Transcription
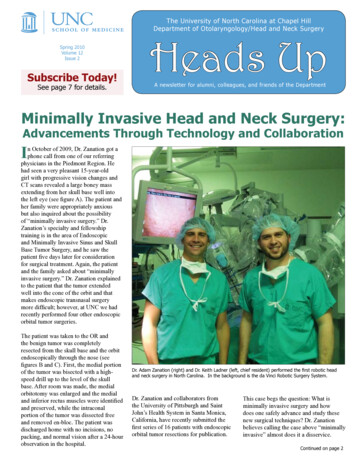
The University of North Carolina at Chapel HillDepartment of Otolaryngology/Head and Neck SurgerySpring 2010Volume 12Issue 2Subscribe Today!See page 7 for details.Heads UpA newsletter for alumni, colleagues, and friends of the DepartmentMinimally Invasive Head and Neck Surgery:Advancements Through Technology and CollaborationIn October of 2009, Dr. Zanation got aphone call from one of our referringphysicians in the Piedmont Region. Hehad seen a very pleasant 15-year-oldgirl with progressive vision changes andCT scans revealed a large boney massextending from her skull base well intothe left eye (see figure A). The patient andher family were appropriately anxiousbut also inquired about the possibilityof “minimally invasive surgery.” Dr.Zanation’s specialty and fellowshiptraining is in the area of Endoscopicand Minimally Invasive Sinus and SkullBase Tumor Surgery, and he saw thepatient five days later for considerationfor surgical treatment. Again, the patientand the family asked about “minimallyinvasive surgery.” Dr. Zanation explainedto the patient that the tumor extendedwell into the cone of the orbit and thatmakes endoscopic transnasal surgerymore difficult; however, at UNC we hadrecently performed four other endoscopicorbital tumor surgeries.The patient was taken to the OR andthe benign tumor was completelyresected from the skull base and the orbitendoscopically through the nose (seefigures B and C). First, the medial portionof the tumor was bisected with a highspeed drill up to the level of the skullbase. After room was made, the medialorbitotomy was enlarged and the medialand inferior rectus muscles were identifiedand preserved, while the intraconalportion of the tumor was dissected freeand removed en-bloc. The patient wasdischarged home with no incisions, nopacking, and normal vision after a 24-hourobservation in the hospital.Dr. Adam Zanation (right) and Dr. Keith Ladner (left, chief resident) performed the first robotic headand neck surgery in North Carolina. In the background is the da Vinci Robotic Surgery System.Dr. Zanation and collaborators fromthe University of Pittsburgh and SaintJohn’s Health System in Santa Monica,California, have recently submitted thefirst series of 16 patients with endoscopicorbital tumor resections for publication.This case begs the question: What isminimally invasive surgery and howdoes one safely advance and study thesenew surgical techniques? Dr. Zanationbelieves calling the case above “minimallyinvasive” almost does it a disservice.Continued on page 2
This patient underwent significant risksto the brain and her vision, so minimallyinvasive doesn’t mean minimal risks. Dr.Zanation believes minimally invasivesurgery means any novel techniquesthat result in less functional and qualityof life deficits without compromisingthe long-term efficacy of the surgery.For endoscopic skull base surgery, theprimary benefit is no brain retraction andno need for a formal craniotomy. Theseadvantages have the potential to limitbrain trauma and improve neurocognitiveand neurofunctional outcomes, and ifimproved cosmetic or “no incision”surgery is possible, then it is a secondarybenefit. So how does a surgical teamstudy these new techniques?Surgical science is rooted in a foundationof step-wise thought. First, the approachor technology must be conceived, andthen pre-clinical testing illustrates thefeasibility of new approach prior topatient application. The next step takesthe surgery to highly selected patientswith the short-term goal of studyingtechnical limitations and peri-operativesafety. Lastly, longer-term primaryoutcomes such as tumor control mustbe studied. All these are within thebounds of routine clinical care; however,studying cost, quality of life, and specificfunctional outcomes takes additionaleffort and planning outside the realm ofclinical care.This pathway of prospective, hypothesisdriven, and controlled evaluation of cost,quality of life, and functional outcomes isone of keystones for the Zanation-EbertLab. Dr. Charles Ebert is a new attendingfaculty at UNC with fellowship trainingand a special interest in complex andminimally invasive surgery for sinonasalinflammatory disorders. He and Dr.Zanation have joined in a collaborativelab group to develop and study theoutcomes