counter alternative. Tier 2 alsoincludes some high-cost generic drugs.Preauthorization may be required. Note:*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 3 of 8
Common Medical EventServices You May NeedWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most)whether you get up to30 days, 60 days, or 90days at a time. You canreceive up to a 90-daysupply for someprescriptions.Preventive: 0%Value Tier: 0-30 daysupply: 5%coinsurance or 10,whichever is lessSpecialty drugsLimitations, Exceptions, & OtherImportant InformationPostal Prescription Services (PPS) is theplan’s only network mail-order pharmacy.Prescriptions purchased through other mailorder pharmacies will not be covered.Not coveredCoverage is limited to up to a 30-day supplyper prescription or refill from the plan'sspecialty pharmacy, Ardon Health.Preauthorization is required.15% coinsurance50% coinsuranceNot applicable15% coinsurance50% coinsurancePreauthorization may be required. 75 copayment pervisit; 15% coinsurance 75 copayment per visit;15% coinsuranceEmergency room copayment is waived ifadmitted directly to a hospital or facility asinpatient from the emergency room (but youwill pay an inpatient copayment).Tier 1: 0-30 day supply:10% coinsurance or 25, whichever is lessTier 2: 0-30 day supply:30% coinsurance or 75, whichever is lessIf you have outpatientsurgeryFacility fee (e.g., ambulatorysurgery center)Physician/surgeon feesEmergency room careIf you need immediatemedical attentionEmergency medicaltransportation20% coinsurance20% coinsuranceUrgent care15% coinsurance50% coinsuranceCoverage is not provided for air or waterambulance if ground ambulance wouldserve the same purpose. Ambulanceservices for personal or conveniencepurposes are notcovered.Not applicable*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 4 of 8
Common Medical EventIf you have a hospitalstayIf you need mentalhealth, behavioralhealth, or substanceabuse servicesIf you are pregnantServices You May NeedFacility fee (e.g., hospitalroom)What You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most) 200 copayment perday up to 600 per50% coinsurancemember per calendaryearLimitations, Exceptions, & OtherImportant InformationProvider must notify plan on admission.Physician/surgeon fees15% coinsurance50% coinsurancePreauthorization may be required.Outpatient services15% coinsurance50% coinsurancePreauthorization may be required. Nocoverage for marriage or family counseling.Inpatient services 200 copayment perday up to 600 permember per calendaryearProfessional services:15% coinsurance50% coinsurancePreauthorization required for inpatientadmissions. Provider must notify the plan fordetoxification, intensive outpatient program,and partial hospitalization.Office visits15% coinsurance50% coinsuranceChildbirth/deliveryprofessional services15% coinsurance50% coinsuranceChildbirth/delivery facilityservices 200 copayment perday up to 600 permember per calendaryear50% coinsuranceUltrasounds during pregnancy are limited toone in week 13 or earlier and one duringweeks 16-22 (additional may be coveredwhen medically necessary).Elective deliveries before 39 weeksgestation covered only if medicallynecessary.Elective deliveries before 39 weeksgestation covered only if medicallynecessary.Custodial care, maintenance care, andprivate duty or continuous care in theHome health care15% coinsurance50% coinsurancemember’s home are not covered.Inpatient: 200Coverage is limited to 60 inpatient days perIf you need helpcopayment per day upcalendar year for all therapies combinedrecovering or haveto 600 per memberand 60 outpatient visits per calendar yearother special healthRehabilitation services50% coinsuranceper calendar yearfor all therapies combined. InpatientneedsProfessional services:admissions for rehabilitation services mustbe preauthorized.15% coinsuranceHabilitation services50% coinsuranceCoverage includes neurodevelopmentalInpatient: 200*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 5 of 8
Common Medical EventServices You May NeedSkilled nursing careWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most)copayment per day upto 600 per memberper calendar yearProfessional services:15% coinsuranceInpatient: 200copayment per day upto 600 per member50% coinsuranceper calendar yearProfessional services:15% coinsuranceDurable medical equipment15% coinsurance50% coinsuranceHospice services 0 after deductible ismet50% coinsuranceChildren’s routine eye examIf your child needsdental or eye careChildren’s glasses or contactlensesChildren’s dental check-up 0 of the allowedamount 0 up to the allowedamount for one pair ofstandard lenses andframes per year; or 0 up to the allowedamount for a one-yearsupply of contact lensesin lieu of standardlenses and frames.Not coveredNot coveredNot coveredNot coveredLimitations, Exceptions, & OtherImportant Informationtherapy. Coverage is limited to 60 inpatientdays per calendar year for all therapiescombined and 60 outpatient visits percalendar year for all therapies combined.Preauthorization is required.Coverage is limited to 150 days percalendar year. Services must bepreauthorized.Foot orthotics are covered only forprevention of diabetic complications.Replacement of lost, stolen, or damageddurable medical equipment is not covered.Hospice coverage is limited to 6 months.Coverage for respite care is limited to 14visits per the patient’s lifetime.Not subject to deductible. Coverage forchildren under the age of 19. You pay 0 ofthe allowed amount when you see a VSPChoice network provider for one coveredpreventive eye exam with refraction orvisual analysis per calendar year.Not subject to the deductible. There is nocontact lens fitting fee. Coverage forchildren under the age of 19. Visioncoverage is provided by UMP, incollaboration with Regence Choice VisionPlan administered by Vision Service Plan(VSP).Not applicable*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 6 of 8
