Transcription
INTERNATIONAL BEST PRACTICEBEST PRACTICEGUIDELINES: EFFECTIVESKIN AND WOUNDMANAGEMENT OFNON-COMPLEX BURNS3 BEST PRACTICE GUIDELINES: EFFECTIVE SKIN AND WOUND MANAGEMENT OF NON-COMPLEX BURNS
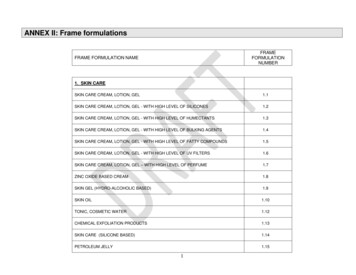
FOREWORDSupported by an educationalgrant from B BraunThe views presented in thisdocument are the work of theauthors and do not necessarilyreflect the opinions of B Braun. Forfurther information about B Braunwound care products, please go to:http://www.woundcare-bbraun.com Wounds International 2014Published byWounds InternationalA division of SchofieldHealthcare Media LimitedEnterprise House1–2 HatfieldsLondon SE1 9PG, UKwww.woundsinternational.comTo cite this document.International Best PracticeGuidelines: Effective skin andwound management of noncomplex burns. Wounds International, 2014.Free download available from:www.woundsinternational.comC 3 This document is a practical guide to the management of burn injuries forhealthcare professionals everywhere who are non-burns specialists.With an emphasis on presenting hands-on and relevant clinical information,it focuses on the evaluation and management of non-complex burn injuriesthat are appropriate for treatment outside of specialist burns units. However,it also guides readers through the immediate emergency management of allburns and highlights the importance of correctly and expediently identifyingcomplex wounds that must be transferred rapidly for specialist care. Finally, itlooks at the ongoing management of newly healed burn wounds and postdischarge rehabilitation.The document acknowledges the importance of continuous and integratedinput from all members of the multidisciplinary team, where such a teamexists, while recognising the role and resources of singlehanded and outreachgeneralists providing a complete care service.Although strategies vary within and between regions, this document seeks topresent the essential key best practice principles that can be applied universally and adapted according to local knowledge and resources.EXPERT WORKING GROUPBishara Atiyeh, Professor of Plastic and Reconstructive Surgery, Division of Plastic Surgery,American University of Beirut Medical Centre, Department of Surgery, LebanonJuan P Barret, Head, Department of Plastic Surgery and Burns & Director, Burn Center/Face andHand Transplantation Program & Professor of Surgery, Department of Surgery, UniversityHospital Vall d’Hebron, Barcelona, SpainProfessor Hu Dahai, Professor of Surgery, Department of Burns and Cutaneous Surgery, XijingHospital, The Fourth Military Medical University, Xi'an, PR ChinaProfessor Franck Duteille, Head of Plastic, Reconstructive and Aesthetic Surgery Unit and BurnsCentre, CHU, Nantes, FranceAnn Fowler, Burns Outreach Senior Nurse Practitioner, Stoke Mandeville Hospital, UKDr Stuart Enoch, Director of Education and Research, Doctors Academy Group, Cardiff, UK,Visiting Professor, Department of Biomedical Technology, Noorull Islam University, IndiaElizabeth Greenfield, Administrative Director, International Society for Burn Injury, Texas, USAAndré Magnette, Head Nurse, Burns Unit, Centre Hospitalier Universitaire de Liège, BelgiumHeinz Rode, Emeritus Professor of Paediatric Surgery, Red Cross Children's Hospital, Universityof Cape Town, South AfricaProfessor Xia Zhao-fan, Professor and Chairman, Department of Burn Surgery, ChanghaiHospital, Second Military Medical University, Shanghai, PR ChinaBESTPRACTICE GUIDELINES:BEST PRACTICEGUIDELINES: EFFECTIVEEFFECTIVE SKINSKIN ANDAND WOUNDWOUND MANAGEMENTMANAGEMENT OFOF NON-COMPLEXNON-COMPLEX BURNSBURNS
INTRODUCTIONIntroductionBurn injuries present many challenges to thediverse range of healthcare professionals whoencounter them worldwide. The EuropeanBurns Association describes a burn injury as acomplex trauma needing multidisciplinary andcontinuous therapy1.Most non-complex burn injuries (see Box 1for definitions) will heal spontaneously withconservative treatment. However, the qualityof initial care will affect the pain and distress apatient may experience, and will greatly influence the aesthetic and functional outcome.Studies show that burn injuries that take morethan 2–3 weeks to heal are much more likelyto result in hypertrophic scarring2.Complex burns must be promptly and appropriately identified