of novel surgical techniquesand technologies. This collaboration hasbeen immensely successful, resulting ina significant volume of research ideasand data, including three newly active,prospective clinical surgical trials in onlynine months. This success and modellead Dr. Zanation along with Dr. RobertBuckmire to conceive of the Universityof North Carolina Minimally InvasiveOtolaryngology/Head and Neck SurgeryCenter.2A. Pre-operative coronal CT scan showing skullbase and orbital mass.and Neck Surgery through technology,research, and minimally invasive surgicaltechniques. It is an umbrella for all typesof advancements in surgical techniquesand morbidity across all subspecialtiesof Otolaryngology (from Head and NeckSurgery to Laryngology to Rhinology,etc.). The goal of the Center is to advancesurgical care while prospectively studyingsurgical outcomes. This Center is opento all fields of Otolaryngology/Headand Neck Surgery at UNC, and we hopethrough cross-pollination of ideas fromdifferent specialties we can even furtheradvance minimally invasive techniquesand technology, such as robotic assistedsurgery (see The UNC Robotic Headand Neck Surgery Program, page 3),across multidisciplinary fields. Thelong-term goal of the Center is to obtainB. Post-operative coronal CT with completeresection of mass via an endoscopic approach.C. Post-operative axial CT scan with completeresection.The UNC Minimally InvasiveOtolaryngology/Head and NeckSurgery Center has been set up as thefirst such center in the United States.The mission statement of the Centeris Advancing functional and quality oflife outcomes in Otolaryngology/HeadChair’s CornerThis issue of Heads Up is very telling of the progress thatwe have made in our Department at both the research andclinical levels. The utilization of the robot in the clinicalarena is extremely exciting. In addition, the developmentof minimally invasive techniques in approaching the skullbase has allowed us to perform operations which previouslywould have been extremely morbid to the patient.Harold C. Pillsbury, MDDepartment ChairThe continued efforts that we have in Malawi areemphasized by Dr. Carlton Zdanski’s collaboration with Dr.Carol Shores, who has had a long-standing commitment tothe Head and Neck Surgery effort there.Our research accomplishments have rounded out themissions of the Department. Our medical students, Adam Campbell and Tom Suberman,have done a tremendous job in the laboratory working on issues related to cochlearimplantation. They have presented at the American Otologic Society and the AmericanNeuro-Otologic Society in early May.Finally, it was wonderful for me to reminisce with John Emmett, who was a co-resident ofmine in Otolaryngology/Head and Neck Surgery here at UNC in the 1970s.I hope you enjoy reading this as much as I have.www.med.unc.edu/ent
research funding to support these areasof development and research whileadvancing surgical techniques withinOtolaryngology.Currently active prospective clinicaltrials within the UNC Minimally InvasiveOtolaryngology/Head and Neck SurgeryCenter are listed below. We hope to opensuch outcomes trials within each divisionof the Department of Otolaryngology/Head and Neck Surgery. Multiple othertechnical, anatomic and retrospectivestudies are also underway:1. Prospective Morbidity, Quality of Lifeand Neurocognitive Outcomes after SkullBase Surgery2. Prospective Evaluation of the ClinicalImpact and Outcomes of a MultidisciplinaryHead and Neck Tumor Board3. Analysis and Comparison ofOutcomes, Gene Expression Profiles andEosinophilic Pathways in Allergic FungalRhinosinusitisFor more information on the UNCMinimally Invasive Otolaryngology/Headand Neck Surgery Center, see our websitecoming soon at unc-net.org or call 919966-3343 for Dr. Zanation.The UNC Robotic Head and Neck Surgery ProgramIn March 2010, the Dr. Zanationperformed North Carolina’s firstTransoral Robotic Head and NeckSurgery (TORS). This surgery wasthe culmination of over 12 months ofwork to set up a Robotic Head andNeck Surgery Program with the helpof the CARES (Computer And RoboticEnhanced Surgery) Center at UNC.In December 2008, Dr. Zanation metwith Dr. John Boggess, Departmentof Obstetrics and Gyncology, todiscuss a future robotics programfor Otolaryngology/Head and NeckSurgery. Dr. Boggess is internationallyrenowned