Transcription
RESPIRATORYMEDICINE(1998)92, 70-75Characteristicsand complaints of patientsprescribed long-term oxygen therapy in theNetherlandsM.J. KAMPELMACHER’, R. G. VAN KESTEREN”, G. P. J. ALSBACH , C. F. MELISSANT*,H. J. WYNNE’, J. M. C. DOUZE” AND J-W. J. LAMMERS*“Centue for Home Mechanical Ventilation, Division of Internal Medicine and Dermatology,‘Division of Obstetrics and Gynaecology and *Department of Ptllmonavy Diseases,Heart-LungInstitute, University Hospital Utrecht, and ‘Cent, fov Biosfatistics, University of Utrecht, Utrecht,The NetherlandsIn patients prescribed long-term oxygen therapy (LTOT), compliance is often poor. Both patient- and treatmentrelated factors seem to be involved. As a base for improvements in LTOT, the characteristics and complaints ofLTOT patients were investigated.A survey was set up in a random sample of clients of the largest oxygen company in the Netherlands. Patients wereselectedif they were 2 18 years old, had a phone and if they had had oxygen equipment for 2 6 months, All patientswere visited at home by a medical student. Data are presented for a total of 528 patients (response rate 62%). Thetypical LTOT patient was a 70-year-old male with chronic obstructive pulmonary disease (COPD), who had hadoxygen equipment for 3.5 years and who used oxygen cylinders and nasal cannulae for 13 h day- i. Twenty percentof the patients still smoked. Although LTOT was prescribed in 80% of the patients by a chest physician, prescriptionwas often inadequate. Only 33% of the patients were informed adequately about the therapy. Twenty percent of thepatients used oxygen for fewer hours per day than prescribed. Non-compliant patients were mainly men (P O.O06)and more often ashamed of their therapy (P O.O23)than compliant patients. The blood oxygen level was monitoredregularly in 73% of the patients. Most complaints concerned the oxygen equipment, especiallythe concentrator. Thesingle most important complaint had to do with restricted autonomy. Only 19% of the patients had no complaintsat all.It is concluded that LTOT should be improved with regard to the education, motivation and monitoring ofpatients. The prescribing physician needs to be included in an education programme. Given the numerous problemsthese patients experience, LTOT should be improved in particular with regard to equipment convenience.RESPIR. MED.(1998)92, 70-75IntroductionIn patients with chronic obstructive pulmonary disease(COPD) and chronic hypoxaemia, long-term oxygentherapy (LTOT) improved survival and reduced clinicaldeterioration over a 3-year period (1,2). An effect was onlydemonstrated if oxygen was used for at least 15 h day - ‘,with greater benefit for longer periods. International guidelines, therefore, recommend the prescription of 15 h day- ias a minimum (3,4). However, if LTOT is prescribedaccording to these guidelines, it imposes a considerableReceived24 September1996 and acceptedin revisedform4 February1997.Correspondenceshould be addressedto: M. K. Kampelmacher,Centre for Home MechanicalVentilation, HP BOO.118,UniversityHospitalUtrecht,P.O.Box 85500,3508 GAUtrecht,TheNetherlands.0954 6111/98/010070 06 12.00/Oburden on many patients. Consequently, compliance totreatment is poor (5-7). Compliance may, amongst otherfactors, be affected by patient characteristics, such as motivation and severity of diseasesymptoms, information aboutthe disease and the therapy, and, especially, by the perceived discomfort of the treatment itself (5-8). Attempts toimprove compliance should, therefore, be based on knowledge of the characteristics and the complaints of thesepatients.In 1991, data on the characteristics and complaints ofLTOT patients in the Netherlands were lacking. At thesame time, relevant epidemiological data in the literatureoften originated from (chest) physicians instead of patients,contained only a small number of patients, and differedfrom country to country (9-12). Moreover, studies lookinginto the complaints of LTOT patients were scarce. This allled to the aim of the present study, namely to investigate thecharacteristics and complaints in patients who had been01998 W. B. SAUNDERSCOMPANYLTD
