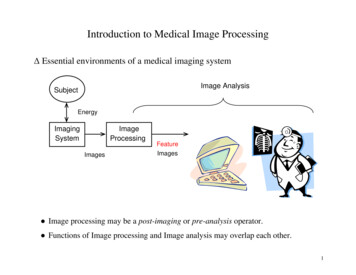
Transcription
www.clinicalimagingscience.orgJournal of Clinical Imaging ScienceNeuroradiology/Head and Neck Imaging Review ArticleImaging features of cartilaginous tumors of the head andneckPattana Wangaryattawanich1, Mohit Agarwal2, Tanya Rath3Department of Radiology, Division of Neuroradiology, University of Washington School of Medicine, Seattle, Washington, 2Department of Radiology,Medical College of Wisconsin, Milwaukee, Wisconsin, 3Department of Radiology, Mayo Clinic Arizona, Phoenix, Arizona, United States.1ABSTRACT*Corresponding author:Pattana Wangaryattawanich,Department of Radiology,Division of Neuroradiology,University of WashingtonSchool of Medicine, Seattle,Washington, United States.There is a wide spectrum of head and neck cartilaginous lesions which include both neoplastic and nonneoplastic processes. Cartilaginous tumors of the head and neck are uncommon, posing a diagnostic challenge.Benign cartilaginous tumors that may occur in the head and neck include chondroma, chondroblastoma,chondromyxoid fibroma, osteochondroma, and synovial chondromatosis. Chondromesenchymal hamartomais a rare non-neoplastic cartilaginous lesion that is included for the 1first time in the new WHO classificationand radiologically can mimic a tumor. Malignant cartilaginous tumors include chondrosarcoma and chondroidvariant of chordoma. Characteristic tumor locations, internal chondroid matrix calcification, and typical T2hyperintense signal secondary to high-water content within the extracellular matrix of the hyaline cartilage areuseful imaging features that narrow the differential diagnosis and help in diagnosing these diseases. This articlepresents a narrative review of the anatomy of the head and neck cartilaginous structures, discusses the currentknowledge and imaging spectrum of benign and malignant cartilaginous tumors and tumor-like lesions of thehead and neck.pattanaw@uw.eduKeywords: Cartilage, Cartilaginous lesions, Cartilaginous tumors, Chondroid, Head and neckReceived : 01 October 2021Accepted : 18 November 2021Published : 04 December 2021DOI10.25259/JCIS 186 2021Quick Response Code:INTRODUCTIONRadiologic diagnosis of cartilaginous tumors of the head and neck can be challenging due totheir rarity.[1] Their imaging appearance may overlap with other pathologies in the same location,further adding to the diagnostic dilemma. Thus, an understanding of the anatomy of head andneck cartilaginous structures is critical to correctly identifying the spectrum of cartilaginouslesions occurring in the head and neck. This review article describes the anatomy of the headand neck cartilaginous structures and radiologic features of benign and malignant cartilaginoustumors of the head and neck.ANATOMY OF THE CARTILAGINOUS STRUCTURES OF THE HEAD ANDNECKCartilage is an avascular connective tissue that plays a pivotal role in the growth and developmentof the human skeleton and histologically is composed of specialized cells, called chondrocytes.Chondrocytes can synthesize and secrete different components of the extracellular matrix(ECM), such as collagens, proteoglycans, and glycoprotein, which provide tensile strength and is is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows othersto remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms. 2021 Published by Scientific Scholar on behalf of Journal of Clinical Imaging ScienceJournal of Clinical Imaging Science 2021 11(66) 1
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckflexibility to tissue.[2,3] The perichondrium is a thin fibrousmembrane covering the external surface of the cartilage andcontaining superficial blood vessels. These vessels providenutrition to the cartilage by means of diffusion.[3]In humans, there are three main types of cartilage: Hyalinecartilage, elastic cartilage, and fibrocartilage, each ofwhich has different types and proportion of collagens andproteoglycans.[2] Hyaline cartilage is the most abundantcartilage in the human body, found primarily at the articularsurfaces of the synovial joints and at the epiphyseal platesof long bones. It facilitates joint movement and, in the headand neck region, is present at the skull base, within thenasal septum, the laryngeal cartilages, and in the trachealrings.