Transcription
Immediate Maxillary Molar ImplantPlacement with Simultaneous CrestalApproach Maxillary Sinus Bone Graft andFlapless ExtractionJone Kim, DDS, MSINTRODUCTIONP.I. Bränemark introduced the idea ofosseointegration when he noticed theincorporation of titanium with bonetissue.1 The concept of osseointegrationrevolutionized the replacement of missingteeth with dental implants. Greaterunderstanding in bone and soft tissuephysiology, accelerated by technologicaladvances, has resulted in significantimprovements in dental implant surgery;enabling a reduction in the number ofsurgeries with less invasive surgicaltechniques, optimized esthetics, anddecrease in the length of total treatmenttime from extraction to final restoration.Contemporary implant surgeons employless traumatic surgical techniques, placeimplants immediately, and combinemultiple surgical techniques with fewersurgeries.The posterior maxillary molar site isparticularly challenging due to reducedalveolar bone and the presence of themaxillary sinus. A ridge preservation bonegraft and/or a maxillary sinus bone graft isoften required prior to implant placement,complicating immediate implantplacement. Simultaneous flaplessextraction, crestal sinus lift, immediateimplant placement and ridge preservationcan be combined into one surgical visit forthe reconstruction of posterior maxillarymolars with appropriate preoperativeevaluation and meticulous surgicaltechnique.EXTRACTIONThere is a theoretical advantage to flaplessextractions in decreasing bone resorption.Canine studies comparing flapped versusflapless extractions of second, third andfourth premolars without bone grafting orimplant placement demonstrate nosignificant difference in horizontal andvertical bone loss. 2-4, 5 However, caninestudies comparing flapped versus flaplessextraction of more anterior first andsecond premolars demonstrates asignificant difference with less boneresorption with the flapless technique. 6 Aplausible explanation for this differencebetween the two studies may be that thestripping of the periosteum in areas ofthinner buccal bone in the more anteriorportion of the maxilla causes greater boneresorption. Studies have shown that thinbuccal bone ( 1 mm) has more boneresorption compared to thicker bone ( 1
mm).7-12 In addition to alveolar boneresorption, full thickness flap may lead tomarginal recession at the adjacent teeth,defective papillae and loss of keratinizedmucosa.13Flapless surgery makes it simpler to bonegraft the socket than flapped surgery. Theflapless extraction socket is basically anempty cavity where bone grafting particlescan be placed with ease and with lessmobility. In addition, since no incisions aremade, a flapless extraction results in lesssurgical trauma, shorter surgical time, noneed of suturing and decreased swellingand pain. Because of these advantages,the flapless extraction technique should beconsidered for all teeth that require anextraction, even if the extraction site is notfor socket management or immediateimplant placement.However, the most important aspect of theextraction, in the author’s view, is notwhether the flap is made or not but ratherminimizing removal of bone. Therefore, theextraction technique should focus onpreserving the alveolar bone, especiallythe buccal and interradicular bone. Amongthe socket bony walls, buccal bone is thethinnest and will, therefore, resorb morethan other bony walls, and thepreservation of interradicular bone iscritical for immediate molar implantplacement after the extraction.7,9,14,15 If theflapless extraction is too difficult, it isbetter to make a minimal flap and removeless bone than to do a flapless extractionwith more bone removal. If the flaplessextraction can be achieved with no boneremoval, then this should give the bestclinical outcome.RIDGE PRESERVATION BONEGRAFT (RPBG)After extraction, the surrounding alveolarbone goes through stages of remodelingresulting in alveolar dimensionalchanges. 16-18 Cardaropoli et al. 17 andAraujo and Lindhe,18 demonstratehorizontal and vertical bone resorption isfrom loss of bundle bone within two weeksafter extraction. The crestal part of thebuccal bone is solely made up of bundlebone, whereas lingual bone is comprised oflamellar and bundle bone. After extraction,since the crestal part of the buccal bone ismade primarily up of bundle bone,increased bone resorption is observed inbuccal bone compared to lingual bone. 17-24Immediate bone grafting is performedafter the extraction to preserve thealveolar ridge, to minimize future bonegrafting, and increase the success of theimplant surgery. There is horizontal bonereduction of 32% at three months, and 2963% at six to 12 months afterextraction.18,19,25-30 There is 11-22%vertical bone resorption observed at sixmonths post-extraction and increasingvertical resorption with multipleextractions.19,22,31,32 Ridge preservationbone grafting (RPBG) is a predictablesurgical modality to preserve the alveolarbone after the extraction and allow forwider and longer implant placement.19,33-37In a recent randomized controlled clinicaltrial, 48 implants were placed into eitherRPBG sites or spontaneously healedextraction sites four months after toothextraction. All implants survived at the oneyear follow up, but during surgery, 14/24(58%) spontaneously healed extractionsites required additional bone grafting,