PROFILETABLE 1. Patient-reporteddiagnoses and prescribingDiagnosisCPCOPDPneumoconiosisCluster headacheCardiovasculardiseasesPulmonary fibrosisLung cancerDyspnoeaPulmonary emboliCystic fibrosisThoracic cage deformitySclerodermiaOtherNo diagnosis %)(50%)(100%)(100%)(100%)All patients421 (80%)33 (89%)17 (77%)CP, chest physician; NCP, non-chestpulmonary disease.physician;prescribed LTOT in the Netherlands.These data mightallow for comparisonswith data of LTOT patients inother countries, and could possibly serve as a base forimprovementsin LTOT.MethodsTo avoid biased patient selection, a survey was set up in asample of 4500 clients of the largest oxygen company in theNetherlands(Hoek Loos). For reasons of travelling distances, the file was restricted to 2523 patients. After theyhad been coded by number, 1381 of them were randomizedby computer. The selection criteria were: (a) being 2 18years old; (b) having a phone; and (c) having oxygenequipment for 26 months. Eligible patients received anexplanatoryletter together with a reply card from theoxygen company. The name and phone number of a patientwere only handed to the investigators if the card stated apositive reply. The patient was then phoned to arrange ahome visit by a medical student. All patients were visitedbetween 1 October, 1991 and 1 April, 1992.Prior to the visit, 15 students had been trained informulating the 145 questions of a structured questionnaire,which referred to demographic data, the prescribing physician, the illness, smoking habits and mobility. Prescription,usage, equipment,follow-upand coping with treatmentwere examined in detail. Students were instructed that allquestions had to be answered by the patients themselves.To estimate the representativeness of the patient sample,the oxygen companywas requested to complete twoadditionalquestionnaires.One for the patients who hadbeen interviewed and given informed consent, and one forthe patients who had refused the interview. The formerquestionnaire only referred to the amounts of daily oxygenprescribed and used, whereas the latter also referred to age:diagnosis, sex, durationof LTOT, smoking habits andphysiciansANDOFLTOTPATIENTS71(n 10%)(22%)(8%)(33%)(9%)2 (50%)3 (100%)1 (3%)2 (9%)49 (9%)GP, general practitioner;3 (8%)3 (14%)58 (11%)COPD, (2%)(1%)(1%)(1%)(1%)(1%)(1%)(7%)(4%)528 (100%)obstructiveoxygen source. For reasons of privacy, the latter set ofquestions had to be answered anonymously. Finally, 1 yearafter the last interview, the number of eligible patientswho had died was extracted from the file of the oxygencompany. The study was approved by the Medical EthicsCommittee of the University Hospital Utrecht.STATISTICALANALYSISData analysis and descriptive statistics were performedusing the SPSS/PC program(SPSS Inc., Chigaco, U.S.A.).Subgroups were compared using t-tests and Mann-WhitneyU-tests for continuous variables, and by x2 tests in contingency tables for categorical variables. Continuousvaluesare reported as mean & standard deviation; all P valuesrelate to two-tailedcomparisonsand were consideredstatistically significant if cO.05.ResultsOf the 895 patients selected, 341 (38%) refused to participate. Twenty-six of the remaining 554 patients could not beinterviewed for reasons of severe illness or early death.Therefore, data are presented for 371 men (70%) and 157women, with a median age of 70 years (range 19,8-91.9),who had been on LTOT for a mean of 3.5 i 3.6 (0.5-33.0)years. The patients’ diagnoses for which LTOT had beenprescribed are listed in Table 1. There were 350 ex-smokers.Of the 108 smokers, 75 (69%) had a lung disease and 15smoked while using oxygen. Eighty-ninepatients (17%)were housebound and 117 (22%) lived alone. In 389 patients(76%), the costs of LTOT were reimbursed by the DutchNationalHealth Service; the remainingpatients wereprivately insured.In 421 patients (SO%), LTOT was prescribed by a chestphysician; in 58 (1 l%), by a general practitioner;and in 49
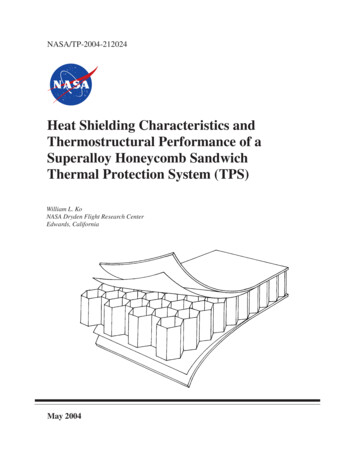
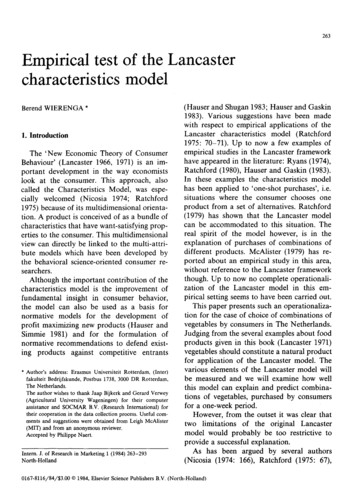
72M. J. KAMPELMACHERTABLE2. Frequencyoxygen sourceET AL.of patients’complaintsOxygen cylinders (n 421)Transport of the cylindersChanging the pressure valveSize and appearance of the cylindersFrequent deliveriesOxygen concentrator (n 76)Vibrations and/or noise (46 dBA)Technical problemsPower failure(s)TransportationproblemsCondensationin the oxygen hoseFragility of the machineLiquid oxygen (n 20)Chance of frostbiteDependency on the stationary canisterNeed for sufficient 10%7%1%35%20%10%5%in nose-Ear complaintsNose13mbleeding9BThroat complaints8mExanthema5m4Other mLOSS duringsleep3nSlashes21 1I0FIG. 1. Complaints(n 528).Restricted(9”/0), by a non-chest physician (internist,cardiologist,neurologistor E.N.T. specialist) (Table 1). Dyspnoea andhypoxaemia were the most important reasons for startingLTOT, in 243 (46%) and 196 patients (37%), respectively.Dyspnoea reduced after LTOT had begun in 34% of 479patients. Only 175 patients (33%) stated that they had beengiven instructions for the use of oxygen, generally by theoxygen company.The oxygen prescription and usage were unknown to 202and 32 patients, respectively. In the remaining patients,oxygen was prescribed for 15.8 5 7.4 h day - i and used for12.7 & 8-O h day - ‘. The mean of the individual differencesbetween the amounts of daily oxygen prescribed and used(n 