for his techniques andresearch with robotic assisted surgeryfor Gynecologic Oncology. With Dr.Boggess’ mentorship and support,Dr. Zanation began training with theda Vinci Robotic Surgery System inthe Fall of 2009. Our first patient hada base of tongue procedure withoutcomplications.ability to access areas of aerodigestivetract without incisions or splitting themandible. This has the potential toreduce surgical morbidity and providebetter patient functional outcomes.The da Vinci robotic surgery systemis a three-dimensional endoscopebased robot with three articulatinginstrument arms. As the surgeonoperates, state-of-the-art robotic andcomputer technologies scale, filter,and seamlessly translate the surgeon’shand movements into precise micromovements of the da Vinci instruments.The primary advantage of the systemis high definition 3D visualization,flexibility with complex instrumentmovements in tight spaces, and theThe UNC Robotics Program iscurrently seeing patients for selectedhead and neck cancers, tongue baserelated obstructive sleep apnea, andskull base tumors. Future researchplans involve expanding roboticindications for skull base surgery andmerging other technologies with therobotic interface. For patient referrals,call Laura Lyndon-Miller at the Headand Neck Oncology Program at 919966-9717.Intuitive surgical da Vinci Robotic SurgicalSystemIntraoperative view of robotic base of tongue resectionHeads Up3
Malawi: The Warm Heart of Africaby Jessica Smyth, MD; Carol Shores, MD, PhD; and Carlton Zdanski, MDinvolved in all of the operative cases. Theyquickly assimilated the information andby the end of our stay, Gift was able toperform a cleft lip repair.On a clinic day, Dr. Zdanski takes time between patientsto teach two of the residents, Dr. Gift Mulima (left) andDr. Rahim Ibrahim.Word of the arrival of “Dr. Carol”spread quickly at Kamuzu CentralHospital (KCH) and our clinic wasfilled Monday morning with expectantfaces. Landlocked Malawi ranks amongthe world’s most densely populatedand least developed countries. Its 15million people are served by four majorhospitals, one of which is KCH, locatedin the capital city of Lilongwe. Thereis only one otolaryngologist in Malawi;consequently, it is a rare opportunity tofind a surgeon who is able to treat some ofthe problems more unique to our specialty.Dr. Arturo Muyco, the chair of the SurgeryDepartment, was well aware of this factand notified the district hospitals thatDr. Carol Shores would bring two cleftsurgeons with her – Dr. Carlton Zdanskiand Dr. Krishna Patel. We set up ourmakeshift clinic in a conference room andevaluated the assembled patients, somewho had been awaiting our arrival formonths. Our operating room schedulefilled quickly.Although there is a recognized need inMalawi for otolaryngologists, as well assurgeons from a multitude of specialties,short-term trips are not the most effectivemethod to fill this void and herein lay ourtrue objective. KCH established a surgicalresidency program one year ago and ourgoal was to teach these residents – GiftMulima, Tiyamike Chilunjika and RahimIbrahim – about the principles and practiceof otolaryngology. During our stay, wefocused on their education. In additionto receiving a series of lectures from Dr.Zdanski and Dr. Patel, they were actively4We had the opportunity to manage severalvascular malformations in children.This included the use of propranolol ina severely disfiguring hemangioma in aone-year-old child, which required thecompounding of the drug. Thanks goout to Jenn Zanation who assisted us indirections for compounding from here inthe states. The residents from KCH informus the child is dramatically improved. Thisalso points to the wonderful advantagespresented by this unique opportunity whichallows us to work with clinicians who liveand work in-country and who can providecontinuing care, follow-up, and helpmanaging potential complications.Dr. Zdanski also brought a set of pediatricesophagoscopes, bronchoscopes, andendoscopic foreign body forceps withhim as a very generous donation fromthe Karl Storz Company. During our trip,three children presented with foreignbody aspiration. Dr. Zdanski was ableto teach techniques to the residents andclinical officers to successfully managethe foreign bodies in all of the children.Proper cleaning and care of the