whereas only 1/24 (7%) needed additionalbone grafting in RPBG sites.38There is an inverse correlation, resulting inthinner buccal bone showing a two-foldincrease in horizontal bone loss comparedto thicker buccal bone in spontaneoushealed sites. Whether there is thick or thinbuccal bone, without bone grafting there isan average of 4.04 mm horizontalreduction.39 There is no correlationbetween the thickness of the buccal boneand alveolar bone loss in RPBG sites. In anRPBG site there is an average of 0.71 mmhorizontal bone reduction. RPBG is able tocompensate for alveolar bone contractionfor both thin and thick buccal bone plates.Therefore, what is important is not thethickness of the buccal plate, but ratherwhether or not RPBG was performed afterthe extraction.RPBG ideally should be performed in aflapless manner to prevent horizontal boneloss and maintain keratinized gingiva. In aprospective randomized clinical trial thatcompared flapped and flapless RPBG,horizontal bone loss was 3.5 0.9 mmand 1.7 0.6 mm for the flapped andflapless approach, respectively.13 Inaddition, the flapless technique showed anincreased width of keratinized gingivacompared to pre-operative measurement,whereas the flapped approach showeddecreased width. However, the flappedgroup had a slightly less vertical buccalbone reduction compared to flapless (-0.6 0.7 vs. -1.1 0.9 mm), which wasstatistically significant.Even though autogenous bone is the goldstandard for bone grafting, many bonegraft alternatives such as xenograft,allograft, alloplast , and bonemorphogenetic protein have been used inRPBG. Currently, there is no consensus onone bone graft material being superior tothe others. 29,33,37,40-47 No matter whichbone grafting material or surgicaltechnique is utilized, the ultimate goal ofRPBG is to preserve the alveolar bone forfuture implant placement reducing theneed for additional bone augmentation atthe time of implant placement. 6,48-50IMMEDIATE IMPLANTPLACEMENTIn the beginning stages of implant surgery,implants were primarily placed in adelayed manner. Extraction sockets healedfor several months prior to implantplacement. Implants placed in a delayedapproach have a high success rate.5155The first clinical study of immediateimplant placement was published in1978.56 Surgical techniques have evolvedalong with increased knowledge of bonehealing in the extraction site to improvethe immediate placement of dentalimplants with predictable results7,26,5765Short term survival rates and clinicaloutcomes are similar in both immediateand delayed approaches.63 Advantages ofimmediate implant placement include thereduction in the number of surgeries andtreatment time, preservation of alveolarheight and width, optimal gingival esthetic,ideal implant placement and patient’sconvenience.47,59,66-72 There is morefavorable bone healing and improvementin soft tissue contour with immediateplacement.26One of the major concerns with immediateimplant placement is the presence ofinfection at the extractionsite.73 Successful outcomes have beendemonstrated with placement of implantsplaced into extraction sites with periapicallesions.5,74-76 A retrospective study of 418
immediate implants placed into extractionsites with periapical lesions demonstrateda 97.8% survival rate with mean follow upof 67 months. 77 Immediate implantsurvival rates are similar for extractionsites with or without perapical lesions.There are several factors that areimportant to ridge alteration and survivalafter immediate implant placement:thickness of buccal wall, horizontal bonegap and initial primary implantstability.7,57,63,78Thicker bone in the buccalwall resulted in less resorption of thebuccal wall, which will decrease the chanceof dehiscence and other implantcomplications.7,9,39,78,79 In the posteriormaxilla there will frequently be a horizontalgap after immediate implant placementdue to the fact that the dimension of thesocket is larger than the diameter of theimplant.For maxillary first molar, the averagemesio-distal and bucco-lingualmeasurement is 10.4 and 11.5 mm,respectively. 