Transcription
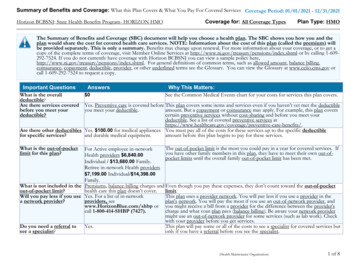
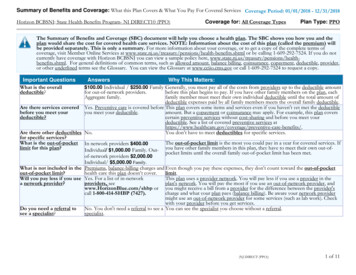
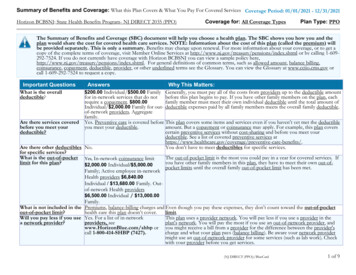
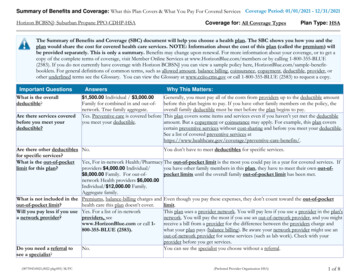
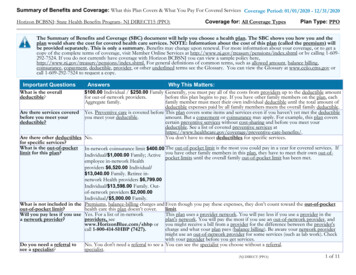
Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: 01/01/2020 - 12/31/2020Horizon BCBSNJ: State Health Benefits Program- NJ DIRECT15 (PPO)Coverage for: All Coverage TypesPlan Type: PPOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and theplan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) willbe provided separately. This is only a summary. Benefits may change upon renewal. For more information about your coverage, or to get acopy of the complete terms of coverage, visit Member Online Services at http://www.nj.gov/treasury/pensions/index.shtml or by calling 1-609292-7524. If you do not currently have coverage with Horizon BCBSNJ you can view a sample policy ml. For general definitions of common terms, such as allowed amount, balance billing,coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at www.cciio.cms.gov orcall 1-609-292-7524 to request a copy.Important QuestionsWhat is the overalldeductible?Answers 100.00 Individual / 250.00 Familyfor out-of-network providers.Aggregate family.Why This Matters:Generally, you must pay all of the costs from providers up to the deductible amountbefore this plan begins to pay. If you have other family members on the plan, eachfamily member must meet their own individual deductible until the total amount ofdeductible expenses paid by all family members meets the overall family deductible.Are there services covered Yes. Preventive care is covered before This plan covers some items and services even if you haven’t yet met the deductiblebefore you meet youryou meet your deductible.amount. But a copayment or coinsurance may apply. For example, this plan coversdeductible?certain preventive services without cost-sharing and before you meet yourdeductible. See a list of covered preventive services are-benefits/.Are there other deductibles No.You don’t have to meet deductibles for specific services.for specific services?What is the out-of-pocket In-network coinsurance limit 400.00 The out-of-pocket limit is the most you could pay in a year for covered services. Iflimit for this plan?Individual/ 1,000.00 Family; Active you have other family members in this plan, they have to meet their own out-ofpocket limits until the overall family out-of-pocket limit has been met.employee in-network Healthproviders 6,520.00 Individual/ 13,040.00 Family. Retiree innetwork Health providers 6,799.00Individual/ 13,598.00 Family. Outof-network providers 2,000.00Individual/ 5,000.00 Family.What is not included in the Premiums, balance-billing charges and Even though you pay these expenses, they don’t count toward the out-of-pocketout-of-pocket limit?health care this plan doesn’t cover.limit.Will you pay less if you use Yes. For a list of in-networkThis plan uses a provider network. You will pay less if you use a provider in thea network provider?providers, seeplan's network. You will pay the most if you use an out-of-network provider, andwww.HorizonBlue.com/shbp or you might receive a bill from a provider for the difference between the provider'scall 1-800-414-SHBP (7427).charge and what your plan pays (balance billing). Be aware your network providermight use an out-of-network provider for some services (such as lab work). Checkwith your provider before you get services.Do you need a referral toNo. You don't need a referral to see a You can see the specialist you choose without a referral.see a specialist?specialist.(NJ DIRECT (PPO))1 of 11
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.CommonMedical EventServices You May NeedIf you visit a health Primary care visit to treat ancare provider’s office injury or illnessor clinicSpecialist visitPreventivecare/screening/immunizationWhat You Will PayNetwork ProviderOut-of-Network(You will pay theProvider(You will payleast)the most) 15.00 Copayment per30% Coinsurance.visit. 