and referred. Practitionerscalled on scene must also be well versed inemergency management, including optimalfluid resuscitation and wound care, prior totransfer.BOX 1: DEFINITIONSThis document uses the following definitionsNon-complex burn: (previously described asminor burns) any partial thickness thermalburn covering )15% total body surface area(TBSA) in adults or )10% in children ()5% inchildren younger than 1 year) that does notaffect a critical area*. Includes deep dermalburns covering )1% of the body.Complex burn: (previously described as major burns) any thermal burn injury affecting acritical area* or covering 15% TBSA in adultsor 10% in children ( 5% in children youngerthan 1 year). All chemical and electrical burnsare considered complex.*Burns to hands, feet, face, perineum or genitalia, burns crossing joints and circumferentialburnsSIZE OF THE PROBLEMWorldwide, an estimated 6 million peopleseek medical treatment for burns annually, butmost are treated in outpatient clinics (WorldBurn Foundation www.burnfoundation.com).However, the lack of national and internationalregistration of burns injuries makes it difficultto estimate the true cost of burns.In developing low- and middle-incomecountries (LMICs), burn injuries are an indomitable problem, and much more commonthan in the USA and Europe or other highincome developed countries3. However, theexact number of burns in LMICs is difficultto determine. A conservative estimate putsthe number of people admitted to hospitalwith burns in India (population over 1 billion)at some 700,000 to 800,000 each year 4.WHO reports that the majority of burnrelated deaths occur in LMICs, in particularSouth-east Asia (Figure 1) (Box 25).FIGURE 1: Regional distribution offire-related mortality64%9%BOX 2: REGIONAL DIFFERENCES IN BURN RATES5Q Infants in the WHOAfrican Region have threetimes the incidence ofburn deaths of infantsworldwideQ Boys under 5 years livingin LMICs of the WHOEastern MediterraneanRegion are almost twiceas likely to die from burnsas boys living in LMICsof the WHO EuropeanRegionQ The incidence of burninjuries requiring medicalcare is nearly 20 timeshigher in the WHO Western Pacific Region than inthe WHO Region of theAmericas9%53%10%15%South-east AsiaWestern PacificAfricaEuropeEastern MediterraneanUSAIlliteracy, poverty and urban overcrowding,along with social, infrastructural, economicand cultural issues complicate further theuniversal challenges of prevention and management3,4. A discussion of the strategiesneeded to address these issues is beyondthe scope of this document, but the mainpoints for consideration are listed in Box 3(see p2).Survival outcomes in developed countries have improved dramatically overthe decades, so the emphasis today is onrestoring post-burn function, appearanceand confidence by taking a consideredmultidisciplinary approach at all stages ofmanagement9,10.BEST PRACTICE GUIDELINES: EFFECTIVE SKIN AND WOUND MANAGEMENT OF NON-COMPLEX BURNS1
INTRODUCTIONBOX 3: STRATEGIES FOR BURNMANAGEMENT IN LMICs. ADAPTEDFROM4,6,7,8Q Include burns as part of the national healthagendaQ Drive effective prevention programmes,including burn educational campaigns inschoolsQ Create a central registry of burns to document extent of burnsQ Improve pre-hospital care with promotionof better referral systems based on triageQ Develop regional centres of excellencewith basic burn care undertaken at districtand base hospitalsQ Define health needs based on priorities defined locally with optimisation of existingfacilities to achieve minimally acceptablestandards of careQ Implement cost-effective treatment approaches (re-use/recycle/adapt availableresources)Q Develop a national body of burn professionals to educate healthcare staffinvolved in burn careUsing the UK (population about 60 million)to illustrate the size of the problem in developed countries, each year around10,11:Q 250,000 people receive burn injuriesQ 175,000 of people with burns attendemergency departmentsQ 16,000 of these are admitted to hospitalfor specialist careQ 1,000 people have burns severe enoughfor formal fluid resuscitationQ 300 people die as a result of their burninjury.In the USA (population about 314 million),each year around12,13:Q 1.25 million people receive burn injuriesQ 450,000 of these receive medicaltreatmentQ 40,000 