Transcription
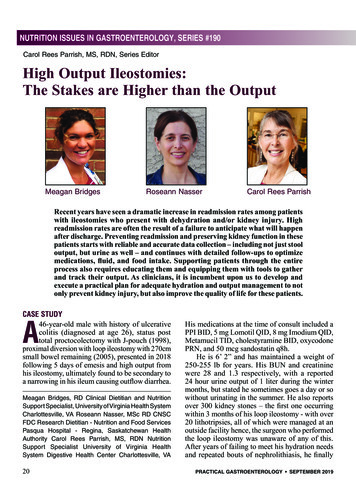
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #190Carol Rees Parrish, MS, RDN, Series EditorHigh Output Ileostomies:The Stakes are Higher than the OutputMeagan BridgesRoseann NasserCarol Rees ParrishRecent years have seen a dramatic increase in readmission rates among patientswith ileostomies who present with dehydration and/or kidney injury. Highreadmission rates are often the result of a failure to anticipate what will happenafter discharge. Preventing readmission and preserving kidney function in thesepatients starts with reliable and accurate data collection – including not just stooloutput, but urine as well – and continues with detailed follow-ups to optimizemedications, fluid, and food intake. Supporting patients through the entireprocess also requires educating them and equipping them with tools to gatherand track their output. As clinicians, it is incumbent upon us to develop andexecute a practical plan for adequate hydration and output management to notonly prevent kidney injury, but also improve the quality of life for these patients.CASE STUDY46-year-old male with history of ulcerativecolitis (diagnosed at age 26), status posttotal proctocolectomy with J-pouch (1998),proximal diversion with loop ileostomy with 270cmsmall bowel remaining (2005), presented in 2018following 5 days of emesis and high output fromhis ileostomy, ultimately found to be secondary toa narrowing in his ileum causing outflow diarrhea.AMeagan Bridges, RD Clinical Dietitian and NutritionSupport Specialist, University of Virginia Health SystemCharlottesville, VA Roseann Nasser, MSc RD CNSCFDC Research Dietitian - Nutrition and Food ServicesPasqua Hospital - Regina, Saskatchewan HealthAuthority Carol Rees Parrish, MS, RDN NutritionSupport Specialist University of Virginia HealthSystem Digestive Health Center Charlottesville, VA20His medications at the time of consult included aPPI BID, 5 mg Lomotil QID, 8 mg Imodium QID,Metamucil TID, cholestyramine BID, oxycodonePRN, and 50 mcg sandostatin q8h.He is 6’ 2” and has maintained a weight of250-255 lb for years. His BUN and creatininewere 28 and 1.3 respectively, with a reported24 hour urine output of 1 liter during the wintermonths, but stated he sometimes goes a day or sowithout urinating in the summer. He also reportsover 300 kidney stones – the first one occurringwithin 3 months of his loop ileostomy - with over20 lithotripsies, all of which were managed at anoutside facility hence, the surgeon who performedthe loop ileostomy was unaware of any of this.After years of failing to meet his hydration needsand repeated bouts of nephrolithiasis, he finallyPRACTICAL GASTROENTEROLOGY SEPTEMBER 2019
High Output Ileostomies: The Stakes are Higher than the OutputNUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #190Table 1. Readmission and Dehydration and/orAKI in Patients with IleostomiesDehydrationYear CitationN&/or AKI*1510719%2001 Beck-Kaltenbach2002 Hallböök1622232%2012 7%16%2013 Paquette2120117%2014 3%11%9%2015 Villafranca264330%2016 LiOrcutt288410417%14%2017 Iqbal29Fish302311365%41%2018 Justiniano3126237%1734* Does not include ER visits/admissions at outside facilitieslost his left kidney. During this admission, it wasdetermined that he needed 3 L of IV fluids nightlyto prevent dehydration and to protect his remainingkidney.INTRODUCTIONCases like the one above are not uncommon amongpatients with ileostomies. As Table 1 shows, recentyears have seen a growing focus on readmissionrates for dehydration and/or acute kidney injury(AKI) among this population (possibly as a resultof stipulations in the Affordable Care Act aimedto decrease hospital readmissions in general).1New ileostomy patients are often sent homewell hydrated from IV fluids while admitted andwith minimal output owing to decreased post-opappetite and intake, but this often does not reflectwhat will happen after discharge when patients areleft to hydrate themselves and their appetite andoral intake picks up. In one study, it was shownthat patients readmitted for AKI presented with aPRACTICAL GASTROENTEROLOGY SEPTEMBER 2019 Table 2. The Clinical Burdenof High-Output Ileostomies Low urine output Dehydration ElectrolyteImbalances Nephrolithiasis AKI CKD Dialysis Fatigue Frequent leakages Peristomal skincomplications Social isolation Reduced physical activity Depression Overall well-being3-fold increase in ileostomy output between postop discharge and readmission (an average of 13days later).2 Another study found that patients hadsignificantly decreased GFR at ileostomy closurecompared to pre-op ileostomy creation for anycause.3 Finally, Li et al. showed that 25% of patientswith ileostomies develop CKD