Transcription
J Wound Ostomy Continence Nurs. 2015;42(5):501-524Published by Lippincott Williams & WilkinsCONTINENCE CAREEvidence-Based Skin CareA Systematic Literature Review and the Developmentof a Basic Skin Care AlgorithmAndrea Lichterfeld Armin Hauss Christian Surber Tina Peters Ulrike Blume-Peytavi Jan Kottner ABSTRACTPatients in acute and long-term care settings receivedaily routine skin care, including washing, bathing, andshowering, often followed by application of lotions,creams, and/or ointments. These personal hygiene andskin care activities are integral parts of nursing practice, but little is known about their benefits or clinicalefficacy. The aim of this article was to summarize theempirical evidence supporting basic skin care proceduresand interventions and to develop a clinical algorithm forbasic skin care. Electronic databases MEDLINE, EMBASE,and CINAHL were searched and afterward a forwardsearch was conducted using Scopus and Web of Science.In order to evaluate a broad range of basic skin careinterventions systematic reviews, intervention studies,and guidelines, consensus statements and best practicestandards also were included in the analysis. One hundred twenty-one articles were read in full text; 41documents were included in this report about skin care forprevention of dry skin, prevention of incontinenceassociated dermatitis and prevention of skin injuries. Themethodological quality of the included publications wasvariable. Review results and expert input were used tocreate a clinical algorithm for basic skin care. A 2-stepapproach is proposed including general and specialskin care. Interventions focus primarily on skin that iseither too dry or too moist. The target groups for thealgorithm are adult patients or residents with intact orpreclinical damaged skin in care settings. The goal of theskin care algorithm is a first attempt to provide guidancefor practitioners to improve basic skin care in clinical settings in order to maintain or increase skin health.KEY WORDS: Baths, Cosmetics, Dermatology, Hospital,Long-term care, Nursing, Prevention, Skin, Skin care. IntroductionMaintaining and improving skin health and integrity aremajor goals in acute and long-term care. Skin integrity isregarded as a quality indicator1 and maintaining skinintegrity is widely accepted as being more cost-effectivecompared to wound treatment.2-4 Patients who are critically and chronically ill and those with immobility or incontinence are at risk for developing a broad range ofadverse skin conditions such as pressure ulcers (PUs), incontinence-associated dermatitis (IAD), skin tears, or intertriginous dermatitis (intertrigo).5,6 Due to continuouschanges in skin and underlying soft tissue structure andfunction,7 advancing age can also be regarded as an independent risk factor for developing skin problems. Dry skin(xerosis), fungal infections, and several forms of dermatitisare most prevalent in aged populations in care settings.8-12Thousands of patients receive daily routine skin care,including washing, showering, and bathing with or without the use of skin cleansers. Cleansing is often followedby application of lotions, creams, and ointments. Thesepersonal hygiene and skin care activities are integral partsof nursing practice, but little is known about the benefitsand clinical efficacy of these practices.5,13 Andrea Lichterfeld, MA, Clinical Research Center for Hair andSkin Science, Department of Dermatology and Allergy, Charité–Universitätsmedizin, Berlin, Germany. Armin Hauss, MSc, Clinical Quality and Risk