Transcription
An Original StudyTalar Neck Fractures Treated With ClosedReduction and Percutaneous ScrewFixation: A Case SeriesMichael L. Fernandez, MD, Allison M. Wade, MD, Michael Dabbah, MD, and Paul J. Juliano, MDAbstractTalus fractures are relatively rare injuries, accounting forapproximately 3% of all foot fractures. Fractures of thetalar neck account for almost 50% of all talus fractures.Diagnosis and treatment of these fractures play animportant role in patients’ outcomes. Treatment of talarneck fractures has slowly evolved from closed treatment to open reduction and internal fixation. Treatmentof type I and type II talar neck fractures is debatedin the orthopedic community. Choosing which treatment to perform depends on injury severity, associated injuries, and surgeon experience and preference.In this article, we report on our retrospective reviewof all talar neck fractures treated with closed reductionand percutaneous fixation between 1996 and 2001 at thePennsylvania State University Milton S. Hershey MedicalCenter.produced by an axial force directed to the plantar surfaceof the foot just distal to the talus with the ankle in theneutral position. In addition, Hawkins4 and Canale andKelly10 both noted a significant rotational componentassociated with talar neck fractures. Historically, thesehigh-energy fractures were noted in plane crashes duringthe era when pilots controlled rudders with their feet.The sudden deceleration of a plane crash combined withthe position of the pilot’s feet resulted in hyperdorsiflexion of the foot.1,2,8 Now, high-speed motor crashes andfalls from a significant height consistently reproduce themechanisms that cause talar neck fractures.A trauma patient who presents after a motor vehicleaccident or fall from a height and reports foot and/orankle pain must undergo a thorough physical examination, including radiography. Standard anteroposte-Diagnosis and treatment of talar neck fractureshave always been challenging. The mechanismof injury for these fractures has often beendescribed as a combination of axial compression forces and dorsiflexion at the ankle.1-8 Petersonand colleagues9 showed that talar neck fractures wereDr. Fernandez is former Resident, Foot and Ankle Department,Department of Orthopaedics and Rehabilitation, Penn StateMilton S. Hershey Medical Center, PennsylvaniaState University College of Medicine, Hershey, Pennsylvania.Dr. Fernandez currently is in private practice at the OrthopaedicInstitute of Harrisburg, Harrisburg, Pennsylvania.Dr. Wade is Fellow, Foot and Ankle Department, Departmentof Orthopaedics and Rehabilitation, Penn State Milton S.Hershey Medical Center, Pennsylvania State University Collegeof Medicine, Hershey, Pennsylvania.Dr. Dabbah is in private practice at Orthopaedics Associates ofFrederick, Frederick, Maryland.Dr. Juliano is Professor, Vice Chairman, Residency Director, andChief, Foot and Ankle Division, and Foot and Ankle FellowshipDirector, Department of Orthopaedics and Rehabilitation, PennState Milton S. Hershey Medical Center, Pennsylvania StateUniversity College of Medicine, Hershey, Pennsylvania.Address correspondence to: Paul J. Juliano, MD, Departmentof Orthopaedics and Rehabilitation, Penn State Milton S.Hershey Medical Center, Pennsylvania State University Collegeof Medicine, PO Box 850, MC H089, 500 University Dr, Hershey,PA 17033 (tel, 717-531-5638; fax, 717-531-7583; e-mail,pjuliano@hmc.psu.edu).Am J Orthop. 2011;40(2):72-77. Copyright 2011, QuadrantHealthCom, Inc. All rights reserved.72 The American Journal of Orthopedics Figure 1. (A) Lateral view of first 2.0 guide pin, inserted posterolaterally and extending through dorsum of foot. (B) Superiorview of 3-hole guide being used to insert second 2.0 guide pinlaterally and in direction reverse that of first pin. (C) Partiallythreaded 4.5-mm cannulated screw placed anterior to posterior,with second screw placed posterior to anterior.www.amjorthopedics.com