15.00 Copayment per30% Coinsurance.visit; Specialist.No Charge.If you have a testNot Covered.Diagnostic test (x-ray, bloodNo Charge.30% Coinsurance.work)Imaging (CT/PET scans, MRIs) No Charge.30% Coinsurance.If you need drugs to Generic drugstreat your illness orPreferred brand drugsconditionNon-preferred brand drugsMore information aboutprescription drugSee separate Prescription Drug Plan SBCcoverage is availablethrough your employer. Specialty drugsIf you haveFacility fee (e.g., ambulatoryNo Charge.30% Coinsurance.outpatient surgerysurgery center)Physician/surgeon feesNo Charge.30% Coinsurance.If you needimmediate medicalattentionEmergency room care 100.00 Copayment pervisit for OutpatientHospital.Emergency medicaltransportation10% Coinsurance.Limitations, Exceptions, & OtherImportant InformationOut-of-network coverage forchiropractic and acupuncture servicesis limited to no more than 35 a visitfor chiropractic and 60 a visit foracupuncture or 75% of the in networkcost per visit, whichever is less?One per calendar year. You may haveto pay for services that aren'tpreventive. Ask your provider if theservices needed are preventive. Thencheck what your plan will pay for.noneRequires pre-approval.nonenone30% Coinsurance for out-of-networkanesthesia. 100.00 Copayment per 50 copay/visit for physician referralsvisit for Outpatientor pediatric (under age 19) ER visits;Hospital. Deductible doesand if admitted within 24 hours, thenot apply.copayment is waived. Payment at thein-network level applies only to trueMedical Emergencies & AccidentalInjuries.30% Coinsurance.Limited to local emergency transport tothe nearest facility equipped to treat theemergency condition.2 of 11
CommonMedical EventServices You May NeedUrgent careIf you have ahospital stayIf you need mentalhealth, behavioralhealth, or substanceabuse servicesIf you need helprecovering or haveother special healthneeds 15.00 Copayment pervisit.none30% Coinsurance.Facility fee (e.g., hospital room) No Charge.30% Coinsurance.Requires pre-approval. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.Physician/surgeon feesNo Charge.30% Coinsurance.Requires pre-approval. 30%Coinsurance for out-of-networkanesthesia.Outpatient servicesNo Charge for Outpatient 30% Coinsurance.Hospital. 15.00 Copayment perOffice visit for MentalHealth and BehavioralHealth. No Charge forSubstance abuse Officevisit.No Charge.30% Coinsurance.Inpatient servicesIf you are pregnantWhat You Will PayLimitations, Exceptions, & OtherNetwork ProviderOut-of-NetworkImportant Information(You will pay theProvider(You will payleast)the most)Office visits 15.00 Copayment per visit 30% Coinsurance.for Office.Some specialty outpatient servicesrequire pre-approval.Requires pre-approval. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.Cost sharing does not apply forpreventive services. Maternity care mayinclude tests and services describedelsewhere in the SBC (i.e. Ultrasound.)Childbirth/delivery professional No Charge.servicesChildbirth/delivery facilityNo Charge.services30% Coinsurance.30% Coinsurance.Home health careNo Charge.30% Coinsurance.Requires pre-approval. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.Requires pre-approval.Rehabilitation servicesNo Charge for Inpatient 30% Coinsurance.and Outpatient Facility. 15.00 Copayment per visitfor Office.No Charge for Inpatient30% Coinsurance.and Outpatient Facility.Habilitation servicesnoneRequires pre-approval. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.3 of 11
CommonMedical EventServices You May NeedSkilled nursing careIf your child needsdental or eye careWhat You Will PayLimitations, Exceptions, & OtherNetwork ProviderOut-of-NetworkImportant Information(You will pay theProvider(You will payleast)the most) 15.00 Copayment per visitfor Office.No Charge.Requires pre-approval. Limited to 12030% Coinsurance.days in-network and 60 out-of-networkfacility days for a combined maximumof 120 days per calendar year. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.Durable medical equipment10% Coinsurance.30% Coinsurance.Requires pre-approval for all rentalsand some purchases.Hospice servicesNo Charge.30% Coinsurance.Children’s eye exam 15.00 Copayment pervisit.Not Covered.Not Covered.Not Covered.Requires pre-approval. There is aseparate 200 deductible per inpatientstay for out-of-network facilities.Coverage is limited to 1 visit.Children’s glassesChildren’s dental check-upNot Covered.Not Covered.nonenone4 of 11