Management,Charité - Universitätsmedizin Berlin, Germany Christian Surber, PhD, Department of Dermatology, University ofBasel and Zurich, Switzerland. Tina Peters, MSc, Clinical Research Center for Hair and SkinScience, Department of Dermatology and Allergy, Charité–Universitätsmedizin Berlin, Germany. Ulrike Blume-Peytavi, MD, PhD, Clinical Research Center for Hairand Skin Science, Department of Dermatology and Allergy, Charité–Universitätsmedizin Berlin, Germany. Jan Kottner, PhD, Clinical Research Center for Hair and SkinScience, Department of Dermatology and Allergy, Charité–Universitätsmedizin Berlin, Germany.The authors declare no conflicts of interest.Correspondence: Andrea Lichterfeld, MA, Charité–UniversitätsmedizinBerlin, Department of Dermatology and Allergy, Clinical ResearchCenter for Hair and Skin Science, Charitéplatz 1, 10117, Berlin,Germany (andrea.lichterfeld@charite.de).DOI: 10.1097/WON.0000000000000162Copyright 2015 by the Wound, Ostomy and Continence Nurses Society J WOCN September/October 2015 501Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.JWOCN-D-15-00006 LR 50125/08/15 5:00 PM
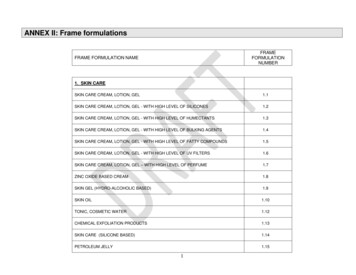
502Lichterfeld et alWe practice in a similar situation at the CharitéUniversitätsmedizin Berlin, one of the largest universityhospitals in central Europe. Multiple skin care productsare used, and skin care routines are based on personal beliefs, preferences, and local care policies rather than current best evidence or consistent best practices. In order toreduce practice variations, we developed a basic skin carealgorithm based on current best evidence and best practices. A quality improvement project was launched. Thisarticle reports results of a systematic literature reviewabout the current best evidence regarding basic skin care.Review results and expert input were then used to create aclinical algorithm for basic skin care in care settings,which is introduced in the second part of this article.Basic skin care was defined as skin cleansing and application of topical products in order to maintain and improve the skin's barrier function and integrity. Commonpractices include washing, bathing, showering with orwithout cleansing products, and application of leave-onproducts such as lotions creams or ointments. We placedspecial emphasis on a preventive approach to skin care.14Application of administration of prescriptive agents wasexcluded from this project. MethodsA systematic literature search was conducted to evaluatethe empirical evidence supporting basic skin care interventions. The electronic databases MEDLINE, EMBASE,and CINAHL were searched ranging from 1995 to 2013.We also completed reference (ancestry) searches of selected publications. After inclusion of publications fromthe database and reference list searches, a forward searchwas conducted using Scopus and Web of Science. Thistechnique allowed us to search forward in time of publication of key articles to ensure a more thorough review.There were no language restrictions.We decided to cover a broad range of basic skin careinterventions in our literature review. We therefore deemedthe following article types eligible for inclusion: (1) systematic reviews; (2) intervention studies; and (3) clinicalpractice guidelines, consensus statements, and best practice standards. Many intervention studies have been included in previous systematic reviews already. If studieshad already been included in a previous review, they werenot included as a single study again. Instead we limitedour review to randomized controlled