80 If the gap is within 2 mm,after implant placement, spontaneoushealing without bone grafting can occur.57,81If the gap is wider than 2 mm, bonegrafting is recommended for immediateimplant placement after extraction in orderto minimize bone resorption.63 Adequateprimary stability is another critical factorfor a successful clinical outcome in animmediate implant placement and loadingof the implant.82, 83 Currently, studiesdemonstrating that primary stability is notcrucial with implants with special types ofsurface treatment have only been done ondelayed implant placement not onimmediate implant placement. 84,85Pre-operative and post-extractionevaluation of the socket and bone isimportant for determining if primarystability of the implant can be attained. Forimmediate molar implant placement afterextraction, besides vital structures such asthe maxillary sinus, adequate dimensionsof the alveolar bone, particularly ofinterradicular bone, are crucial forachieving primary stability of theimplant.15,86 Primary stability of the implantis achieved by placing the implant in theinterradicular bone. Anatomical dimensionsof the interradicular bone will depend upontooth and trunk length and rootmorphology;80 the more divergent theroots are the wider the interradicular bone.Vertical length of the interradicular bonecan be limited by pneumatization ofmaxillary sinus. The location ofinterradicular bone is usually the ideal sitefor implant placement. When there is anabsence or inadequacy of interradicularbone for immediate molar implantplacement, the surgeon may attempt toplace the implant in one of the rootsockets. However, placing the implant atan off-angle will increase the magnitude offorce to the implant and surroundingbone.87 In addition, an implant that isplaced in a compromised position may leadto difficulties with abutment and crownplacement and hygiene. Therefore, goodextraction technique to preserve thesocket wall and interradicular bone is vitalto the successful outcome of immediateimplant placement after an extraction.
MAXILLARY SINUS BONEGRAFTMaxillary sinus bone graft (MSBG) was firstintroduced by Tatum in 1976. 88Subsequently, Boyne and James publishedthe first study of maxillary sinus bonegrafting using autogenous bone grafting in1980. 89 Ever since then, a lateral windowapproach, derived from the Caldwell-Lucprocedure, has been the surgical choice totreat vertically deficient bone in theposterior maxilla. 90-93 Even thoughautogenous bone is the gold standard,different bone grafting materials havebeen used in the lateral approach MSBGwith predictable results. 94-100The obvious indication for MSBG isinadequate vertical alveolar bone in theposterior maxilla for implant placement. Aslong as the bone grafting does not extendto block the ostium, bone grafting in thesinus is not contraindicated and isgenerally a benignprocedure. 101 Contraindications for MSBGcan be categorized into two groups:patient (medical) and sinus (local)factors. 101, 102 Some of the patient ormedical contraindications includechemotherapy or radiotherapy of themaxillary region, immunocompromisedstatus, medical conditions affecting bonemetabolism, pregnancy, uncontrolleddiabetes and alcohol or drug abuse. Sinusor local contraindications includeinadequate transverse dimension of thesinus, intranasal acute or chronic sinusitis,unrepaired oroantral fistula, recent nasalor sinus surgery, cysts or tumors of thesinus, and ostium in the surgical site.In addition to these contraindications,there are factors that may predisposecertain patients to implant failures in themaxillary sinus.101-104 One of the predictorsof implant failure in the posterior maxilla issmoking. Studies have shown thatsmoking is a relative risk to implantfailures. 105, 106 In regards to effects ofsmoking in MSBG, a retrospective study byZinser104 evaluated 1,045 implants placedin the grafted maxillary sinus andconcluded that smoking doubled therelative risk of implant failure.104 Incontrast, a review of implants placed inmaxillary sinus lift sites by Pjetursson, etal.107 did find higher failure rates forsmokers compared to non-smokers (3.5%vs. 1.9 %, respectively), but thisdifference was not statistically significant.Other predictors of implant failure in theposterior maxilla that were mentioned arebone quality, time lapse from extraction toimplant placement, residual alveolar boneheight, augmented compared to nonaugmented sinus and membranethickness.After Tatum88 first introduced lateralapproach MSBG, Summers 108 publishedthe first crestal approach (also known astransalveolar) to the sinus, using a set oftapered osteotomes with increasingdiameter. Since then, MSBG has evolvedover the years from lateral windowopening to various crestal approachtechniques, including using piezoelectricsurgery, trephines, osteotome, hydrauliclift/pressure, press-fit bone block, drillsspecifically designed for crestal approachand modifications of these techniques.109121Studies comparing crestal versus lateralapproaches to MSBG revealed that bothtechniques showed similar success inclinical results.122-124The main advantages to the crestalapproach MSBG is that it can be donewithout a flap, with less post-operative