people require in-hospital care,including 30,000 at hospital burn centresQ 5,500 people die as a result of their burninjury.must be made clear to first-aid physicianswho work at the scene of burn accidentsand to those involved in after-treatment inhospitals how extremely important it is topossess adequate basic knowledge15.Inappropriate or poor treatment may resultin complications, such as infection and scarring, unnecessary pain and anxiety for thepatient and family and increased societalcosts (e.g. temporary loss of school or workactivities).TRAINING AND EXPERIENCEMost burn injuries (around 90% in the UKand the USA) are non-complex woundsthat can be safely and effectively managedoutside of specialist burns units10,12,13,16.Non-complex burns are commonly assessedby a range of healthcare professionals, andthere is a need to have agreement aboutwhat types of injury need referral to a specialist burn facility. However, distinguishingbetween complex and non-complex burns isnot straightforward, and many non-specialistdoctors and nurses lack experience or formaltraining in burn management.In a survey carried out in the minor burn facility of the Royal Perth Hospital in Australia,only 39% of patients had received appropriate first aid from their primary healthcareprovider17. In a review of minor burns care inhospital emergency departments in Ontario,Canada, 70% of clinicians surveyed saidthey would not measure burn area whenassessing a patient and 45% did not discussanalgesic requirements18. Both are keycomponents of burn care. These are seriousissues as poor initial management can causea superficial burn wound to progress to adeeper, more complex wound19.In some parts of the world, uncertainty andmisconceptions about management arecomplicated by limited resources and lack ofsupport personnel.A European-wide systematic review foundthat, across Europe, mortality rates varyfrom 1.4% to 18%14. There was a clear correlation between prognosis and the extentand depth of the burn injury. Therefore, it2 3 BESTPRACTICE GUIDELINES:BEST PRACTICEGUIDELINES: EFFECTIVEEFFECTIVE SKINSKIN ANDAND WOUNDWOUND MANAGEMENTMANAGEMENT OFOF NON-COMPLEXNON-COMPLEX BURNSBURNS
CAUSES OF BURNSCauses of burnsBurns are caused by exposure to thermal (heat), electrical, chemical or radiationsources. Children under 5 years and the elderly are at increased risk of burn injuryCAUSES OF BURN BY AGEChildren account for almost half of the population with severe burn injury and children belowfive years of age account for 50–80% of allchildhood burns20. Burns are the eleventhmost common cause of death in children aged1–9 years and the fifth most common causeof non-fatal childhood injuries. Globally, themajority of children with burns are boys with aratio of 2:1 to girls, and there is a higher mortality rate from burns among boys20.FIGURE 2: Causes of burns by incidence in theUK . Adapted from235%40%Most childhood burns occur in the home;scalds are the most common burn type(accounting for 60–70% of all hospitalisedburn patients), followed by flame and contactburns21,22 (Box 4).FlameThe vast majority of adult burns occur in thehome, outdoors or in the workplace. Theseresult from thermal (scalds, flame, contact),electrical or chemical sources. Other importantcauses include radiation and extreme cold(frostbite).Who is at increased risk?Those most vulnerable to burn injury include:Q ChildrenQ Elderly peopleQ Those with reduced mental capacity, e.g.those with dementia or learning difficultiesand those who may not recognise or reactto a dangerous situationQ Those with reduced mobility and anyonewith sensory impairment, which may prevent a quick response to injury.MECHANISM OF INJURYIt is important to consider the mechanism bywhich a burn was caused, as this influencesthe pathophysiology of the injury and, therefore, how it should be managed.THERMAL BURNSMost burns are thermal injuries and these predominantly comprise scalds and flame injuries(Figure 2)23.Flame injuriesIn developed countries, flame injuries are mostcommonly seen in men and women of workingage (15–64 years). The incidence in children55%ScaldsChemicaland electricaldecreased after legislation restricting thedesign and material of night clothing. Indeveloping countries, flame injuries are themost common form of burn, occurring mainlyin women