trials (RCTs) reporting basic skin care treatment effects that were not includedin previous systematic reviews. Editorials, comments, casecontrol studies, and studies focusing on the treatment ofpersons with IAD, skin tears, or PUs were excluded.Study Selection and Data ExtractionTwo reviewers (A.L. and A.H.) independently screened theresults of the database search based on title and abstract.Potentially relevant articles were read in full textJ WOCN September/October 2015independently by the same 2 reviewers; disagreementswere resolved by consensus. The results were methodologically clustered into (1) systematic reviews, (2) RCTs,and (3) clinical practice guidelines, consensus statements,and recommendations. The following characteristics wereextracted: (1) Systematic reviews: authors, review topic,main inclusion criteria, summary of results, and includedstudies (Table 1); (2) RCTs identified during reference reviews: authors, topic/research question, sample, intervention, and main results (Table 2); and (3) Clinical practiceguidelines, consensus statements, and recommendations:source, topic, conclusion, and recommendations aboutskin care (Table 3). Besides the different publication typesidentified, content was then iteratively classified into related topics.The methodological quality of all systematic reviewsand the RCTs included in our review was independentlyrated by 2 reviewers (A.L. and A.H.); disagreements inquality were resolved by consensus. We used a validatedinstrument to evaluate systematic review quality (AMSTAR,Assessing the Methodological Quality of SystematicReviews).15 This instrument consists of 11 items coveringthe design and the conduct of each systematic review, forexample, whether a research question and inclusion criteria were stated a priori, or if a list of inclusion and exclusion criteria was provided. Other questions address, forexample, the characteristics, the scientific quality of theincluded studies, or whether publication bias was assessed.All questions were answered with “Yes,” “No,” “Can'tanswer,” or “Not applicable.” Every “Yes-answer” wasassigned one point, indicating that this quality criterionwas met.Randomized controlled trials included in this reviewwere rated using the Cochrane Collaboration's tool for assessing risk of bias.16 Six possible bias categories (sequencegeneration, allocation concealment, blinding, incompleteoutcome data, selective outcome reporting, and other potential threats to validity) were ranked using “Yes” for lowrisk of bias, “No” for high risk of bias, or “Unclear.”Because of their heterogeneous nature, the methodologicalquality of the guidelines, consensus statements, and recommendations was not formally assessed.Development of the Skin Care AlgorithmAfter evaluation and summary of empirical evidence,recommendations for care, along with consensus statements and a clinical algorithm for basic skin care in aninstitutional care setting, were developed. At first, reviewresults were clustered into similar interventions and activities. These interventions were then ordered accordingto the general care process logic.17 The first draft of ouralgorithm was sent to colleagues with expertise in dermatology (U.B.P.), skin pharmacology/pharmacy (C.S.),nursing science, and basic skin care research (J.K., A.L.),clinical quality and risk management (A.H.). Based onfeedback from these expert colleagues, the algorithm wasCopyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.JWOCN-D-15-00006 LR 50225/08/15 5:00 PM