[2] Ossification of the laryngeal cartilages increaseswith advancing age [Figure 1]. Male laryngeal cartilagestend to ossify to a greater extent compared to females.[4,5]Nonuniform ossification of the laryngeal cartilages is one ofthe pitfalls in evaluating cartilaginous invasion in patientswith laryngeal cancer. It is very important to be familiar withthis normal variation to avoid over staging of tumors.[6]Elastic cartilage, as the name implies, has high elasticity dueto the elastin fibers. In the head and neck, elastic cartilage ispredominantly found in the epiglottis, pinna of the externalear, external auditory canal, and the eustachian tube.[2] Unlikethe hyaline cartilage which forms the thyroid, cricoid andarytenoid cartilages, the elastic cartilage of the epiglottis doesnot undergo ossification with age.[7] Fibrocartilage is a poorlyvascularized tissue composed of fibroblasts and chondrocytes.It has a high density of collagen Type I which provides itshigh tensile strength.[8,9] It is predominantly found at the sitesof ligamentous and tendinous attachments, intervertebraldiscs, symphyses, synchondroses, and menisci.[8,9] In the headand neck region, fibrocartilage is found in the articular discand articular surfaces of the temporomandibular joint, aswell as spheno-petrosal and petro-occipital synchondroses atthe skull base.[8] Embryonic remnants of cartilaginous matrixwithin these synchondroses can be origins of cartilaginoustumors in the skull base.[10] [Table 1] summarizes the typesof cartilage and related cartilaginous structures in the headand neck.IMAGING FEATURES OF CARTILAGINOUSTUMORS IN THE HEAD AND NECKThe 2017 4th edition of the WHO classification of head andneck tumors is the most updated pathologic classification ofhead and neck tumors and tumor-like conditions.[11] Benigncartilaginous tumors that may occur in the head and neckinclude chondroma (aka enchondroma), chondroblastoma,chondromyxoid fibroma (CMF), osteochondroma, andsynovial chondromatosis. Chondromesenchymal hamartomais a rare non-neoplastic cartilaginous lesion that is includedfor the 1st time in the new WHO classification[12] and isJournal of Clinical Imaging Science 2021 11(66) 2abFigure 1: Physiologic ossification of the thyroid cartilage. Axialcontrast-enhanced neck CT in soft tissue window of a 15-year-oldboy (a) and a 41-year-old man (b) show physiologic ossificationof the thyroid cartilage which increases with age. Note absence ofossification of the thyroid cartilage (arrow) on (a) and non-uniformossification of the thyroid cartilage (arrow) on (b).Table 1: Head and neck structures derived from each type ofcartilage.Types of cartilage Head and Neck StructuresHyaline cartilageElastic cartilageFibrocartilageSkull base, nasal septum, larynx, tracheaEpiglottis, external ear (that is, ear pinna andouter cartilaginous portion), the eustachiantube of the middle earIntervertebral disks of the spine,articular disc and articular surface of thetemporomandibular joint, spheno-petrosaland petro-occipital synchondroses of theskull baseincluded in this discussion, because it can mimic a tumor.Malignant cartilaginous tumors include chondrosarcomaand chondroid variant of chordoma. [Table 2] lists thecartilaginous tumors and tumor-like lesions affecting thehead and neck and their characteristic imaging features.In general, cartilaginous tumors with well-differentiatedchondroid matrix frequently contain internal calcificationwhich can be visualized on plain radiography and CT. Typicalcalcification patterns of chondroid matrix are ring-andarc-like or popcorn-like which correlate with histologicalenchondral ossification.[13] On MRI, cartilaginous tumorstypically have intermediate signal on T1WI and high signalon T2WI reflecting the high-water content within the ECMof the hyaline cartilage. The areas of dense calcification arehypointense on both T1- and T2WI.[13-15] The lesions mayenhance avidly, and the intensity of enhancement varies withthe extent of the calcific component [Figure 2]. Studies on thediagnostic utility of FDG PET/CT have produced conflictingresults with some studies indicating limited utility of FDG PETin differentiating benign tumors from low-grade chondroidmalignancies because of significant overlap of SUV max, while