aged 16–35 years21,22. This groupspends long periods cooking at floor level inloose-fitting clothing, using equipment thatmay be unsafe4,6 (Figure 3).BOX 4: CAUSES OF BURNS BY AGE IN THEUK. ADAPTED FROM23Figure 3: Flame burn wound.Photo courtesyProfessor FranckDuteilleYoung children (1–4 years)Q 20% of all patients with burnsQ 70% due to scaldsQ Boys more likely to be burnt than girls(due to behavioural differences)Older children and adolescents (5–14 years)Q 10% of all patients with burnsQ Teenagers often injured from illicitactivities involving accelerants orelectrocutionFigure 4: Scald burn wound.Photo courtesy Professor FranckDuteilleWorking age (15–64 years)Q 60% of all patients with burnsQ Predominantly flame burnsQ Around 33% work-related incidentsElderly people ( 65 years)Q 10% of all patients with burnsQ At higher risk of scalds, contact burns andflame burns (due to effects of aging, suchas immobility and slowed reactions)Figure 5: Scald burn wound showingtypical map of Africa topography.Photo courtesy André MagnetteBEST PRACTICE GUIDELINES: EFFECTIVE SKIN AND WOUND MANAGEMENT OF NON-COMPLEX BURNS3
CAUSES OF BURNSFlame injuries tend to be of any depth(partial or full thickness — see Definitionsof burn depths, p10) and often a mixture ofdepths.Figure 6: Contact burn wound.Photo courtesy Professor FranckDuteilleFigure 7: Deep dermal contactburn wound. Photo courtesyAndré MagnetteFigure 8: Electrical burn. Photocourtesy Professor FranckDuteilleScaldsScalds are frequently due to spilling of hotdrinks and liquids, and immersion in a hotbath or shower (Figure 4, p3). They accountfor around 70% of burns in children, althoughthey are also common in elderly people.Scalds tend to cause superficial or superficial dermal burns, and may involve a largearea of skin. In children who have pulled ahot liquid onto themselves from a height, atypical ‘map of Africa’ distribution may beseen with a large area of burn at the top anda smaller area underneath (Figure 5, p3).CHEMICAL BURNSBurn injuries from corrosive agents occurmainly in industrial accidents, but theycan also result from products found in thehome.Chemical burns are caused by:Q Acids (e.g. sulphuric, nitric, hydrofluoric,hydrochloric and phosphoric)Q Alkalis/bases (e.g. sodium or potassiumhydroxide, sodium or calcium hypochlorite, ammonia or phosphates, andchemicals in household cleaning agents,bleaches and cement). These tend tocause deeper burns than acidsQ Organic products (e.g. bitumen).Common sources of contact burns includeirons, oven doors, vitro-ceramic cookingstations, radiators and the glass fronts ofgas fires (Figure 6).Chemical burns tend to cause deep dermalor full thickness burns because the tissuescontinue to be damaged until the chemical is completely removed (e.g. by copiousirrigation) (Figures 10–12, p5).ELECTRICAL BURNS4 3 Electrical burns may interfere with thecardiac cycle and cause arrhythmias.Cardiac monitoring should be consideredon admission.Contact burnsContact burns occur either when the skintouches an extremely hot object (oftenseen in industrial accidents) or when ittouches a less hot object for a very longtime. The latter may be seen in people whohave lost consciousness, such as thosewith epilepsy or who misuse alcohol ordrugs, or in elderly people after a fall orblackout.Contact burns tend to cause deep dermalor full thickness burns (Figure 7).Figure 9: Electrical burn. Photocourtesy Professor FranckDuteilleFlash burns (high voltage) occur when aperson is exposed to an arc of high-voltagecurrent, but the current does not actuallyenter the body. The associated heat energycauses superficial burns to exposed bodyparts (such as face, neck, hands and upperlimbs). Ignited clothing may cause deeperburns.Electrical burns occur when electricity flowsthrough the body from an entry point to anexit point. The burn is caused by the heat energy of the electric current damaging tissuealong its path of flow (Figures 8 and 9).The extent of tissue damage is determinedby the voltage of the current:Q Low-voltage (domestic current) burns— Small, deep contact burns are seen atthe entry and exit pointsQ High-voltage burns— Currents of more than 1,000 voltscause extensive deep tissue damageand even limb loss. Currents of morethan 70,000 volts are usually fatal.Be aware of the serious effects