TABLE 1.JWOCN-D-15-00006 LR 503(1) Use of soap andwater not appropriate;(2) use of structuredperineal skin care; (3)use of products withpH near to normalskin; and (4) use ofskin protectant(1) Use of disposable bodyworns inincontinent patients to protect skin;(2) avoidance of soap, only use ofemollient soap; (3) use of no rinsecleanser with ingredients likeCLINISAN(Synergy Health, UK)reduces risk of pressure ulcer formation; (4) use of bag bath leads toreduction in skin dryness; and (5) zinccream and SUDOCREM (Kyberg Phar.Vert. GmbH, Germany) reduce skinrednessSummary of resultsXX XByers et al (1995)Dealey (1995)Hardy (1996)Mason (1997) XX(1) Adults; (2) studiesdescribing interventions for preventionand treatment of IAD(1) Systematic reviews, randomized ornonrandomized studies; (2) evaluationof nonmedical intervention or program for improvement of skin integrity; (3) age 65 years and over; (4)aged care facility, hospital, or longterm careMain inclusioncriteriaIncluded studiesEffectiveness of interventions for preventionand treatment ofincontinence-associated dermatitis (IAD)Beeckman et al(2009)2Effectiveness of topical skin care interventions for residents of aged carefacilitiesHodgkinson et al(2006, 2007)22Review topicSystematic Reviews (1) Avoidance of frequent washing; (2)use of mild soaps;(3) washing/bathingwith lukewarmwater; (4) pat skindry instead of rubbing; (5) use ofemollients with lowpH directly afterwashing; (6) use oflanolin-free products; (7) skin protection with productsincluding silicons;and (8) applicationof no-rinse cleansersreduces skin tears(1) Skin care andassessment tools;(2) aged humans;(3) healthy skinSkin care for healthyskin in older peopleHaslingerBaumann andBurns (2009)21XX (1) Regular bathing with warmwater (not hot);(2) Not too longsoaking (avoidance of dehydration);(3) Avoidance ofsoap, use ofgently productslike emollients;(4) Soap candamage theskin (alter pH ofskin surface,disturb skinflora); (5) Usesoft cloth(1) Older than 65years; (2) quantitative or qualitative research;(3) skin cleansing interventions; and (4)skin healthmeasuresSkin cleansingpractices forolder peopleCowdell et al(2015)13XX X(1) Syndet (liquid) soaps,bag bath reduced skindryness; (2) moisturizerscontaining humectants(eg, urea, glycerin)reduced dry skin conditions and strengthenedskin barrier; (3) emollients combined withhumectants reduce xerosis; (4) use of specialsoaps, nondetergentcleansers reduces risk forskin injuries; and (5)additionally appliedemollients or barrierproducts promote skinprotection(1) Primary interventionstudies, reporting treatment effect (bathing/cleansing procedure/application of leave-on/rinse-off products/cosmetic products); (2)experimental and observational design; (3) Invivo; and (4) age rangelower limit 50 yearsPrevention of dry skin andskin injuries in agedskinKottner et al (2013)5 (1) Insufficientevidenceabout the useof topicalagents for PUprevention;and (2) 79%PU risk reduction whendressingsapplied overbony prominences(1) Risk of PU; (2)randomizedcontrolled trialscomparing theuse of dressings, topicalagents, or bothPrevention ofpressure ulcersusing dressingsand local applicationsMoore andWebster(2013)3 Lichterfeld et al(continues)3223(1) Use of skin care regimens in incontinenceinstead of soap andwater; (2) soap andwater less effective andmore time consumingthan “pH cleanser” andbarrier cream; and (3)good skin care important for prevention orimproving IAD(1) Older than 65 years ormajority with mean ageof 65 years; (2) homecare facilities; (3)descriptive/ observational or interventionstudies with focus ofmanagement of incontinence, promotion andmaintenance of continence as outcomemeasures; and (4) typeof conditionManagement of incontinence and continencepromotion in older people in care homesFlanagan et al(2014)4J WOCN Volume 42/Number 5503Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