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excludedservices.) Cosmetic Surgery Long Term Care Routine foot care Dental care (Adult) Private-duty nursing Weight Loss ProgramsOther Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture (for pain management only) Hearing Aids (Only covered for members age15 or younger) Bariatric surgery (requires pre-approval) Infertility treatment (requires pre-approval) Chiropractic care (limited to 30 visits/year) Most coverage provided outside the UnitedStates. (Subject to deductible/coinsuranceand balance billing.) Non-emergency care when traveling outsidethe U.S. (Subject to deductible/coinsuranceand balance billing.)Routine eye care (Adult)5 of 11
Your Rights to Continue Coverage:There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: the plan at 1-800-4147427 (SHBP), the Department of Health and Human Services, Center for Consumer Information and Insurance Oversight, at 1-877-267-2323 x61565 orwww.cciio.cms.gov, or the U.S. Department of Labor, Employee Benefits Security Administration at 1-866-444-3272 or www.dol.gov/ebsa. Othercoverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace. For moreinformation about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596.Your Grievance and Appeals Rights:There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a grievance or appeal. For moreinformation about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also provide completeinformation to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance,contact: Horizon Blue Cross Blue Shield of New Jersey Member Services at 1-800-414-SHBP (7427). You may also contact the Department of Labor’sEmployee Benefits Security Administration at 1-866-444-EBSA (3272) or www.dol.gov/ebda/healthreform.Does this plan provide Minimum Essential Coverage? YesIf you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for anexemption from the requirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? YesIf your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through ------To see examples of how this plan might cover costs for a sample medical situation, see the next ---6 of 11
About these Coverage Examples:This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs willbe different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the costsharing amounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to comparethe portion of costs you might pay under different health plans. Please note these coverage examples are based on self-only coverage.Peg is Having a Baby(9 months of in-network pre-natal careand a hospital delivery) The plan’s overall deductibleSpecialist CopaymentHospital (facility) CoinsuranceOther Coinsurance 0.00 15.000%10%This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility ServicesDiagnostic tests (ultrasounds and blood work)Specialist visit (anesthesia)Total Example CostIn this example, Peg would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Peg would pay is 12,800.00 0.00 20.00 0.00 100.00 120.00Managing Joe’s type 2 Diabetes(a year of routine in-network care of awell-controlled condition) The plan’s overall deductibleSpecialist CopaymentHospital (facility) CoinsuranceOther Coinsurance 0.00 15.000%10%This EXAMPLE event includes services like:Primary care physician office visits (includingdisease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)Total Example CostIn this example, Joe would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Joe would pay is 7,400.00 0.00 150.00 0.00 6,040.00 6,190.00Mia’s Simple Fracture(in-network emergency room visit andfollow up care) The plan’s overall deductibleSpecialist CopaymentHospital (facility) CoinsuranceOther Coinsurance 0.00 15.000%10%This EXAMPLE event includes services like:Emergency room care (including medical supplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy)Total Example Cost 1,900.00In this example, Mia would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Mia would pay is 0.00 110.00 80.00 0.00 190.00Please note that some of the Limits or Exclusions listedabove may be covered under the Prescription Plan.This plan has other deductibles for specific services included in this coverage example. See "Are there other deductibles for specific services?" row above.The plan would be responsible for the other costs of these EXAMPLE covered services.7 of 11
8 of 11
9 of 11
10 of 11
11 of 11
Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: 01/01/2020 - 12/31/2020 Horizon BCBSNJ: State Health Benefits Program- NJ DIRECT15 (PPO) Coverage for: All Coverage Types Plan Type: PPO (NJ DIRECT (PPO)) 1 of 11 The Summary of Benefits and Coverage (SBC) document will help you choose a health plan.