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckTable 2: Characteristic imaging features of cartilaginous tumors of the head and neck.Cartilaginous lesionsCommon locationsCharacteristic imaging featuresBenign cartilaginous tumors andtumor-like lesionsChondroma (aka enchondroma)Cricoid and thyroid cartilagesWell-defined expansile hypodense lesions withvariable amounts of coarse, chondroid, mottledcalcificationDifficult to distinguish from chondrosarcoma onimagingNonspecific well-defined expansile bone lesionscontaining a variable amount of internal chondroidmatrix calcificationIntratumoral cystic degeneration or secondaryaneurysmal bone cysts in one third of tumorsWell-defined, expansile bone lesions with a scleroticrim, intralesional calcification approximately 10%of tumorsExophytic bone lesions with continuity of bonemarrow from the parent bone into the tumor andcartilaginous cap at the peripheryAbnormal thickening of the cartilaginous cap(exceeding 1.5–2.5 cm) indicating malignantdegenerationJoint effusion, abnormal synovial thickening andenhancement suggestive of synovitis, adjacent boneerosion due to mechanical pressure, and calcified ornoncalcified intra-articular loose bodiesRare benign, slow-growing, locally destructive,tumor-like lesionAssociated with pathologic DICER1 genetic variantsExpansile heterogeneous mixed solid and cysticmasses, internal calcifications in 50% of lesionsChondroblastomaSkull base (the squamous portion of thetemporal bone)Chondromyxoid fibromaSkull base, sinonasal cavityOsteochondromaMandible, particularly mandibularcondyle and coronoid processSynovial chondromatosisTemporomandibular jointChondromesenchymal hamartomaSinonasal cavity, orbitMalignant cartilaginous tumorsChondrosarcomaChondroid chordomaSkull base (particularly petroclivalfissure) and cricoid cartilageClivusother studies report a strong correlation between histologicalgrading of cartilaginous tumors and SUV max.[16,17]BENIGN CARTILAGINOUS TUMORS ANDTUMOR-LIKE LESIONSChondromaChondroma is a benign, slowly growing cartilaginoustumor. In the head and neck, the most common locationis the cricoid cartilage, followed by the thyroid cartilage.Expansile soft tissue masses with boneerosion and invasion of adjacent structures,intratumoral calcification up to 50% of skull basechondrosarcomasMRI - heterogeneous T2 hyperintense signal with avariable degree of contrast enhancementTumor location - more frequently located offmidline near the petro-occipital fissureSimilar to conventional chordoma includingexpansile soft tissue mass with adjacent boneerosion and occasional internal calcificationApproximately, 70–75% of laryngeal chondromas arisefrom the endolaryngeal surface of the posterior laminaof the cricoid cartilage.[18] Less common locations arearytenoid cartilage, epiglottis, trachea, nose, ear pinna, andother soft tissues such as muscles of mastication.[18-20] OnCT, chondromas are seen as expansile well-circumscribedhypodense lesions with variable amounts of coarse,chondroid, mottled calcification, arising from a cartilaginousstructure [Figure 3]. When they occur within submucosalregions, the overlying mucosa is altered in contour but isJournal of Clinical Imaging Science 2021 11(66) 3
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckotherwise maintained. MRI appearance of chondromas isless specific because of its relative insensitivity in detectingchondroid calcifications. It can, however, provide additionalinformation with regards to the extent of the lesion due toits high soft tissue contrast resolution.[21] Chondromas andchondrosarcomas are difficult to distinguish on the basis ofimaging, and as such histopathology is always required forconfirming the diagnosis.[21,22]ChondroblastomabacFigure 2: Characteristic CT and MRI features of well-differentiatedcartilaginous tumors. A 19-year-old man with sinonasalchondrosarcoma presenting with sinonasal obstructive symptoms.Axial maxillofacial CT image in bone window (a) shows a largeright sinonasal mass containing internal ring-and-arc calcifications,a classic feature of calcified chondroid matrix (arrow). The tumoris heterogeneously hyperintense on T2W MRI image (b) andmoderately enhancing on post-contrast T1W MRI image withfat suppression (c). Note the T2 hypointense area in the posterioraspect of the tumor (arrowhead in b) corresponding to the area ofdense calcification on CT.Chondroblastomas are rare benign but locally aggressivebone tumors which commonly involve the epiphysis of thelong bones such as distal femur, proximal tibia, and proximalhumerus. Craniofacial chondroblastomas are uncommon,accounting for 2–7% of all chondroblastomas.