equipmentwas taught as well. At the end of the trip,the equipment was left at KCH where itwill significantly improve the ability of theMalawian clinicians to better manage thiscommon problem.In addition to airway, cleft, and vascularmalformation cases, we had theDr. Zdanski demonstrates airway endoscopy as a clinicalofficer takes a look through the scope. The endoscopyequipment was generously donated by Karl Storz GmbH& Co. KG.opportunity to operate on neck masses andan unfortunate case of Noma. We wereable to impart new anesthetic managementtechniques, such as the use of localepinephrine and spontaneous ventilationduring foreign body removal. We even gotopportunities to share our technique formastoidectomy – we performed two withheadlights (camping headlights, that is),mallets, chisels, and curettes. Thankfully,we had brought our loupes for the clefts.Prior to this trip, we were able to collectand send 20,000 worth of books for theresident library and medical equipment forthe theater (operating rooms) and wardsthanks to the generous donations of manyof you. Additionally, we collected moneyto provide each of the residents with alaptop computer. Each resident voiced theirsincere thanks, as their access to computershad been very limited and this would be avaluable tool to their continued education.On the trip to Malawi, Dr. Smyth read abook titled, “The Boy Who Harnessedthe Wind,” by William Kamkwamba.This is a fantastic snapshot of the life of aman raised in this Malawi. One synopsisstated, “Much more than a memoir, this isa snapshot of life as a precocious teenagerin contemporary Africa, and an affirmationof the notion that talent, beauty, andbrilliance are distributed in equal measurearound the world, even if opportunity isnot. This is a story that hums with theexcitement of an individual who, like thecontinent where he was raised is poised forgreatness.” It is our mission to continue toprovide opportunities and training for theseresidents, the talent and future of Malawi.We sincerely thank all of you who haveshown interest in this endeavor and alsofor your continued support. Plans arealready in the works for return educationaltrips to Malawi with Drs. Shores, Zdanski,and Patel. It is our goal to have a sustainedcontinuing surgical educational presencein otolaryngology/head and neck surgeryat KCH. If you wish to donate to theeducation of the residents at KCH, andthe new class who will start July 2010, wehave a fund established. Please contactHolli Gall, Major Gifts Officer, at (919)843-5734, or holli gall@med.unc.edu.www.med.unc.edu/ent
Future Otolaryngologists Gain SignificantResearch Experience in Fitzpatrick Labby Thomas A. Suberman and Adam P. CampbellSince 1999, the Fitzpatrick lab has been aplace for residents and medical studentsto gain significant research experience.Although the projects have changedthrough the years, the guidance of Dr.Doug Fitzpatrick has remained constant.Currently, both Adam Campbell andThomas Suberman are taking a year awayfrom medical school to devote to researchwith Drs. Fitzpatrick , Oliver Adunka, andCharles Ebert.Tom: I grew up on a farm several milesfrom the UNC campus, attending localpublic school, then Carolina FriendsSchool, and UNC, before graduatingfrom Skidmore College. I then went on toColumbia University’s postbaccalaureateprogram, where I completed premedcoursework while working and volunteeringin hospitals around New York City. I movedback to Chapel Hill for medical schoolthinking that I would pursue a career inpsychiatry. But that changed during mythird year clerkship in Otolaryngologywhen I discovered, during a radical neckdissection with Dr. Shockley, that I lovedsurgery. I realized the field of ENT wouldallow me to work with patients in acute andlong-term settings, as well as collaboratewith physicians who were as concernedwith their patients and research as they wereabout one another. After the clerkship ended,I created a month-long elective to researchminimally invasive pituitary surgery underDrs. Charles Ebert and Brent Senior. I thenreceived the year-long T32 NIH traininggrant which has enabled me to spend thisyear working under Drs. Fitzpatrick andAdunka, as well as to continue my clinicalwork with Dr. Ebert.Adam: I was raised in Charlotte, NorthCarolina, and completed my undergraduatework at Vanderbilt