M. L. Fernandez et alABCFigure 2. Anteroposterior (A) and lateral (B) radiographs of rightHawkins type I talar neck fracture after percutaneous pinning.Postoperative anteroposterior (C) and lateral (D) radiographs.Drior, lateral, and oblique radiographs of the foot andankle should be obtained.8 In evaluation of the talusspecifically, it is also helpful to obtain the radiographicview described by Canale and Kelly10 in 1978. For theCanale view, the ankle is placed in maximum equinus, 15 of foot pronation, and the beam is directedcephalad 75 from horizontal. Although originallydescribed for evaluation of varus malunions of the talarneck, this view has become a helpful tool in radiographic evaluation of the acutely injured talus.10 It isa direct anteroposterior view of the talar neck. Whena severely comminuted fracture is being evaluated, orwhen plain radiographs are negative but there is a highclinical suspicion of a talar neck fracture, computedtomography (CT) may provide additional information.Studies have shown that the most accurate techniquesfor measuring talar neck displacement is CT.11 Toolanand Sangeorzan8 wrote that, when a CT scan has beenformatted 3-dimensionally, the anatomy of the talus iswww.amjorthopedics.commore easily identified. They added that evaluation ofvertical talar neck fractures is best performed in thetransverse and sagittal planes.The Hawkins classification system is often used todescribe talar neck fractures. Hawkins type I talarneck fractures, which are nondisplaced, can be treatedwith cast immobilization and non–weight-bearing for aperiod of approximately 6 to 12 weeks.10,12-15 In cases ofpolytrauma, anticipated nonadherence, and/or necessaryearly mobility, however, internal fixation is recommended.1 Hawkins type II talar neck fractures are displacedfractures with dislocation of the subtalar joint. The traditional suggestion for reducing this type of fracture andminimizing the risk for avascular necrosis (AVN) is thatany fracture with 2 mm of displacement or rotationaldeformity should undergo open reduction and internalfixation (ORIF).12,15 Hawkins type III injuries involvedisplacement and dislocation from the ankle and subtalar joints. These injuries are also traditionally treatedwith ORIF with or without a medial malleolar and/orfibular osteotomy.1 Type IV injuries, initially describedby Canale and Kelly,10 are displaced fractures associatedwith an ankle, subtalar, and talonavicular dislocation.16The talar body is vulnerable to AVN because of itsblood supply. The artery of the tarsal canal, whichbranches off the posterior tibial artery approximately1 cm proximal to the division of the medial and lateralplantar artery, is the most consistent blood supply to thetalar body. Unfortunately, it is susceptible to injury witha talar neck fracture because of its position within thetarsal canal. The deltoid artery, a branch of the arteryof the tarsal canal or posterior tibial artery, directlysupplies blood to the medial quarter to half of the talarFebruary 2011 73
Talar Neck Fractures Treated With Closed Reduction and Percutaneous Screw FixationTable I. Outcomes by Fracture TypeFracture TypeExcellentHawkins IHawkins IIHawkins 01also sustained ipsilateral talar body fracture.Table II. Patients With Hawkins Sign and Progression to Avascular NecrosisHawkins SignPresentAbsentTotalPatients (n)336body. Last, the artery of the sinus tarsi, which is vulnerable secondary to its size and location, supplies thelateral eighth to quarter of the talar body.15,17There is a correlation between severity of injury tothe talar neck and likelihood of progression to AVN.10The higher the injury grade, the higher the likelihood ofdisruption of the vascular anatomy of the talus, which,in turn, increases the risk for AVN. Type I injuries maydamage only one source of the talar blood supply andtherefore carry a small risk for AVN. Type II injuriesdamage possibly 2 of the 3 main sources of blood flow,and AVN may be noted in up to 40% of patients in thisgroup. In type III injuries, all 3 sources of blood flow tothe talus may be lost, and AVN may be noted in up to84% of patients in this group.2,10,16 In type IV injuries,100% of patients develop AVN.In 1970, Hawkins4 noted a subchondral lucencyin the talar dome approximately 6 to 8 weeks afterinjury—what came to be called the Hawkins sign. Thissubchondral lucency is a good prognostic indicator ofabsence of AVN. In a 1978 study, Canale and Kelly10substantiated the Hawkins sign. Of 23 patients whoshowed the Hawkins sign as early as 12 weeks afterinjury, only 1 developed AVN. The authors wrote thatthis subchondral lucency is indicative of hyperemia anddisuse osteopenia and that it correlates well with theimprobable progression of AVN in the talus but advisedthat a negative Hawkins sign does not necessarily meanAVN will develop. Although 20 of 26 patients (76.9%)with a negative Hawkins sign developed AVN, theremaining 6 (23.1%) did not. This study was conductedbefore use of magnetic resonance imaging (MRI).Studies conducted since then have shown MRI to be themost sensitive method for detecting AVN, though thesestudies involved the proximal femur, not the talus.18,19Although recent studies have indicated that posttraumatic subtalar arthritis is the most common complication after operative treatment,20 the most debilitating74 The American Journal of Orthopedics Progression to Avascular Necrosis (n)011complication is AVN. Our hypothesis focused on closedreduction and percutaneous fixation of talar neckfractures and whether use of this minimally invasiveapproach can lower rates of AVN and possibly improveclinical outcomes for patients who sustain talar neckfractures.In 2002, Fayazi and colleagues21 had suggested analternative to ORIF: closed reduction and percutaneous fixation. This procedure is performed to minimizefurther damage to soft-tissue structures, maintain and/or minimize disruption of the blood supply to the talus,and reduce surgery time.In this article, we review the outcomes of a series ofcases of talar neck fractures treated with closed reduction and percutaneous fixation at our institution.Materials and MethodsInstitutional review board approval was obtained toreview all cases of talar neck fracture treated between1996 and 2001 at our institution. Ten patients were identified in the operative cases database of Dr. Juliano, thesenior surgeon. With pediatric patients, open injuries, andHawkins type IV fractures excluded, 7 patients met ourreview criterion of having undergone closed reductionand percutaneous fixation of the talus. Of these 7 patients,4 had Hawkins type I injuries, 2 had Hawkins type II,and 1 had Hawkins type III. One patient with a type Ifracture was lost to follow-up, leaving 6 patients for thestudy. Radiographs and the Hawkins system were used toclassify all injuries. Each patient underwent closed reduction, and a transfixion pin was placed through the calcaneal tuberosity and attached to a traction bow. Reductionwas facilitated by placing the foot in plantarflexion andcarefully maneuvering the heel from varus to valgus withthe aid of the transfixion pin. Closed reduction of the1 Hawkins type III injury in this series was done with atechnique described by Baumhauer and Alvarez.13 All thepatients involved in this series underwent percutaneouswww.amjorthopedics.com
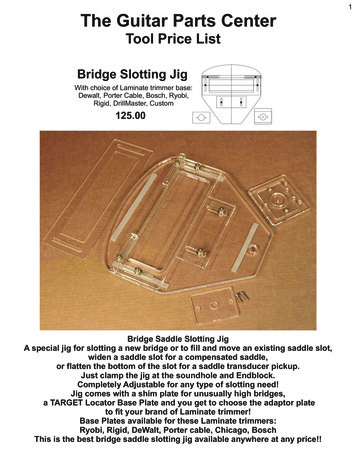
M. L. Fernandez et alTable III. Overview of All 6 PatientsAge atAssociatedPt Sex Injury, y DiagnosisInjuriesTime to SurgeryOperating Time, HospitalRoom, hminStay, Fair2 M21Hawkins type I, Right nondisplaced Motor vehicle7270250Positiveright footacetabular fracture accident: patientejectedSubtalararthritisExcellent3 F20Hawkins type I,right footMotor rNone(phoneinterview)ExcellentMotorcycleaccident: axial loadNoneExcellent1 M304 M30Hawkins type I, Noneright footRight ulnar styloidavulsion fracture,neck hematoma,sternal contusionHawkins type II, Noneright footMechanismof InjuryBicycle accident:25inversion-type injury59310502Followup, wk1232Positive5 F35Hawkins type II, Fracture of posterior Fall from 10 feet48722152NegativeAvascularPoorleft footmedial tuberclenecrosis,of left talar bodysubtalararthritis6 M56Hawkins type III, Right medialFall from 5 feet4.5125124NegativeSubtalarExcellentright footmalleolar fracturearthritisfixation of talar neck fractures as described by Fayazi andcolleagues.21 This procedure begins with a closed reduction attempt, as already described. Intraoperative fluoroscopy is used to check the adequacy of the reduction. In thecase of less than anatomical reduction, conversion to openreduction is necessary. When the reduction is satisfactory,a small incision is made on the posterolateral aspect ofthe heel anterior to the Achilles tendon and posterior tothe peroneal tendons. Blunt dissection is then continuedthrough the subcutaneous tissue to the talar dome. Underfluoroscopic guidance, a 2.0-mm guide wire is put slightlysuperior to the posterolateral talar tubercle and perpendicular to the fracture line. The guide wire is then movedin an anteromedial fashion and is advanced through thedorsum of the foot. After this, another 2.0-mm guide wireis placed parallel and lateral to the original wire in thereverse direction using an AO/ASIF (Arbeitsgemeinschaftfür Osteosynthesefragen/Association for the Study ofInternal Fixation) 3-hole guide. This second wire is placedthrough a small incision on the dorsum of the foot anteromedial to posterolateral through the talar neck. Next,a