within 2 years,likely due to recurrent, sub-clinical dehydration.4As clinicians, we are tasked with interveningnot only to prevent kidney injury, but also to easethe other clinical and psychological burdens as wellas quality of life challenges that so many patientswith high-output ileostomies face (Table 2).High Output DefinedAs Table 3 shows, there can be many causes of highoutput, which in turn may lead to dehydration andkidney injury. A normal, mature ileostomy shouldonly make about 1200mL of output each day (Table4). Jejunostomies can initially put out up to 6 L, butthis too will decrease with the help of medication.On the other hand, colostomies usually only putout 200-600mL/day. In the literature, “high output”is loosely defined as 1500mL/day.Acute Kidney Injury and DehydrationAs of 2011, expanded guidelines have beenproposed based on serum creatinine levels andurine volume, widening the scope of what itmeans to have an AKI (Table 5). Dehydration,however, is a bit more nebulous. While there is nosingle way to define it, one of the best indicatorsis whether a patient is able to make enough urine( 1200mL/ day). Other indicators are listed inTable 6. Note that dark urine can sometimes be aside effect of a particular medication, rather thana sign of dehydration. Make sure to ask patients21
High Output Ileostomies: The Stakes are Higher than the OutputNUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #190#190if they have ever been admitted for dehydration(whether at your own or another outside facility)and/or been to the emergency department andreceived IV fluids or experienced a kidney stone.Treating and Preventing Dehydration:What to Do When an Ileostomy Patientis ReadmittedTreatment for dehydration will look different inileostomy patients vs. those without ileostomies.In addition to fluid resuscitation with IV fluids,high output ileostomy patients are often told todrink more by mouth. Drinking more, however,does not mean absorbing more fluid and in fact, insome, will drive ileostomy losses further, resultingin even worse dehydration or volume depletion.In patients suffering from ongoing malnutrition,sweetened liquid nutrition supplements (such asEnsure/Boost, etc.) are often recommended, butthese too are known to drive stool losses in thosewith high output. Some patients may notice that ifthey drink less fluid, their bothersome ileostomyoutput decreases, but then so does their urineoutput, often to a volume well below a liter perday. Unfortunately, while many patients are taughtto record their stool or ileostomy volume, mostare not educated to measure urine also, and thisis the most important guide to hydration in thesepatients. Stool or ileostomy output may look great,but it may come at the expense of an adequate urineoutput, which may ultimately result in renal demiseand chronic kidney insult.Data CollectionImportance of Ins and Outs (I&O)For dehydrated, high output ileostomy patients,the first step is to ascertain the patient’s true GIanatomy (if not known). If the operative reportis unclear, consider ordering an abdominal CT todetermine a patient’s anatomy and/or the presenceof any strictures. If this is not an option, a smallbowel follow-through can help determine grossanatomy and transit time through the GI tract.For an accurate 24-hr I&O while an ileostomypatient is admitted, an order for “Strict or MeasuredI&O” vs. just “I&O” will ensure greater accuracy–i.e., not just if/when the patient stooled or emptiedtheir ileostomy bag, but the actual volume of eachoccurrence. In many cases, it is worth having a22 Table 3. Possible Causes of High Ileostomy Output Short bowel syndrome (SBS) Poor quality of remaining bowel(acts like SBS) Intraabdominal sepsis Enteric infection(C. diff, salmonella, etc.) Carcinoid Proximal stomas / small bowel fistulas Recurrent / active disease(e.g. Crohn’s flare) Medication initiation or steroid withdrawal “Outflow” diarrhea from stricture/obstructive processdiscussion with the nursing staff to clarify thedifference between I&O and Strict I&O. It is alsovery important that both floor and wound andostomy nurses document if a patient’s ostomy isleaking, or bursting, so all know that the ostomyvolume recorded in the medical record is less thanwhat the losses really are. In general, goal urineoutput should be around 1200mL (or in the case ofkidney stone formers, at least 1500mL) each day.Ideally, a goal stool output should be 1500mL/ day,not just to reduce the risk for dehydration, AKI orkidney stones, but also to improve the patient’soverall quality of life. Providing patients with thetools to measure both urine and ostomy output isessential (see Figures 1-4).SodiumPatients with high ostomy output are at risk forsodium depletion as jejunal and ileal effluentcontain 80-140mEq sodium per liter respectively.It will be important to provide enough sodium inthe patients IV fluids to reflect this and adjust asthe output is brought down under control. Oneway to determine if your patient is sodium repleteis to obtain a 24 hour or random urine Na level; 10mmol/L suggests Na depletion.5,6Osmotic vs Secretory DiarrheaSome patients who present with high outputwill require differentiating between osmotic and(continued on page 24)PRACTICAL GASTROENTEROLOGY SEPTEMBER 2019