JWOCN-D-15-00006 LR 504 Bates-Jensen et al (2003) Baatenburg de Jong andAdmiral (2004)Wilson and Nix (2005) Hunter et al (2003)Torra I Bou et al (2005)XBirch and Coggins (2003) Thompson et al (2005) Pham et al (2002)Warshaw et al (2002) Lewis-Byers et al (2002)Hoggarth et al (2005) Kuzmina et al (2002) XClever et al (2002) XCooper and Gray (2001) X XX X XX X X X X XX 4/11Cowdell et al(2015)13XXX X XXXXXXXX X X 6/11Kottner et al (2013)5 X 10/11Moore andWebster(2013)3 X X X anet al (2014)4J WOCNZehrer et al (2004a, 2004b) Dawson et al (2001) 3/11HaslingerBaumann andBurns (2009)21Lichterfeld et alBale et al (2004) XSheppard and Brenner (2000)X Draelos (2000)X5/11Beeckman et al(2009)2Schölermann et al (1999)X7/11Whittingham and May (1998)Methodological quality withAMSTAR (max. 11)Hodgkinsonet al(2006, 2007)22Systematic Reviews (Continued )TABLE 1.504 September/October 2015Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
JWOCN-D-15-00006 LR 505 Kalowes (2012)Roure et al (2012)8 Total Elewa et al (2012) Quatresooz et al (2009)Papanas et al (2011) Houwing (2008) Cooper et al (2008)Han (2011) Sloane et al (2007) Nakagami (2007)Beeckmann et al (2011) Welzel et al (2006) Okada et al (2006) Dieter et al (2006)Qiuli (2010) Bliss et al (2006, 2007)Groom et al (2010)7/11Methodological quality withAMSTAR (max. 11)Hodgkinsonet al(2006, 2007)22Systematic Reviews (Continued )TABLE 1.12 XX5/11Beeckman et al(2009)23 3/11HaslingerBaumann andBurns (2009)215 4/11Cowdell et al(2015)1329X XX X XX XX XX X6/11Kottner et al (2013)56 X X X X X 10/11Moore andWebster(2013)33 7/11Flanaganet al (2014)411111111111111112Total(n)J WOCN Volume 42/Number 5Lichterfeld et al505Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
Efficacy of ammoniumlactate 12% lotionvs liposome basedmoisturizing lotionfor plantar xerosisN 57Loss of follow-up:n 14Mean age: 42 yDuration: 6 wksIntervention: Twice-dailyapplication ofammonium lactate12% lotion andliposome-basedmoisturizing lotion onleft or right footOutcomes: (1) xeroticgrade, (2) clinicalevaluation (1 worse to 6 clear)SourceUy et al(1999)40Sample/InterventionN 70Loss of follow-up:n 31Mean age 48 yDuration: 4 wksIntervention: Twice-dailyapplication of 5%salicylic acid and 10%urea and 12%ammonium lactate onleft or right footOutcomes: (1) Xerosisseverity scoreTopicJWOCN-D-15-00006 LR 506Jennings et al Efficacy of 5% salicylic(1998)56acid and 10% ureavs 12% ammoniumlactate fortreatment of footxerosisYesSequence(1) Decrease in mean xeroticUncleargrade of ammonium lactatelotion and liposomemoisturizing lotion(baseline: 2.3 to week 4:0.80; P .001);(2) Clinical evaluation: Mean4.7 (ammonium) and 4.6(liposome) week 4; mean3.7 (ammonium) and 3.5(liposome) week 6; nodifferences between groups(1) Decrease in xerosis severityscore after 4 weeks (week 0:2.4, week 4: 1.0; P .15),no differences betweengroupsMain ResultsAdditional Randomized Controlled Trials Not Included in Systematic ReviewsTABLE 2.AllocationYesYesBlinding Participants/PersonnelYesYesRisk of BiasUnclearUnclearBlinding -dailyapplication ofeither creamreduces skindryness on feet.InterpretationLichterfeld et alJ WOCN(continues)Unclear Twice-dailyapplication ofeither lotionreduces xerosisand hyperkeratosison feet.Yes506 September/October 2015Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