[1,23,24] Themost common location in the head and neck region is theskull base, with a predilection for the squamous portionof the temporal bone adjacent to the temporomandibularjoint. The other less common sites include mandibularcondyle [Figure 4], paranasal sinuses, and maxilla.[25-28]Histopathological features of chondroblastomas includepolygonal mononuclear cells (chondroblasts), multinucleatedgiant cells, and chondroid matrix. A fine network ofpericellular calcification (so called “chicken-wire” pattern)can be seen in varying amounts. Clinical manifestationsdepend on tumor location, for example, with skull basechondroblastomas presenting as cranial neuropathy andchondroblastoma of the TMJ presenting with jaw pain, etc.Radiologically, chondroblastomas are seen as nonspecificwell-defined expansile osseous lesions containing a variableamount of internal chondroid calcification. Invasion of thesurrounding structures indicates the locally aggressive natureof these lesions.[29,30] Intratumoral cystic degeneration orsecondary aneurysmal bone cysts occur frequently in up toone third of these tumors.[1,23] Although the tumors are locallyaggressive, distant metastasis is rare. Surgical resection withcomplete tumor removal is the standard treatment.[31]Chondromyxoid fibromaabFigure 3: Laryngeal chondroma. A 51-year-old woman withlaryngeal chondroma presenting with hoarseness for 6 months.Axial contrast-enhanced (a) and coronal-reformatted (b) CT imagesshow a small expansile hypodense lesion at the left lamina of thethyroid cartilage (arrows). She underwent open resection of thelesion. Histopathology revealed a hypocellular tumor containinghyaline cartilage. The overlying perichondrium was intact with noevidence of destructive growth.Journal of Clinical Imaging Science 2021 11(66) 4CMF account for less than 1% of all primary osseoustumors and predominantly affect the metaphysis of the longbones, particularly in the lower extremities. CMF of theskull and facial bones are exceedingly rare, with less than100 cases reported in English literature.[32] The previouslyreported locations of craniofacial CMF are skull base,sinonasal cavity, and, less frequently, the calvarium.[31,32]These tumors demonstrate slow growth and tend to invadesurrounding bones and soft tissue structures. Radiologicfindings of CMF are nonspecific. On CT, CMFs are wellcircumscribed, expansile osseous lesions with a sclerotic
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckbacabcFigure 4: Chondroblastoma. A 36-year-old woman withchondroblastoma arising from the right mandibular condylepresenting with worsening right jaw pain. Axial T2WI MRI image(a), axial (b) and coronal (c) contrast-enhanced T1W MRI imageswith fat suppression show an exophytic enhancing T2 hyperintensemass arising from the right mandibular condyle projectingmedially into the right masticator space (arrows). Note edema andenhancement of the right lateral pterygoid muscle (arrow heads).Figure 5: Chondromyxoid fibroma. A 56-year-old woman withchondromyxoid fibroma of the right central skull base presentingwith multiple right cranial neuropathy. Axial T1WI (a), axialT2WI (b) and coronal contrast-enhanced T1W MRI image with fatsuppression (c) show a large expansile mass arising from the rightgreater wing of sphenoid (arrows). The tumor demonstrates mixedsignal intensity on both T1WI and T2WI with small lobular foci ofT2 hyperintensity, and diffuse contrast enhancement.rim. Intralesional calcification is an uncommon imagingfeature and can be identified in approximately 10% of allCMF.