University. I first becameinterested in Otolaryngology after hearingDr. Craig Buchman’s lecture on cochlearimplants during my first year of medicalschool. Subsequently, I spent the nextsummer working with Dr. Buchman andDr. Adunka building the pediatric cochlearimplant database under the T32 traininggrant. I continued to work on this databasefor the next two years, at which point IHeads UpLeft to right: Tom Suberman, Doug Fitzpatrick, PhD; Oliver Adunka, MD; and Adam Campbellreceived a departmental training grant tospend a year working with Drs. Fitzpatrickand Adunka. Currently, I am continuing touse the pediatric database to evaluate thecorrelation between endolymphatic ductand sac size and degree of hearing lossin patients with large vestibular aqueductsyndrome.Under the tutelage of Drs. Fitzpatrickand Adunka, our primary project hasbeen the development of an intracochlearrecording system that will allow surgeonsto assess intracochlear trauma duringcochlear implantation. This is important,as studies have shown that cochleartrauma and electrode malpositioning canlead to decreased speech perception incochlear implant recipients. To develop thistechnology, we have been using an animalmodel to define electrophysiologic patternsof damage caused by electrode interactionwith intracochlear structures. Ultimately,this system could reduce intracochleardamage, maximize hearing preservation, andimprove patient outcomes.So far, our research efforts have been veryfruitful. We both presented at the MidwinterMeeting of the Association for Research inOtolaryngology in Anaheim, California, forwhich we each received a travel award. Weare currently preparing multiple manuscriptsfor publication and have been acceptedto present our work at the CombinedOtolaryngology Societies Meeting in LasVegas, Nevada, this April.In addition, we have been working ona number of other projects. With Drs.Fitzpatrick and Cant (Duke University), weare helping to map the medial geniculatebody of the gerbil thalamus. We are alsotraining rabbits to distinguish betweenvowel sounds in order to determine ifsounds can be discerned with patternedelectrical stimulation of the midbrain.Finally, continuing the long legacy ofallergy experiments at UNC, we are workingwith Drs. Ebert and Jiri Prazma to determinewhether bacterial infections in rats prime themiddle ear for future otitis media.This year of research has been wonderful,and none of it would be possible without theincredible mentorship of Drs. Fitzpatrick,Adunka, and Ebert. The dedication thatthe Department demonstrates to researchand medical students is truly astounding.During this year, we have learned to developquestions, present our results and writemanuscripts and skills that will undoubtedlyassist us in our future academic careers.5
What Ever Happened to. Dr. John Emmett?When I first met Dr. Newton Fischer,I remember him looking at me andsaying, “Um, what makes you so special?”My reply was simply, “I don’t know Ijust want to do head and neck surgery.” Ireceived Dr. Fischer’s blessing to train meat UNC after a long interview (or was itan interrogation?). In July 1974, I joinednone other than Dr. Harold “Rick” Pillsburyand Dr. Henry “Harry” McDonald as firstyear residents in Otolaryngology/Head andNeck Surgery. Rick impressed me with hisenthusiasm and boundless energy. Harry wassoft spoken with a quick smile and a downhome sense of humor. It was a real pleasureto work with both of these individuals as weshared duties at the bottom of the residencytotem pole.Dr. Newton Fischer and Dr. Paul Biggerswere master teachers with each one havinga distinct approach to training residents.These two individuals were two of the mostintelligent and amazing people I have evermet. Dr. Fischer always demanded the verybest out of each of us, and rightly so. Heled by example and was at times a sterntaskmaster, but there was no doubt thatthe well being of each resident and theirfamily was of paramount importance to him.When Dr. Fischer was in deep thought, heoftentimes would reach over his head withhis right arm to scratch the left side of hishead. All of us caught ourselves doing thesame thing after a while! Dr. Fischer was andstill is a true renaissance man. His love of theart and science of medicine is matched byhis love of music, literature and especiallygardening. During