partially threaded 4.5-mm cannulated screw is placedanterior to posterior, and the second screw is placed posterior to anterior (Figure 1). After the incisions are closedwith 3-0 nylon, the patient is placed in a 3-sided coaptation splint.21 Figure 2 shows a radiographic view of thepercutaneous fixation.We used the Hawkins scoring system (as originallydescribed by Hawkins4) to evaluate 4 postoperative criteria: pain, limp, ankle range of motion (ROM), and subtalar ROM. In this system, the maximum number of pointsis 15. A patient with no pain is given 6 points; with painonly after fatigue, 3 points; with pain on walking, 0 point;www.amjorthopedics.comwith no limp, 3 points; with limp, 0 points. Ankle ROMand subtalar ROM are each rated on a 3-point scale: 3points for full ROM, 2 for partial ROM, 1 for joint fusion,and 0 for fixed deformity. Scores of 13 to 15 were considered excellent; 10 to 12, good; 7 to 9, fair; and 6 or less,poor. Excellent and good results were deemed satisfactory.For the 6 patients who were followed up, presence ofHawkins sign was assessed 6 to 8 weeks after injury, assuggested by Hawkins.4 In addition, for this investigation, a diagnosis of posttraumatic subtalar arthritiswas made when decreased ROM and/or pain was notedat the subtalar joint in association with degenerativechanges on radiographs.ResultsMean age at time of injury was 32 years (range, 20-56years), mean time between injury and fixation was 29.6hours (range, 4.5-72 hours), mean surgery time was 102minutes (range, 70-147 minutes), mean hospital stay was1.5 days (range, 0-2 days), and mean follow-up was 81.5weeks. Five patients had associated fractures—an openHawkins II talar neck fracture on the contralateral foot,an ipsilateral talar body fracture, an ipsilateral medialmalleolar fracture, an occipital skull fracture, an ipsilateralacetabular fracture, and an ulnar styloid avulsion fracture.Of the 6 patients, 4 had excellent results, 1 had a fairresult, and 1 had a poor result (Table I). The 4 patientswith excellent results did not develop AVN, but 2 ofthese 4 patients developed subtalar arthritis. Of the 3type I patients, 2 had excellent results, and 1 had a fairresult. Of the 2 type II patients, 1 had an excellent result,and 1 had a poor result. The 1 type III patient had anexcellent result.February 2011 7573
Talar Neck Fractures Treated With Closed Reduction and Percutaneous Screw FixationThe type II patient with a poor result also had anipsilateral talar body fracture. This patient subsequentlydeveloped AVN and subtalar arthritis and was treatedwith steroid injections and ultimately with subtalararthrodesis. Two other patients (type I, type III) alsodeveloped subtalar arthritis.A Hawkins sign was present in 3 of the 6 patientsexamined 6 to 8 weeks after injury. Of these 3 patients,none developed AVN. Of the 3 patients without aHawkins sign, 1 had a type II fracture and developedradiographic AVN but did not progress to talar domecollapse (Table II).Table III is an overview of all 6 patients who werefollowed up. Data include type of injury and results.The only poor result was for a patient who sustained atalar body fracture in addition to the talar neck fracture.Three patients had posttraumatic arthritis and pain.One patient was diagnosed with radiographic AVN butdid not develop talar dome collapse.DiscussionFractures of the talar neck are associated with numerouscomplications, including AVN, malunion, nonunion, andposttraumatic arthritis. ORIF is advocated for displacedtalar neck fractures.13,22,23 Canale23 and Hawkins4 agreedthat type III and type IV talar neck fractures shouldundergo ORIF. For type I and type II, however, treatmentstill depends on injury severity, associated injuries, andsurgeon experience and preference.The blood supply to the talus has been reviewed byseveral authors, including Baumhauer and Alvarez.13This supply is extremely vulnerable in talar neck fractures. Most of the vessels that supply the talus enterthe head and supply the body in a retrograde manner.With this configuration, fractures through the talarneck can result in AVN of the talar dome and body.Owing to the unique blood supply of the talus, the riskof AVN is proportional to injury severity. In type IIIand type IV fractures, the only remaining blood supply to the dome may be through the deltoid ligament.Therefore, it is important to try to preserve the soft-tissueenvelope around the talus. As a result, our hypothesiswas that closed reduction