324). Sixty-fourpatientswas -0.6*3.2hday-’(20%) used oxygen for less hours per day than prescribedbecause of the difficulties they experienced with the treatment, absence of dyspnoea or fear of becoming addicted tooxygen. Compared to the compliantpatients, the noncompliant patients were more frequently males (P O.O06)and were more often ashamed of their therapy (P O.O23).Compliantand non-compliantpatients did not differ significantly with respect to age, diagnosis, duration of LTOT,oxygen source, smoking cessation, and number and type ofcomplaints (other than shame).A total of 430 patients (8 1%) used oxygen cylinders (10 1,20 kg); 71 (13%) used a MC 44 oxygen concentrator(DeVilbiss Healthcare, U.S.A.); 19 (4%) used liquid oxygen;and eight (2%) used a combinationof these. Patients usinga concentratorcomplained more often about their equipment than patients using either cylinders or liquid oxygen(P O.OOl) (Table 2). Of the 316 patients (63%) who hadreceived portable cylinders, 86 (27%) did not use them atall, 54 (16%) used them sporadicallyand only 19 (18%)carried the cylinders themselves.Nasal cannulae were used by 435 patients (82%), a nasalcatheter by 49 (9%), a face mask by 16 (3%), a cuffed nasalcatheter by 15 (3%), a combinationof these by seven(lo%), and a transtrachealmicrocatheterby six ygensowce5III101520% of patientsdue to the oxygen delivery2530device50Feeling ashamedTreatmentduration020III406080100% of patientsFIG. 2. Categories of complaintstherapy (LTOT) (n 528).due to long-termoxygen(1%). A total of 212 patients (40%) had frequently occurring complaints due to their oxygen delivery device (Fig. 1).All complaintscould be divided into five categories(Fig. 2). Most complaints concerned the oxygen equipment,of which the single most important problem was restrictedautonomy.Only 19% of the patients did not have anycomplaints at all (Fig. 3).LTOT monitoringin the outpatientdepartmentwasperformed in 451 patients (85%). In 387 patients (73%), theblood oxygen level was checked regularly by means ofarterial blood gas analysis (73%), capillary blood gas analysis (14%), pulse oximetry (1%) or by a combinationof these(12%). A total of 129 patients (24%) were visited at home,mostly by a general practitioner,a district nurse or aphysiotherapist.To test the representativenessof the patient sample, aselection of their data was compared to data of the 341non-respondents.Except for the daily amounts of oxygenprescribed and used, which were supplied by the oxygencompany together with the data on the non-respondents,informationwas given by the patients themselves. With the
PROFILE AKD012345Number of categoriesFIG 3. Number of categoriesterm oxygen therapy (LTOT)of complaintsdue to long-(n .%%).exception of compliance,all data differed significantly(Table 3). Adding the 26 drop-outs did not influence theresult.DiscussionThis study documentsthat in patients using LTOT,complaints due to this therapy are very common. Mostdiscontent was related to the equipment.As has beendemonstratedby others, patients who use a concentratorare troubled most (13-15). Comparison with other studiesis, however, difficult as studies that have looked into thecomplaints of LTOTpatients are scarce. Moreover, in thefew studies available, patients were rarely directly asked fornegative experiences.In addition, this study shows that in the Netherlands, thetypical LTOTpatient is a 70-year-old male COPD patientwho has had oxygen equipment for 35 years and who hasbeen using oxygen cylinders and nasal cannulae for a meanof 13 h day - i. Althoughthis is, in many respects, inagreement with findings from other countries, there aresome differences which make it difficult to transfer thepresent results to those of other countries (g-12,16-18).Forexample, in Scotland and Sweden, the mean age of patientswas somewhat lower (9,18). This may be due to an earlierstart of LTOT in these countries due to the implementationof clear guidelines. In France and Sweden, oxygen wasprescribed in l&24%of the LTOT patients because ofhypoxaemiadue to sequelae of tuberculosis.In theNetherlands,this is rarely an indication for LTOT (9,19).In France, Poland, Sweden and Switzerland, most patientshave oxygen concentrators, whereas in Italy, most patientsuse liqu
(COPD) and chronic hypoxaemia, long-term oxygen therapy (LTOT) improved survival and reduced clinical deterioration over a 3-year period (1,2). An effect was only demonstrated if oxygen was used for at least 15 h day - ‘, with greater benefit for longer periods. International guide- lines, therefore, recommend the prescription of 15 h day- i as a minimum (3,4). However, if LTOT is prescribed .
![Ticket: # 3011470 - Re: [FCC Complaints] Re: Billing](/img/9/fcc-complaints-from-alabama-residents-2.jpg)