[33] MRI characteristics of CMF are similar to othercartilaginous tumors which show low signal on T1WI andheterogenous high signal on T2WI due to its cartilaginousand myxoid components, and heterogeneous enhancementon postcontrast sequence [Figure 5]. The nonspecificimaging appearance spurs a wide differential diagnosis whichincludes chondrosarcoma, chordoma, chondroblastoma,and chondroblastic osteosarcoma. Total tumor resection isthe treatment of choice, with curative intention. In general,curettage is not recommended due to its higher recurrentrate (up to 25%). The role and efficacy of radiation therapyfor local tumor control remains controversial.[32]elsewhere in the body and are seen as exophytic osseouslesions with continuity of bone marrow from the parent boneinto the tumor [Figure 6]. A layer of cartilage known as thecartilaginous cap is seen at the growing end of the lesion.The cartilaginous cap is better seen on MR and typicallyhas low signal on T1WI and high signal on T2WI.[36] Onpostcontrast images, there is enhancement at the peripheryof the lesion which correlates on histology with fibrovasculartissue covering the nonenhancing cartilaginous cap.[39] Thecartilaginous portion of osteochondroma may undergomalignant transformation. Abnormal thickening of thecartilaginous cap (exceeding 1.5–2.5 cm) on imaging is anominous sign and is viewed with suspicion for malignantdegeneration [Figure 7].[40]OsteochondromaSynovial chondromatosisOsteochondroma is a common benign bone lesion whichusually occurs at the end of long bones such as distalfemur.[34] Osteochondroma in the head and neck region isrelatively rare. The most common location is the mandible,particularly the mandibular condyle and coronoid process,but it can arise from any part of the mandible or other osseousstructures in the head and neck.[34-38] On imaging, head andneck osteochondromas are similar to osteochondromas seenSynovial chondromatosis is a benign but locally aggressivedisease characterized by chondroid metaplasia of thesynovium, with subsequent formation of intra-articular loosebodies, causing destruction of the joint.[41,42] In the head andneck, it frequently involves the temporomandibular joint.Synovial chondromatosis can be divided into two subtypes– primary and secondary.[41,42] Pathogenesis of primaryform remains unknown, but according to recent cytogeneticJournal of Clinical Imaging Science 2021 11(66) 5
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckaabFigure 6: Osteochondroma. A 28-year-old woman withosteochondroma of the right mandibular condyle presentingwith chronic right jaw pain. Axial (a) and coronal-reformatted(b) CT images in bone window show an exophytic osseous lesionoriginating from the right mandibular condyle, continuous with themedullary cavity of the mandible (arrow). Note remodeling of theskull base from chronic long-standing pressure effect (arrowhead).abFigure 7: Osteochondroma with secondary chondrosarcoma.A 70-year-old man with secondary chondrosarcoma originatingfrom the osteochondroma of the cervical spine presenting withpalpable lump in the neck. Axial T2W MRI image (a) shows anexophytic T2 hyperintense mass arising from the right ventral aspectof C4 vertebral body (arrow). Axial CT image in bone window (b)shows a few small calcific foci within the tumor (arrowhead). Note asmall underlying osteochondroma deep to the tumor (black arrow).studies, it is believed to be a benign neoplastic process ratherthan metaplastic disease.[43] In contrast, secondary form isassociated with underlying joint diseases such as mechanicaljoint abnormalities or arthritic conditions. Malignanttransformation of primary synovial chondromatosis tochondrosarcoma may occur although it is uncommon.[44]Radiologic features of synovial chondromatosis includejoint effusion, abnormal synovial thickening andenhancement suggestive of synovitis, adjacent bone erosiondue to mechanical pressure, and calcified or noncalcifiedintra-articular loose bodies [Figure 8].