and percutaneous fixation oftalar neck fractures can lower rates of AVN and possibly improve clinical outcomes for patients with talarneck fractures.Most Hawkins type I talar neck fractures have goodclinical outcomes with low risk of AVN and no reportsof talar malunion.15 In type II fractures, unsatisfactoryresults have been reported in up to 60% of cases, AVN inup to 71% of cases, and arthritis in up to 64% of cases.Compared with type I and type II fractures, type IIIfractures have a less favorable prognosis, and complications are abundant.16 Fifty percent of these fracturesmay be open, which increases the risk for talar bodyinfections. Unsatisfactory results have been reported inup to 91% of these cases and AVN in up to 100%.4 7674 TheThe AmericanAmerican JournalJournal ofof OrthopedicsOrthopedics Several factors are involved in the unsatisfactory outcomes for these injuries. First, the insult to the talus surfaceat time of injury significantly harms the articular cartilage,and the damage may result in posttraumatic arthritis.16Second, when ORIF is warranted, dissection of surroundingsoft tissues causes further disruption of an already compromised blood supply,21 which may contribute to developmentof AVN in the talus. Third, a delay in treatment may increasethe risk for subsequent AVN,8,12,15 though recent reportshave suggested that time to reduction does not predict outcome, union, or development of AVN.20,24The purpose of this retrospective study was to determinethe rates of AVN and overall clinical outcome in patientswho underwent closed reduction and percutaneous fixation for talar neck fractures. We reviewed the results of 6such patients. Use of the Hawkins scoring system revealedexcellent scores (13-15 points) in 4 (67%) of these patients.Canale and Kelly10 reported a Hawkins foot score of 59%(a satisfactory result), but they included patients whounderwent both ORIF and closed reduction.Complications of talar neck fractures are well documented.4,10,13,15,23,25 Grob and colleagues26 reported a37% incidence of posttraumatic subtalar arthritis in aseries of 41 patients, Canale and Kelly10 and Canale23reported a 52% incidence of AVN, Lorentzen and colleagues27 reported a 65% incidence of subtalar arthritis(mean follow-up, 22 months), and Lindvall and colleagues20 reported a 100% incidence of radiographic posttraumatic arthritis involving at least the subtalar joint. Inthe present study, we found a 50% incidence of subtalararthritis and a 17% rate of AVN at a mean follow-up ( 20months) similar to that of Lorentzen and colleagues.27Our rates of subtalar arthritis and AVN are slightly lowerthan those in the literature and may be the result of oursmall patient population and relatively short follow-up.Small population and short follow-up are valid criticisms of this study, but we should point out that the meanfollow-up for the 4 patients with satisfactory results was81.5 weeks. This outcome gives value to the study in thatadequate time was allowed in which potential complications could be documented in these patients. In addition,the patient with a fair outcome had a follow-up of only12 weeks. We could argue that, with a longer follow-up,the Hawkins score for this patient might have been higher(ie, the outcome might have been better). Finally, theseinjuries are rare and are often associated with other injuries that may necessitate ORIF, thus removing the optionof percutaneous fixation. However, we believe that closedreduction and percutaneous fixation preserves the softtissue around the talus and thereby lowers the incidenceof radiographic AVN.Nevertheless, more studies are warranted, particularlystudies with a larger patient population. Furthermore, acomparison of talar neck fractures treated with ORIFand talar neck fractures treated with closed reductionand percutaneous fixation in the same patient population would be valuable. Finally, time to reduction maywww.amjorthopedics.comwww.amjorthopedics.com