Effect of 2.5%dexpanthenol onexperimentallydamaged skinGehring andGloor(2001)27SourceEffect of topicalapplieddexpanthenol onepidermal barrierfunction andstratum corneumhydration(1) Drug-free vehicle(placebo),(2) vehicle and 6%borage oil,(3) vehicle 6%borage oil and2.5%dexapanthenol,(4) vehicle and 2.5%dexapanthenol, (5)vehicle and 1%dexapanthenolTopicJWOCN-D-15-00006 LR 507Gehring andGloor200026Risk of BiasMain ResultsSample/InterventionYesAllocation(1) Increase in SCH for placebo Unclear Unclear Unclear UnclearN 40and dexpanthenol vsLoss of follow-up: n. r.untreated skin (P .01)Mean age: 34.6 y(2) Decrease on TEWL inDuration: 5 ddexpanthenol vs vehicleIntervention: Applicationand untreated skin (P of 50-μl study product.05)5 times daily 30 min(3) Decrease of inflammationafter washing testfor dexpanthenol vs vehicleOutcomes: (1) stratum(P .01) and untreated skincorneum hydration; (2)(P .05)TEWL; and (3) antiinflammatory effectBlinding Participants/PersonnelYesCompleteness(1) Improvement of stratumUnclear Unclear Unclear UnclearN 60corneum hydration (P Loss of follow-up:.001) with vehicle alone;n 0additional improvementMean age: 37.8 ywith dexpanthenol (P .01Duration: 1 wkvs untreated; P .05 vsvehicle)Intervention: Twice-dailyapplication of 200-μl (2) Decrease of TEWL (P .05)study product on volarfor formulation withforearm vs placebodexapanthenol comparedto placebo groupOutcomes: (1) Stratumcorneum hydration, (2)TEWLSequenceAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )Blinding OutcomeTABLE lear Application of 2.5%dexpanthenolstabilizedepidermal barrierfunction and hashydrating andanti-inflammatoryeffects.Unclear Twice-dailyapplications ofdexpanthenolmaintainepidermal barrierfunction.J WOCN Volume 42/Number 5Lichterfeld et al507Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
Effects of 3 bathadditives(BALMANDOL(Spirig PharmaGmbH(Switzerland),EUCERIN(Bayersdorf AG(Germany),EUCERIN(Bayersdorf AG(Germany),BALNEUM (AlmirallHermal GmbH(Germany)), on skinbarrier functionHill andEdwards200244SourceEffectiveness of 40%urea and 12%ammonium lactatein the treatment ofxerosisTopicJWOCN-D-15-00006 LR 508Ademolaet al(2002)23Sample/InterventionN 20Loss of follow-up: n. r.Mean age: 42.8 yDuration: 2 dIntervention: Applicationof randomized testproducts on the rightand left arm on 2 daysOutcomes: (1) TEWLN 25Loss of follow-up:n 7Age: range 18-65 yDuration: 28 dIntervention: Twice-dailyapplication of testproductsOutcomes: (1) TEWL,(2) scaliness,(3) roughness, and(4) SCHMain ResultsRisk of BiasYesAllocation(1) Mean TEWL: 24Unclear Unclear Unclear Unclear(BALMANDOL (SpirigPharma GmbH(Switzerland)), 22 (EUCERIN(Bayersdorf AG (Germany)),21.5 (BALNEUM (AlmirallHermal GmbH (Germany))17 (Water) at baseline; 18(BALMANDOL (SpirigPharma GmbH(Switzerland)), 22 (EUCERIN(Bayersdorf AG (Germany)),20 (BALNEUM (AlmirallHermal GmbH (Germany))18 (Water) after 120 minGreater effect of BALMANDOL(Spirig Pharma GmbH(Switzerland), on barrierfunction (P .05) AUCTEWL vs TimeBlinding Participants/PersonnelYesCompletenessUnclear Unclear Unclear Unclear(1) Mean TEWL of 40% ureawas lower than inammonium lactate(P .05) at day 28(2 and 3) Improvement of 40%urea cream in skinroughness, fissures,thickness, dryness (P .05)compared to 12%ammonium lactate(4) Increase in SCH for bothgroupsSequenceAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )TABLE 2.Blinding ld et alJ WOCN(continues)Unclear BALMANDOL (SpirigPharma GmbH,Switzerland) had agreater effect onskin barrierfunction thanBALNEUM(Almirall HermalGmbH, Germany)and EUCERIN(Bayersdorf AG,Germany).Unclear Twice-dailyapplication ofeither creamreduces xerosis,but 40% urea wassuperior to 12%ammoniumlactate.508 September/October 2015Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