High Output Ileostomies: The Stakes are Higher than the OutputNUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #190(continued from page 22)secretory diarrhea. These patients will need tobe NPO for 24 hours with IV fluids and possiblyparenteral nutrition (PN), if also malnourished. Ifileostomy output significantly drops during thistime, then it is osmotic in nature and can at leastbe partially managed by reducing food and/or fluidintake (and replacing with IV fluids as needed).The added benefit of this approach is that yourpatients will be able to see for themselves howeating and drinking directly drive output. If, on theother hand, ileostomy output remains over 500800mL/24 hours, then it is considered a secretorydiarrhea and will require a different medicationand treatment approach.Determining a Malabsorptive ComponentIf you suspect malabsorption, collect a 48-72 hourfecal fat to determine the degree. A patient withsevere malabsorption may require PN, whereasa patient with mild to moderate malabsorptionmay see enough improvement with diet/beveragechanges, along with antidiarrheal and antisecretorymedications. For younger patients, a 48-hour sampleis usually sufficient, but Medicare beneficiaries willneed to complete a 72-hour collection. Whichevertest you use, ensure that your patients are ingesting/infusing 100 g fat per day either orally or enterally.A patient cannot malabsorb fat if they do not ingestit.short bowel syndrome. Our clinical experience,however, suggests that these patients may benefitfrom a “relative” short bowel diet, at least until theiroutput is well under control. In general, this diet ishigh in complex carbohydrates and low in sugaralcohols (contained in many liquid medications7),sugar, and sugary beverages (Table 7).8-11 Thosewith an end jejunostomy or ileostomy will needadditional salt. Once a patient’s output is undercontrol, it is important to begin liberalizing thediet as tolerated to avoid unnecessary restrictionsand potential nutrient deficiencies.Overall fluid intake is patient-specific. Ingeneral, hypertonic fluids, which pull waterinto the small bowel and thereby increase stoolvolume, should be avoided altogether.12 Thisincludes fruit juice/drinks, regular sodas, sweettea, syrup, ice cream, sherbet, sweetened gelatin,and liquid nutrition supplements such as Ensure,Boost or store brand equivalents. Small amountsof hypotonic fluids, such as water, tea, coffee,alcohol, and diet sodas, are allowed. However,bear in mind that hypotonic fluids will pull sodiuminto the small bowel; sodium in turn will pull waterTable 4. Normal Ostomy Output Expected Patients Need to Know This§ Ileostomy: 1200mL (mature 600-800mL)§ Jejunostomy: up to 6 liters§ Colostomy: 200-600mLFood and Fluid ConsiderationsThere is limited data on specialized diets forileostomy patients other than those with knownNightingale JM (Ed). Intestinal failure. Greenwich MedicalMedia Limited. London, England, 2001.Table 5. Acute Kidney Injury Defined32Stage Serum Creatinine24 Urinary OutputExamples of Expected Urinary Volume11.5-1.9 x baselineOR 0.3 mg/dL 0.5 mL/kg/hr for6-12 hrs60 kg female 180-360 mL70 kg male 210-420 mL22.0-2-2.9 x baseline 0.5 mL/kg/hrfor 12 hrs60 kg female 360 mL70 kg male 420 mL33.0 x baselineORIncrease to 4.0 mg/dLORInitiation of CRRT 0.3 mL/kg/hrfor 24 hrsORAnuria for 12 hrs60 kg female 432 mL70 kg male 505 mLPRACTICAL GASTROENTEROLOGY SEPTEMBER 2019
High Output Ileostomies: The Stakes are Higher than the OutputNUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #190with it, thereby increasing stool volume as well.Initially, a drastic fluid restriction (e.g. 120mLwith meals plus sips of water with meds for 24hours) can be a powerful demonstrator to thepatient regarding just how much oral fluids candrive output. Remember that all patients will stillneed to maintain a urine output of at least 1200mL/day;
ostomy nurses document if a patient’s ostomy is leaking, or bursting, so all know that the ostomy volume recorded in the medical record is less than what the losses really are. In general, goal urine output should be around 1200mL (or in the case of kidney stone formers, at least 1500mL) each day.