M. L. Fernandez et albe an important predictor of functional outcome andcould be included in future studies.Authors’ Disclosure StatementThe authors report no actual or potential conflict of interest in relation to this article.References1. Anderson HG. The Medical and Surgical Aspects of Aviation. London, UK:Oxford Medical; 1919.2. Coltart WD. Aviator’s astragalus. J Bone Joint Surg Br. 1952;34(4):545566.3. Gibson A, Inkster RG. Fractures of the talus. Can Med Assoc J.1934;31(4):357-362.4. Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am.1970;52(5):991-1002.5. Jensenius H. Fractures of the astragulus. Acta Orthop Scand.1950;19(1):195-209.6. Kenwright J, Taylor RG. Major injuries of the talus. J Bone Joint Surg Br.1970;52(1):36-48.7. Swanson TV, Bray TJ, Holmes GB Jr. Fractures of the talar neck. J BoneJoint Surg Am. 1992;74(4):544-551.8. Toolan BC, Sangeorzan BJ. The Traumatized Foot: Fractures of the Talus.AAOS Monograph Series; 2001:1-11.9. Peterson L, Romanus B, Dahlberg E. Fracture of the collum tali—an experimental study. J Biomech. 1976;9(4):277-279.10. Canale ST, Kelly FB Jr. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J Bone Joint Surg Am. 1978;60(2):143-156.11. Chan G, Sanders DW, Yuan X, Jenkinson RJ, Willits K. Clinical accuracy of imaging techniques for talar neck malunion. J Orthop Trauma.2008;22(6):415-418.12. Adelaar RS. Fractures of the talus. Instr Course Lect. 1990;39:147-156.13. Baumhauer JF, Alvarez RG. Controversies in treating talus fractures. OrthopClin North Am. 1995;26(2):335-351.14. DeLee JC. Fractures and dislocations of the foot. In: Mann RA, CoughlinMJ, eds. Surgery of the Foot and Ankle. 6th ed. St. Louis, MO: Mosby;1993:1539-1600.15. Higgins TF, Baumgaertner MR. Diagnosis and treatment of fracturesof the talus: a comprehensive review of the literature. Foot Ankle Int.1999;20(9):595-605.16. Berlet GC, Lee TH, Massa EG. Talar neck fractures. Orthop Clin North Am.2001;32(1):53-64.17. Mulfinger GL, Trueta J. The blood supply of the talus. J Bone Joint Surg Br.1970;52(1):160-167.18. Mitchell MD, Kundel HL, Steinberg ME, Kressel HY, Alavi A, Axel L.Avascular necrosis of the hip: comparison of MR, CT, and scintigraphy. AJRAm J Roentgenol. 1986;147(1):67-71.19. Henderson RC. Posttraumatic necrosis of the talus: the Hawkins signversus magnetic resonance imaging. J Orthop Trauma. 1991;5(1):96-99.20. Lindvall E, Haidukewych G, DiPasquale T, Herscovici D Jr, Sanders R. Openreduction and stable fixation of isolated, displaced talar neck and bodyfractures. J Bone Joint Surg Am. 2004;86(10):2229-2234.21. Fayazi AH, Reid JS, Juliano PJ. Percutaneous pinning of talar neck fractures. Am J Orthop. 2002;31(2):76-78.22. Günal I, Atilla S, Araç S, Gürsoy Y, Karagözlu H. A new technique oftalectomy for severe fracture-dislocation of the talus. J Bone Joint Surg Br.1993;75(1):69-71.23. Canale ST. Fractures of the neck of the talus. Orthopedics. 1990;13(10):1105-1115.24. Vallier HA, Nork SE, Barei DP, Benirschke SK, Sangeorzan BJ. Talar neck fractures: results and outcomes. J Bone Joint Surg Am. 2004;86(8):1616-1624.25. Daniels TR, Smith JW. Foot fellow’s review: Talar neck fractures. Foot Ankle.1993;14(4):225-234.26. Grob D, Simpson LA, Weber BG, Bray T. Operative treatment of displacedtalus fractures. Clin Orthop. 1985;(199):88-96.27. Lorentzen JE, Christensen SB, Krogsoe O, Sneppen O. Fractures of theneck of the talus. Acta Orthop Scand. 1977;48(1):115-120.This paper will be judged for the Resident Writer’s Award.Did You Know ?Celebrating40Y ears ofThe American Journal of Orthopedicswas born as Orthopaedic ReviewThe American Journal of Orthopedicsand Industry Innovationin 1971.“Congratulations to The American Journal of Orthopedics on your 40thAnniversary! I’ve had the pleasure of being involved with this journal for over 15years (almost 40% of its existence!). I still remember when the journal changedits name from Orthopaedic Review. I must say, with that name change came a farmore rigorous peer review process and the journal really gained legitimacy. Thequality and breadth of original studies, reviews, and supplements that have beenpublished in The American Journal of Orthopedics over the last 10 years havegrown so, making our service on the Editorial Board both a challenge and a joy.Working with the editorial staff and colleagues at the journal has been a realpleasure. Their level of enthusiasm, commitment, and professionalism is top tierand I look forward to the next 15 years!”—Jess H. Lonner, MDAssociate Editor, The American Journal of OrthopedicsDirector, Knee Replacement SurgeryPennsylvania Hospital, Philadelphiawww.amjorthopedics.comFebruary 2011 7377
Department of Orthopaedics and Rehabilitation, Penn State Milton S. Hershey Medical Center, Pennsylvania State University College of Medicine, Hershey, Pennsylvania. Dr. Fernandez currently is in private practice at the Orthopaedic Institute of Harrisburg, Harrisburg, Pennsylvania. Dr. Wade is Fellow, Foot and Ankle Department, Department