of absorption of chemical products from the skin.For example mercury can cause renalfailure even from a small area of local skindamage.PATHOPHYSIOLOGYThe pathophysiology of burn wounds isa slowly evolving process, unlike manyother forms of trauma24. Whatever themechanism, burn injuries cause a localresponse and, in complex burns, a systemicresponse.Local responseThe local response to a burn injury consistsof inflammation, regeneration and repair.A burn may be divided into three zones(Figure 13, p5):BESTPRACTICE GUIDELINES:BEST PRACTICEGUIDELINES: EFFECTIVEEFFECTIVE SKINSKIN ANDAND WOUNDWOUND MANAGEMENTMANAGEMENT OFOF NON-COMPLEXNON-COMPLEX BURNSBURNS
CAUSES OF BURNSQZone of coagulation/necrosis— At the centre of the wound— No tissue perfusion— Irreversible tissue damage due tocoagulation of proteinsQZone of stasis— Surrounds the central zone of coagulation— Decreased tissue perfusion— Some chance of tissue recovery withoptimal managementQSystemic responseIn complex burns of more than 20–30%TBSA, there is also a systemic response dueto the extensive release of inflammatorymediators at the injury site. The effects arefar reaching and include systemic hypotension, bronchoconstriction, a threefold increasein basal metabolic rate and a reduced immuneresponse25.Figure 10: Dry necrotic escharcovered chemical burn. Photocourtesy Professor Franck DuteilleZone of hyperaemia— At the periphery of the wound— Good tissue perfusion— Tissue recovery likely.These zones are dynamic environments. Inthe superficial areas and around the edges,the usual process of repair occurs (ingrowthof capillaries and fibroblasts followed byformation of granulation tissue and scar).After 3–4 days, loss of tissue viability in thezone of stasis (for example, due to delayedor suboptimal management) will cause theburn wound to become deeper and wider.Figure 11: Chemical burn withacid. Such wounds tend to besuperficial and self-limiting.Photo courtesy Professor FranckDuteilleFIGURE 13: Zones of a burn injury (photo courtesy Professor Heinz Rode)Zone of hyperaemiaViable tissueFigure 12: Chemical burn due tosodium hydroxide (caustic soda)a strong alkali. Photo courtesyAndré MagnetteZone of stasisDecreased tissue perfusionObliteration of microcirculation, releaseof mediators — TXA, anti-O2 ischaemicreperfusion injury, increase in localvascular permeabilityCentral zone of necrosisCoagulative necrosisBEST PRACTICE GUIDELINES: EFFECTIVE SKIN AND WOUND MANAGEMENT OF NON-COMPLEX BURNS5
EMERGENCYMANAGEMENTEmergency management ofnon-complex burnsClinicians working in the emergency department or community must be confidentin assessing and managing burn injury to ensure optimal outcomesGENERAL FIRST AIDFirst aid and initial management of the burnsite can limit tissue damage and subsequentmortality26. Emergency management continues to be effective for up to 3 hours after theinitial burn injury.If you are the first on scene responder, thepriorities are to:Q Check that it is safe to approach the patient, call for help and, if appropriate, wearappropriate personal protective equipmentQ Stop the burning process (extinguish anyflames using ‘drop and roll’ or turn off theelectricity supply, as appropriate) andremove the patient to a safe place withfresh air. Remove non-adherent clothingand any potentially restricting jewelleryQ Apply general first aid to cool the burnwound.Cool the burn woundCooling thermal burns with tepid, runningwater (12–18 C) removes heat and preventsprogression of a thermal burn injury andlimits tissue damage27. It can also reducepain, cleanse the wound and minimise swelling. This is effective if performed within 20minutes of the injury occurring16 and shouldbe continued for up to 30 minutes28,29,30.Figure 14: Cling film for dressingburn wounds. Lay on wound toprevent external contamination.Allows inspection of wound, isnon-adherent, conformable andessentially sterile. Photo courtesy Professor Heinz RodeIf water is not available then wet towels/compresses or hydrogels (in adults only)are a second-line alternative31,32, althoughthey may be prohibitively expensive in someregions.Ice or very cold water should be avoidedbecause it causes vasoconstriction and may,paradoxically, deepen the wound27.Chemical burns require longer periods ofcopious irrigation — until the injury no longercauses