my years with Dr. Fischer,each resident, sooner or later, had a vegetablegarden, even if the “garden” was a lonetomato plant in a pot outside of their house.My residency years were enlivened byfrequent invitations to the Fischer’s homeand to the home of Dr. Biggers, the latterof whom had a bodacious sense of humor.These events were unique occasions forall of us, each one of which developed apersonality of its own. The sign beside theBiggers’ mailbox actually read “The BiggersFunny Farm”. Their get-togethers usuallyincluded cook-outs with lots of suds andlots of talk. Things were a bit more formalat the Fischer’s home, but always fun.The food was always delicious and wasaccompanied by conversation that rangedover a wide variety of topics. Undoubtedly, Iwas attending one of these affairs when I firstmet Amelia as a young lady. She entertainedus, if I remember correctly, by playing the6Dr. John Emmett, on the far right, with his family. His oldest daughter Kathleen is beside him, with her husband MikeFilosa. Beside Mike is Dr. Emmett’s wife Karen, and on the left end is daughter Susan.harpsichord. The Division of Otolaryngologywas indeed one big extended family.On a more personal note, I became “hooked”on otologic surgery after my first procedureusing an operating microscope. During mysecond year of residency at UNC, I struckup a correspondence with Dr. John Shea inMemphis, concluding with me spendingthree weeks at the Shea Ear Clinic. At theend of the three week period Dr. Shea offeredto train me for a year in his FellowshipProgram, only later to switch that offer tojoin him as an associate. Those early yearswere an interesting period in otology, withvisitors arriving almost on a daily basis fromall over the world to observe Dr. Shea inthe operating room. After I joined Dr. Shea,UNC residents came to Memphis for a 2-4week rotation for a number of years. Rick, Ishould probably start saying Dr. Pillsbury atthis point, joined us for a few months beforegoing to Zurich to train with Dr. Ugo Fisch.In 1998, Greg Staffel and his lovely wife,Marian, visited us at the Shea Clinic. Onething lead to another and all of us at the SheaEar Clinic feel very fortunate that Greg madethe decision to join us in practice. Greg hasbuilt a very strong practice centered aroundnasal and sinus procedures, as well as facialcosmetic surgery.My wife Karen and I celebrated our 30thwedding anniversary last October. Wehave two daughters. My oldest daughter,Kathleen, graduated from University ofGeorgia majoring in Journalism. Our youngerdaughter, Susan, did her undergraduateyears at Princeton and will graduate fromDuke Medical School this spring. She willwe be entering a residency program inOtolaryngology/Head and Neck Surgery inJune 2010.The Department of Otolaryngology/Headand Neck Surgery at UNC has a very specialplace in my heart. Dr. Newton Fischer, ascharged by his mentor at Johns Hopkins,Dr. Crow, has trained many of the muchneeded otolaryngologists in the state ofNorth Carolina. As the torch was passed, Dr.Pillsbury took up a new charge to train thevery finest academicians for our specialty.To Dr. Pillsbury’s credit, nearly every majortraining program in our nation sits beneath apatch of blue sky – Carolina blue sky.Since John Emmett left UNC, he has servedas President of the Memphis Society ofOtolaryngology – Head & Neck Surgery,President of the Tennessee Society ofOtolaryngology – Head & Neck Surgery,and President of the Tristate (GA, AL, TN)Society of Otolaryngology. He has served asSecretary, and later as Vice President, of theSouthern Section of the Triological Society.He has been President of Otosclerosis StudyGroup, and President of the Centurion’s ofthe Deafness Research Foundation. He is amember of the Otologic Society, NeurologicSociety, and Triological Society. Every yearsince 1996 he has been selected as one ofthe “Best Doctors” in America. He hasperformed over 15,000 otologic procedures.www.med.unc.edu/ent