[41,42] In chronicdisease, there may be imaging features of coexistentsecondary osteoarthritis and asymmetric joint spacenarrowing. There is potential for intracranial tumorextension due to its close proximity to skull base. CT isthe best imaging modality for detecting calcified intraarticular loose bodies and for assessment of bone erosion.Journal of Clinical Imaging Science 2021 11(66) 6bFigure 8: Synovial chondromatosis. A 45-year-old woman withsynovial chondromatosis initially presenting with chronic nasalcongestion. The left temporomandibular joint abnormality wasincidentally found on maxillofacial CT. Coronal-reformatted CTimage in bone window (a) and coronal contrast enhanced T1WMRI image with fat suppression (b) show abnormal synovialthickening and enhancement with extensive bone erosion of theleft mandibular condyle and adjacent skull base (arrows). Noteabnormal widening of the left temporomandibular joint.MRI can provide additional information on soft tissueabnormalities, including synovitis, and bone marrowinvolvement. On MRI, the signal characteristics of intraarticular loose bodies are variable depending on the degreeof mineralization. Noncalcified loose bodies typically havelow-to-intermediate signal on T1WI and high signal onT2WI whereas calcified loose bodies show fat signal witha peripheral hypointense rim on T1WI and low signal onT2WI [Figure 9].[41] During the early course of the disease,it can be difficult to diagnose synovial chondromatosis onMRI because loose bodies are not well formed, or they maybe obscured by joint effusion.[45]Chondromesenchymal hamartomaChondromesenchymal hamartoma is a rare benign, slowgrowing, locally destructive, tumor-like lesion that containsmixed proliferating mesenchymal and cartilaginouselements such as mature and immature hyaline cartilage.This rare tumor-like lesion occurs predominantly ininfants and young children. The most common sites aresinonasal cavity and orbit.[46,47] The mass can invade skullbase and extend intracranially.[48] There is an associationof pathologic DICER1 genetic variants, a hereditary cancerpredisposition syndrome, with nasal chondromesenchymalhamartoma.[49,50] As such, otolaryngologic evaluation shouldbe performed in individuals with pathogenic DICER1genetic variants who have persistent nasal obstruction.[49]Surgical resection is the treatment of choice.[48] On imaging,chondromesenchymal hamartomas are seen as expansileheterogeneous mixed solid and cystic masses [Figure 10].Approximately, 50% of nasal chondromesenchymalhamartomas contain internal calcifications. On MRI,tumors typically have low-to-intermediate signal on T1,heterogeneous hyperintense signal on T2, and markedheterogeneous contrast enhancement.[51,52]
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckmultiple enchondromas.[54,57] The standard treatment forchondrosarcoma is surgical resection. Adjuvant radiationis usually given when there is residual tumor followingresection or close resection margins to improve local tumorcontrol. Chondrosarcoma is generally considered to beunresponsive to chemotherapy.[55]abFigure 9: Synovial chondromatosis with calcified intra-articularloose bodies. A 50-year-old woman with synovial chondromatosispresenting with left jaw pain. Axial CT image in bone window (a)shows several small calcified intra-articular loose bodies in the lefttemporomandibular joint (arrow) which are hypointense on axialT2W MRI image (b) (arrowhead). Note diffuse synovial thickeningand distension of the joint capsule (black arrow).abFigure 10: Chondromesenchymal hamartoma. A 16-year-oldman with DICER1 mutation and sinonasal chondromesenchymalhamartoma presenting with chronic sinonasal obstructivesymptoms. Axial (a) and coronal reformatted (b) CT images in bonewindow show polypoid opacification with scattered calcifications inbilateral ethmoid sinuses (arrows).MALIGNANT CARTILAGINOUS TUMORSChondrosarcomaChondrosarcoma is the third most common primarymalignant bone tumor after multiple myeloma andosteosarcoma.[53] Head and neck chondrosarcomas accountsfor 1–12% of all chondrosarcomas. They are usually lowgrade (WHO Grade 1 and 2) with slow growth and indolentclinical course.[54] Distant metastasis is uncommon in lowgrade tumors but is more frequent in higher grade tumors(that is, WHO Grade 3). The most common location in thehead and neck is the skull base, with approximately 60–70% of tumors emanating from the petroclival fissure.[54]The other sites such as larynx and sinonasal cavity are lessfrequent.[55,56] Chondrosarcomas usually occur in isolationbut are occasionally associated with Ollier diseaseor Mafucci syndrome, rare diseases characterized byHead and neck chondrosarcomas appear to be a distinctpathologic entity compared to chondrosarcomas arisingelsewhere in the body.