pain or the pH has been normalised(e.g. by testing with urine pH sticks). Corrosive agents continue to cause tissue damageuntil they are completely removed. Eye injuries should be irrigated copiously with sterilesaline. Diphoterine solution, if available, isa very effective washing agent for chemicalburns33,34.6 3 In some situations an antidote can combat theeffects of the chemical irritant (e.g. calciumgluconate gel will inactivate hydrofluoric acid).Some regions therefore recommend seeking advice from a regional or national toxicology unit.Irrigation of electrical burns is not appropriatebecause the heat damage occurs deep underthe surface of the skin. Water irrigation definitely must not be performed before turningoff the electric power source.Remember: cool the burn, not the patient.Cooling large areas can cause hypothermia,especially in children29. For this reason, donot apply wet soaks or ice packs, or usethese during transit. Patients should becovered with coats, sheets or blankets tokeep them warm.Cover the burnIn most instances, burns should be coveredimmediately after cooling. Covering theburn helps to:Q Prevent bacterial colonisation29,35Q Prevent dessication36Q Relieve pain from exposed nerveendings37.Layers of polyvinylchloride (PVC) film (i.e.cling film, Glad wrap, Saran wrap) formsan excellent emergency dressing for anacute burn injury (Figure 14). The layers offilm must be laid over the burn rather thanwrapped circumferentially, to avoid thepossibility of constriction. If PVC film or acost-effective alternative is not available,then a clean, cotton sheet or similar isappropriate.Cellophane transparent film (made fromregenerated cellulose) can worsen chemicalburns so dressings soaked with water/salineor hydrogels should be used instead, takingcare to avoid hypothermia10.In hot, humid, subtropical climates, burndressings become rapidly saturated andinfected. Burn wounds should therefore beleft exposed, or loosely covered with a cleantowel or moisture-retentive ointment.BESTPRACTICE GUIDELINES:BEST PRACTICEGUIDELINES: EFFECTIVEEFFECTIVE SKINSKIN ANDAND WOUNDWOUND MANAGEMENTMANAGEMENT OFOF NON-COMPLEXNON-COMPLEX BURNSBURNS
EMERGENCYMANAGEMENTDo NOT apply topical antimicrobial creams atthis stage, as they will hinder later assessmentof the wound.RELIEVE PAINPain management in patients with burn injuries is often inadequate. While cooling andcovering the burn gives some relief, opioidsmay be needed initially for pain control.Superficial epidermal burns can be extremely painful (more so than deep wounds)because the nerve endings remain intact butexposed. Medicate with a combination ofparacetamol with a low to moderate potencyopioid at the correct dose. Subsequently,a non-steroidal anti-inflammatory drug issufficient.Patients with partial thickness dermal burnsshould be given intravenous opioids at adose appropriate to body weight10,16,38 orintranasal diamorphine10.Cooling gels (e.g. Burnshield) may be usedto cool the burn and relieve pain in the initialstages16. A full discussion of pain relief aspart of ongoing management is given inManagement of non-complex burn wounds(p17).The tetanus status of the patient shouldbe determined and immunisation given ifindicated39.ASSESSMENT — PRIMARY SURVEYAll burn victims should be evaluated first astrauma patients, using advanced trauma lifesupport guidelines1,29,39. This is often knownas the primary survey, and it aims to identifyand stabilise any life-threatening injuries.The mnemonic ABCDEF indicates the orderof priority for addressing problems (Box 5).For burn victims, there should be a particular emphasis on the airway and breathing.These may be compromised by38:Q Mechanical restriction of breathing (e.g.due to a circumferential deep dermal burnlimiting chest expansion or a burn to thelower part of the face)Q Blast injury (e.g. causing penetration ofthe lung)Q Smoke inhalation (e.g. combustion products causing lung irritation and the effectsof carboxyhaemoglobin).In patients who are clearly well other thanan obviously non-complex burn injury,it is acceptable to move straight to thesecondary survey.Fluid resuscitationEffective fluid resuscitation is the cornerstone of management in major burns. Ifthe burn area is over 15% in adults or 10%in children, intravenous fluids should bestarted as soon as