Announcements(Just a few of the many exciting things happening in our Department)The annual meeting of the Newton D. FischerSociety will be held on Saturday, June5th, in Chapel Hill. Dr. Austin Rose is theCourse Director and promises an outstandingprogram. They keynote speaker is GeraldHealy, MD, Professor of Otolaryngology andLaryngology at Harvard Medical School andOtolaryngologist-in-Chief and Surgeon-inChief at The Children’s Hospital in Boston.The last day to register is May 21st. ContactDawn Wilson (dawn wilson@med.unc.eduor 919-966-8926) for information.The Pediatric Otolaryngology FellowshipProgram is entering its second year. After avery successful beginning, Dr. Alisha Westwill serve as our next fellow following Dr.Laura Rosenthal’s departure for LoyolaUniversity in Chicago. “We know Alishawell from her great work as a resident hereat UNC and are thrilled at the opportunity tocontinue working with her as she continuesher training at the fellowship level,” saidDr. Austin Rose, Director of the PediatricOtolaryngology Fellowship Program.Dr. Craig Buchman was invited facultyat the Medical College of Georgia’sTemporal Bone Course. This course for bothresidents and practicing otolaryngologiststook place in February. Dr. Buchmangave two talks: “The Chronic Ear” and“Cochlear Implants in Children.” Hewas also an invited faculty presenter atthe Midwinter Meeting sponsored by theDepartment of Otolaryngology of theUniversity of Colorado. His two talks were“Electroacoustic Stimulation in Adults” and“Round Window Stimulation in Adults.” Healso served on the “Cochlear Implantation”panel.Dr. Adam Zanation has pioneered a newsurgical procedure for minimally invasivecancer surgery reconstruction. Dr. MihirPatel, a T32 research track resident, hasbeen working in Dr. Zanation’s lab andwrote a paper on the outcomes of this novelreconstructive technique for skull basecancer patients. This was published in theprestigious journal Neurosurgery in March,2010. The paper, entitled “Pericranialflap for endoscopic anterior skull-basereconstruction: clinical outcomes andradioanatomic analysis of preoperativeplanning,” was co-authored by third-yearresident Dr. Rupali Shah with Dr. Zanation asthe senior author.Heads UpThe Southern States Rhinology Coursewas held April 8-10 at Kiawah Island,South Carolina. This course for practicingotolaryngologists and residents provided acomprehensive update on the medical andsurgical practice of rhinology. A hands-onlaboratory dissection component featuredstate-of-the-art endoscopic instrumentation,video, and image guidance systems.The distinguished faculty of academicotolaryngologists from the southeasternUnited States included our own Dr. BrentSenior.A future otolaryngologist interested incraniofacial research, Gitanjali Madan wonthe Harold C. Pillsbury Award (First Place)for her basic science poster presentation,“Umbilical Cord Derived Mesenchymal StemCells Demonstrate Robust Osteoinductionand May Be an Ideal Source for TissueEngineered Bone,” at the John B. GrahamStudent Research Day on January 27, 2010.This same poster won Second Place forOutstanding Medical Student Poster at theAmerican College of Surgeons ClinicalCongress in October 2009. Ms. Madanworks in the lab of Dr. John van Aalst(Department of Surgery, Division of Plasticand Reconstructive Surgery), and theyhave been collaborating with Dr. AmeliaDrake (Chief of the Division of PediatricOtolaryngology and Director of the UNCCraniofacial Center) on a clinical projectthat will be presented at COSM in April.Dr. Jake Dahl will spend 6 months in hissecond year of residency working in thislab to continue the project. Ms. Madanis currently doing research as a HowardHolderness Distinguished Medical ScholarsResearch Fellow and will begin her fourthyear of medical school after the Fellowship.She is also the Wolfgang and Daisy LoskenCraniofacial Research fellow for the 20092010 academic year. After medical school,she is interested in pursuing a residency inOtolaryngology.Dr. Adam Zanation was invited faculty at theUniversity of Nebraska Sinus Course in Vail,Colorado, March 10-12, as well as invitedfaculty at the University of PennsylvaniaMedical Center Skull Base Course, March16-19. He was also selected to the 2010American Academy of Otolaryngology-Headand Neck Surgery CORE Grant ReviewCommittee.Dr. Carol Shore
The UNC Robotic Head and Neck Surgery Program I n March 2010, the Dr. Zanation performed North Carolina's first Transoral Robotic Head and Neck Surgery (TORS). This surgery was the culmination of over 12 months of work to set up a Robotic Head and Neck Surgery Program with the help of the CARES (Computer And Robotic Enhanced Surgery) Center .