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan’s certificate of coverage for more information and a list of any other excludedservices.) Cosmetic services or supplies Medical foods or food supplements Infertility or fertility testing ortreatment after initial diagnosis Custodial care Medications for sexual dysfunction Maintenancecare Private duty or continuous care in the Dental care Marriage or family counseling Immunizations for travel or employmentmember’s home Massage therapy services when the Weight loss programs and drugsmassage therapist is not a network providerOther Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan’s certificate of coverage.) Acupuncture Hearing Aids Routine eye care (adult) Bariatric surgery Non-emergency care when traveling outside Routine foot care for certain medical Chiropractic carethe U.S.conditionsYour Rights to Continue Coverage: Other coverage options may be available to you too, including buying individual insurance coverage through the HealthInsurance Marketplace. For more information about the Marketplace, visit HealthCare.gov or call 1-800-318-2596.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your rights, look at the explanation of benefits you receive for that medical claim. Your plan’s certificate of coveragealso provides complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, orassistance, contact: UMP Customer Service at 1-888-849-3681 (medical benefits) (TRS: 711); Washington State Rx Services at 1-888-361-1611 (prescriptionbenefits) (TRS: 711). The Consumer Protection Division of the Office of the Insurance Commissioner (OIC) is currently designated by the U.S. Department of Healthand Human Services as the official ombudsman in the State of Washington for consumers who have questions or complaints about health care appeals. Consumersmay contact the OIC Consumer Hotline number at 1-800-562-6900.Does this plan provide Minimum Essential Coverage? Yes.If you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from therequirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? Yes.If your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.Language Access Services:[Spanish (Español): Para obtener asistencia en Español, llame al 1-888-849-3681 (TRS: 711)].[Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-888-849-3681 (TRS: 711)].[Chinese (中文): 如果需要中文的帮助, 请拨打这个号码 1-888-849-3681 (TRS: 711)].[Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-888-849-3681 (TRS: 711)].To see examples of how this plan might cover costs for a sample medical situation, see the next section.*For more information about limitations and exceptions, see the plan’s certificate of coverage at hca.wa.gov/ump-pebb-coc.Page 7 of 8
About these Coverage Examples:This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be differentdepending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts(deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you mightpay under different health plans. Please note these coverage examples are based on self-only coverage. Peg is Having a BabyManaging Joe’s Type 2 DiabetesMia’s Simple Fracture(9 months of in-network pre-natal care and ahospital delivery)(a year of routine in-network care of a wellcontrolled condition)(in-network emergency room visit and follow upcare)The plan’s overall deductibleSpecialist coinsuranceHospital (facility) copaymentOther coinsurance 12515% 20015% The plan’s overall deductibleSpecialist coinsuranceHospital (facility) copaymentOther coinsurance 12515% 015% The plan’s overall deductibleSpecialist coinsuranceHospital (facility) copaymentOther coinsurance 12515% 7515%This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility ServicesDiagnostic tests (ultrasounds and blood work)Specialist visit (anesthesia)This EXAMPLE event includes services like:Primary care physician office visits (includingdisease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (insulin pumps andinsulin pump supplies)This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy)Total Example CostTotal Example CostTotal Example Cost 12,840 7,460 2,010In this example, Peg would pay:Cost SharingDeductibles 125In this example, Joe would pay:Cost SharingDeductiblesCopayments 200Copayments 0Copayments 75Coinsurance 1,675Coinsurance 1,679Coinsurance 282 60 2,060What isn’t coveredLimits or exclusionsThe total Joe would pay is 255 2,059What isn’t coveredLimits or exclusionsThe total Mia would pay is 0 482What isn’t coveredLimits or exclusionsThe total Peg would pay is 125In this example, Mia would pay:Cost SharingDeductibles 125The plan would be responsible for the other costs of these EXAMPLE covered services.Page 8 of 8
Page 1 of 8 Summary of Benefits and Coverage: What this Plan Covers & What You Pay for Covered Services Coverage Period: 01/01/2021 - 12/31/2021 Uniform Medical Plan (UMP) Plus-UW Medicine Accountable Care Network (ACN) (PEBB) Coverage for: Individual/Family Plan Type: ACP Important Questions Answers Why This Matters: What is the overall