possible on scene (e.g.using the rule of 10, see Box 6), althoughtransfer should not be delayed by morethan two cannulation attempts16,29,37,40.For physiological reasons the threshold iscloser to 10% in the elderly ( 60 years)11.BOX 6: THE RULE OF 101. Estimate burn size to the nearest 102. %TBSA x 10 Initial fluid rate in ml/h(for adults weighing 40-80kg)3. For every 10kg above 80kg, increase therate by 100ml/hVarious resuscitation fluids are availableand there is no ideal regimen to follow.Healthcare professionals should refer tolocal protocols. However, a commonlyused regimen using crystalloid Hartmann'ssolution and the Parkland formula to calculate the volume required is given in Box 7.BURN-SPECIFIC EVALUATION —SECONDARY SURVEYA patient history and physical examination(sometimes known as the secondary survey) should identify issues that impact onthe immediate management of the patientand/or have implications for transfer decisions. The evaluation should determine13:Q Approximate wound size (see Evaluating burn injury: assessing area anddepth, p9)Q Approximate wound depth (see Evaluating burn injury: assessing area anddepth, p9)Q Location of burn injury (including anyinvolvement of the face, eyes, ears,hands, genitals or feet)Q Presence of an inhalation injuryQ Presence of a circumferential deepdermal burn injuryQ The cause of the burn injury (thermal,electrical or chemical)Q Suspicion of abusive injury.BOX 5: PRIMARY SURVEYFOR PATIENTS WITH BURNINJURIESA Airway maintenance withcervical spine controlB Breathing andventilationC Circulation withhaemorrhage controlD Disability — neurologicalassessmentE Exposure — preventinghypothermiaF Fluid resuscitationBOX 7: SUGGESTEDREGIMEN FOR FLUIDRESUSCITATION. ADAPTEDFROM31AdultsResuscitation fluid alone (first24 hours)Q Give 3–4ml (3ml in superficial and partial thicknessburns/4ml in full thicknessburns or those with associated inhalation injury)Hartmann's solution/kgbody weight/%TBSA. Halfof this calculated volume isgiven in the first 8 hours after injury and the remaininghalf in the second 16-hourperiodChildrenResuscitation fluid as aboveplus maintenance (0.45%saline with 5% dextrose, thevolume should be titratedagainst nasogastric feeds ororal intake):Q Give 100ml/kg for thefirst 10kg body weight plus50ml/kg for the next 10kgbody weight plus 20ml/kgfor each extra kgBEST PRACTICE GUIDELINES: EFFECTIVE SKIN AND WOUND MANAGEMENT OF NON-COMPLEX BURNS7
EMERGENCYMANAGEMENTBOX 8: WHERE THERE IS ADELAY IN TRANSFER TO ABURNS SERVICEIf the time from burn to arrival at a burns service is 6hours and the burn is clean:Q Wash burn wound, coverwith plastic cling wrap fortransfer (do not wrapcircumferentially), allowingfor easy assessment atthe burns service withoutundue discomfort fromremoval of dressingsIf transfer is likely to be 6hours or the burn is dirty:Q Dirty or charred burnsshould be washed withsterile water/tap water (depending on local protocol)and dressed with a silverproduct (impregnated silverdressing or topically appliedsilver sulfadiazine cream)Q Clean burns should bedressed with a low-adherent silicone dressingIn addition, the following situations maywarrant special consideration or referraleven if the burn is non-complex:Q Any co-existing medical conditions (e.g.cardiac disease, diabetes, pregnancy orimmune-compromised state)Q Any predisposing factors that mayrequire further investigation or treatment(e.g. a burn resulting from a fit or faint)Q The possibility of non-accidental injuryQ The person’s social circumstances (e.g.an older person living alone).based purely on the size and depth of theburn, and careful assessment of the patientis required41. If there is uncertainty whetherreferral is appropriate, seek specialist advice(Figure 15).When transfer is delayed, ensure the burnis suitably dressed (Box 8) to avoid contamination.Telemedicine and transmission of photographs to the burn unit may help make amore accurate estimate of the burn extent.Therefore admissions criteria
Burns are the eleventh most common cause of death in children aged 1-9 years and the fifth most common cause of non-fatal childhood injuries. Globally, the majority of children with burns are boys with a ratio of 2:1 to girls, and there is a higher mortal - ity rate from burns among boys 20. Most childhood burns occur in the home;