[55] A meta-analysis study has shownthat head and neck chondrosarcomas tend to be lowergrade and have significantly higher 10-year disease-specificsurvival and overall survival compared to chondrosarcomasat other sites.[55] A recent study also found that the incidenceof IDH mutation is different among the head and neckchondrosarcomas of different subsites.[58] Approximately,86% of skull base chondrosarcomas have an IDH mutationwhile the incidence of IDH mutation in laryngotrachealchondrosarcomas is only 12%. More interestingly, no IDHmutations are found in maxillofacial chondrosarcomas. Theauthors hypothesized that this could be related to differenttypes of ossification (that is, enchondral ossification in theskull base compared to intramembranous ossification in themaxillofacial bones) and different pathway of tumorigenesisin each location.[58]Radiologically, chondrosarcomas are expansile soft tissuemasses with bone erosion and invasion of adjacent structures.Up to 50% of skull base chondrosarcomas show intratumoralcalcification on CT.[59] Intratumoral chondroid calcification(for example, ring-and-arc or popcorn appearance) is one ofthe most helpful imaging features suggesting cartilaginousorigin of the tumor and best depicted on CT. MRI can providemore information regarding bone marrow and soft tissueinvolvement. MR signal characteristics of chondrosarcomaare low-to-intermediate signal on T1 and hyperintensesignal on T2, with a variable degree of contrast enhancement[Figure 11].[60] Low-grade chondrosarcomas may containinternal T2 hypointense septations and septal enhancementwhich corresponds to fibrovascular tissue on histopathologywhile the nonenhancing areas within tumors represent theareas of hyaline cartilage, cystic mucoid tissue, and tumornecrosis.[39]The main differential diagnosis of skull base chondrosarcomais chordoma; it can be difficult to differentiate the two dueto overlapping imaging appearance. The tumor locationis a helpful imaging clue that may help in differentiationbetween these two entities. Skull base chondrosarcomasare more frequently located off-midline near the petrooccipital fissure, whereas chordomas are more oftenlocated in the midline of the clivus.[61] DWI MRI withquantitative assessment of apparent diffusion coefficient(ADC) values may be helpful in distinction, with somestudies demonstrating skull base chondrosarcomas haveJournal of Clinical Imaging Science 2021 11(66) 7
Wangaryattawanich, et al.: Imaging features of cartilaginous tumors of the head and neckbaabFigure 12: Laryngeal chondrosarcoma. A 59-year-old man withlaryngeal chondrosarcoma presenting with progressive hoarsenessof voice. Axial (a) and coronal-reformatted (b) contrast-enhancedCT images show an expansile partially calcified mass arising fromthe left lateral aspect of the cricoid cartilage (arrows), severelynarrowing the airway. Note characteristic chondroid matrixcalcification within the tumor.cFigure 11: Skull base chondrosarcoma. A 31-year-old man withskull base chondrosarcoma presenting with progressive left cranialneuropathy. Axial T2W MRI image (a) and coronal contrast-enhancedT1W MRI image with fat suppression (b) show a large expansileheterogeneously enhancing T2 hyperintense extraaxial mass centeredat the left petroclival fissure (arrows) extending into the prepontinecistern and causing mild mass effect on the adjacent brainstem andleft temporal lobe. The tumor contains subtle small calcifications(arrowhead), a clue to the diagnosis, best seen on CT (c).higher ADC values compared to chordomas, though furtherresearch is required.[61-63]In the larynx, chondrosarcoma is the most commonnonepithelial tumor, and it is much more common thanchondroma.[64] The most frequent sites of tumor are cricoidcartilage followed by thyroid cartilage. CT characteristics oflaryngeal chondrosarcoma is an endolaryngeal soft tissue masswith or without extralaryngeal extension.[65] Approximately,70–80% of laryn
structures in the head and neck.[34-38] On imaging, head and neck osteochondromas are similar to osteochondromas seen elsewhere in the body and are seen as exophytic osseous lesions with continuity of bone