TopicSourceJennings et al Effect of LACTINOL(2002)62(Pedinol Pharmacal,Inc. (USA)) vs LACHYDRIN (BristolMyers Squibb Co.(Germany)) 12% inmild to moderatefoot xerosisSample/Intervention(1) Decrease in mean xerosisN 53severity score in bothLoss of follow-up:groups (baseline: 2.5; weekn 184: 0.8); “both showMean age: 50 yreduction in skin dryness”Duration: 4 wks(p. 148), (2) n. r., (3) n. r.(4) Lactinol-group: heatIntervention: Treatment(n 0), burning (n 2),of test products on leftpruritus (n 3), erythemaor right foot(n 3); Lac-Hydrin-group:Outcomes: (1) xerosisheat (n 1), burningseverity score, (2)(n 3), pruritus (n 1),tenderness, (3)erythema (n 1), (5) nopruritus, (4) adversedifferences in both groupsevents, and (5) overall(mean overall evaluation:evaluation ofboth groups 0.8)treatment (score:5 worse, 4 noimprovement, 3 slight improvement,2 moderateimprovement, 1 good improvement,0 clear)Main ResultsAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )Blinding Participants/PersonnelAllocationRisk of BiasUnclear Unclear Unclear UnclearSequenceJWOCN-D-15-00006 LR 509Blinding OutcomeTABLE ntinues)Unclear Treatment of eitherlotion reduces footxerosis.J WOCN Volume 42/Number 5Lichterfeld et al509Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
Efficacy of virgincoconut oilcompared withmineral oil fortreatment of mild tomoderate xerosisAgero andVeralloRowell200424SourceEfficacy of 5%dexpanthenol inskin protectionTopicJWOCN-D-15-00006 LR 510Biro et al(2003)59Sample/InterventionN 34Loss of follow-up:n 0Age range: 16-70 yDuration: 2 wksIntervention: Twice-dailyapplication of coconutoil (CO) or mineral oil(MO) on legsOutcomes: (1) Skinhydration, (2) skinlipids, (3) pH, (4)TEWL, (5) skinsymptoms (dryness,scaling, roughness,pruritus, grade ofxerosis)N 25Loss of follow-up:n 4Age: range 18-45 yDuration: 26 daysIntervention: Twice-dailyapplication of testproducts on left andright forearmsOutcomes: (1) Sebum,(2) SCH, (3) pHMain ResultsMean changes in values: (1) 8(mineral oil, MO),10 (coconut oil CO),(2) 75.22 (MO), 96.88 (CO),(3) 0.11 (MO), 0.39 (CO),(4) 8.47 (MO), 3.98(CO), (5) dryness: 15 (MO),19.13 (CO), Scaling: 15.94(MO), 17.33 (CO),Roughness: 14.33 (MO),19,94 (CO), Pruritus: 17.61(MO), 17.43 (CO), Grade ofxerosis: 0.78 (MO), 0.94 (CO)Improvement in skin hydrationin both groups(1) 3 μg/cm2 (dexpanthenol andvehicle) day 0; 12 μg/cm2(dexpanthenol), 11 μg/cm2(vehicle) day 22; 4 μg/cm2(dexpanthenol), 3.5 μg/cm2(vehicle) day 2(2) 70 (dexpanthenol),75 (vehicle) day 0;58 (dexpanthol), 70(vehicle) day 26(3) 5.1 (dexpanthenol),5.0 (vehicle) day 0;4.8 (dexpanthenol),4.9 (vehicle) day 26Blinding Participants/PersonnelAllocationRisk of BiasYesYesYesYesUnclear Unclear Unclear UnclearSequenceAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )TABLE 2.Blinding tionOtherNoLichterfeld et alJ WOCN(continues)Twice-dailyapplication ofeither oilsimproved skinhydration and skinsurface lipid levels.Subjective gradingpatients favorcoconut oil.Unclear Twice-dailyapplication of 5%dexpanthenolexhibits protectiveeffects againstskin irritation.510 September/October 2015Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
SourceLoden et al(2004)45TopicDifferences in theirritation potentialof 8 shower or bathoils (1) E45EMOLLIENT BATHOIL (ReckittBenckiser (UK) Ltd),(2) ACOSHOWER&BATH OIL(ACO Hud AB(Sweden)), (3) ACOINTIMATE WASHOIL (ACO Hud AB(Sweden)), (4)CERIDAL BATH OIL(Stiefel LaboratoriesIreland Ltd(Ireland)), (5)BALNEUM HERMAL(Almirall HermalGmbH (Germany)),(6) SEBAMED,SHOWER OIL(Sebapharma GmbH& Co. Boppard(Germany)) (7)NIVEA SHOWER OIL(Nivea (Germany)),(8) PH 5 EUCERINSHOWER OIL(Beiersdorf(Germany)).Sample/InterventionN 15Loss of follow-up:n 0Age range: 23-57 yDuration: 2 dIntervention: Applicationof test products onvolar forearm withchambers over 24 hOutcomes: (1) TEWL, (2)skin blood flow, (3)visual scoringBlinding Participants/PersonnelAllocationRisk of Bias(1) and (2) SEBAMED, SHOWER Unclear Unclear Unclear UnclearOIL (Sebapharma GmbH &Co. Boppard (Germany)),NIVEA SHOWER OIL (Nivea(Germany))and PH 5EUCERIN SHOWER OIL(Beiersdorf (Germany))increased TEWL and bloodflow, BALNEUM HERMAL(Almirall Hermal GmbH(Germany)) showed higherTEWL compared to water;E45 EMOLLIENT BATH OIL(Reckitt Benckiser (UK) Ltd),ACO SHOWER&BATH OIL(ACO Hud AB (Sweden))andACO INTIMATE WASH OIL(ACO Hud AB (Sweden))showed not higher valuesthan water; (3) Waterinduced very weakerythema, no significantdifferences between testproductsMain ResultsAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )SequenceJWOCN-D-15-00006 LR 511Blinding OutcomeTABLE ontinues)Unclear Results showed alarge difference inirritation potentialbetween products.J WOCN Volume 42/Number 5Lichterfeld et al511Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
SourceBuraczewskaet al(2007)42TopicEffect of long-termtreatment withmoisturizers onbarrier function ofnormal skin(1) Ordinary cream,(2) cream withhydrocarbonsisohexadecane andparaffin,(3) vegetabletriglyceride oil,canola oil(4) Vegetabletriglyceride oil,canola oil withurea, (5) lipid-freegel with polymerSample/InterventionN 78Loss of follow-up: n. r.Age range: 25-60 yDuration: 7 wksIntervention: Twice-dailyapplication of testproducts on volarforearmOutcomes: (1) TEWL, (2)blood flow, (3) skincapacitance (onlyundamaged skin)(1) Cream with hydrocarbonsisohexadecane and paraffin,vegetable triglyceride oil,canola oil and canola oilwith urea, and lipid-free gelwith polymer increasedTEWL, complex creamdecreased TEWL; (2)unchanged to baseline; (3)cream with hydrocarbonsisohexadecane and paraffindecreased skin capacitance,unchanged in the otherpreparationsMain ResultsAdditional Randomized Controlled Trials Not Included in Systematic Reviews (Continued )TABLE 2.Blinding Participants/PersonnelAllocationRisk of BiasUnclear Unclear Unclear UnclearSequenceJWOCN-D-15-00006 LR 512Blinding herLichterfeld et alJ WOCN(continues)Unclear Twice-dailyapplication ofmoisturizersinfluences skinbarrier function,but the influencedepends on thecomposition of themoisturizer.512 September/October 2015Copyright 2015 Wound, Ostomy and Continence Nurses Society . Unauthorized reproduction of this article is prohibited.25/08/15 5:00 PM
N 15 females withxerosis of the feetLoss of follow-up: n. r.Mean age: n. r. (adult)Duration: 14 dIntervention: Twice-dailyapplication of 2moisturizers (left andright foot))Outcomes: (1) SkinhydrationSourceBaalham et al Effectiveness of 2(2011)37moisturizer(AQUEOUS CREAM;PinewoodLaboratories Ltd,Ireland) and CCSFOOT CARE CREAM(EC De Witt & CoLtd, England) onxerosis of the feetTopicN 132Loss of follow-up:n 22Age range: 16-65
skin care. Interventions focus primarily on skin that is either too dry or too moist. The target groups for the algorithm are adult patients or residents with intact or preclinical damaged skin in care settings. The goal of the skin care algorithm is a fi rst attempt to provide guidance for practitioners to