swelling and pain, minimal bone graftingmaterials and with reduced surgicaltime.107,116,125 The most common crestalapproach MSBG technique is condensingand tapping of the bone with variousdiameter osteotomes to lift the sinusmembrane, which was first described bySummers.108The crestal approach is simpler than thelateral approach MSBG in the immediatelyextracted molar sites. This is due to thefact that the unevenness of the maxillarysinus floor often occurs from molar rootsprotruding into the sinus, which can makea lateral approach MSBG more challenging.In addition, the lateral approach willrequire making a buccal bony windowabove the mesio-buccal and disto-buccalroots (approximately 12 mm in length) andcontinuously elevating the membraneinferiorly to the sinus floor, at which thelowest point is at the trifurcation of theroots.80 These factors can make the lateralapproach sinus lifting more challengingimmediately after the extraction.In the crestal approach MSBG inimmediately extracted molar sites, theopening into the sinus is through theinterradicular bone, which is usually themost inferior part of the sinus floor in themaxillary molar. Elevating the membranefrom inferiorly to superiorly, will result inuniform and “tent” like sinuselevation.102Also, the crestal approachsinus lift is completed after a sufficientelevation and, thereby, reducing theoverall sinus lifting. Whereas in the lateralapproach, a much larger area of the sinushas to be elevated due to the inability toform “tent” like membrane elevation.In addition, it is the author’s opinion thatbetter stability of the implant can beachieved with a crestal approach due to“tent” like lifting of the maxillary sinusmembrane. This “tenting” effect of themaxillary sinus membrane, via crestalapproach, allows firmer condensing of thebone grafting particles within the elevatedmembrane space than the lateralapproach, which usually has a much largermembrane elevated space that can allowmore movement of the bone graftingparticles.In 2000, Cosci and Luccioli, 129 published astudy introducing a new sinus lifttechnique with the use of lifting drills toperforate, not fracture, the sinus floor andlift the membrane. This technique isreferred to as the Cosci’s technique. Thetip is specially designed so that it will notperforate the sinus membrane even if thedrill tip makes contact with the membrane.There is no use of osteotomes. In this sixyear retrospective study, 265 implantswere placed in a one stage crestalapproach MSBG, in healed sites, with eightimplant losses, resulting in a 97% survivalrate. One study even compared Cosci’stechnique to Summers’ technique.116 Thisstudy showed that both techniquesdisplayed predictable results but Cosci’stechnique required less surgical time, lessintra- and postoperative morbidity and waspreferred by patients. In another study,134 implants placed in a multicenterretrospective study using Cosci’stechnique, showed implant survival rate of96.3% with average follow-up time of 48.2months.130In this study, the average preoperative alveolar bone height was 3.46mm 0.91 mm, which further shows thatimplants can be successfully placed withsimultaneous crestal approach MSBG inalveolar bone height of less than 5 mm.
INDICATIONS AND RATIONALEFOR IMMEDIATE MAXILLARYMOLAR IMPLANT PLACEMENTWITH SIMULTANEOUSCRESTAL APPROACHMAXILLARY SINUS BONEGRAFT AND FLAPLESSEXTRACTIONReduced vertical alveolar ridge due toinherent bone remodeling is one of thechallenges of an implant placement afterthe extraction of maxillary posteriorteeth.17,18 In addition to anatomiclimitations, maxillary sinuspneumatization, which ends normally atage 20, will continue to progress after theextraction with loss of vertical alveolarbone.94,131,132Clinicians should considerpreserving the alveolar bone height byimmediate implant placement and/orimmediate bone grafting to decrease thesinus pneumatization and alveolar boneloss.133 In addition, time lapse from theextraction to implant placement is one ofthe predictors of implant failure inposterior maxilla.103Immediately after the extraction the besttreatment for posterior maxillary teethmay be an implant placement withsimultaneous MSBG, if indicated. In aretrospective analysis, 391 implants wereplaced immediately after the extraction ofmaxillary molar teeth and 156 out of 391implants required simultaneous MSBG dueto inadequate alveolar boneheight.86 Overall survival rate was 99.5%(389/391) after 75 month follow-up,showing that immediate maxillary molarimplant placement at the time ofextraction with simultaneous crestalapproach has a high survival rate.One of the drawbacks for crestal approach,as with the lateral approach, is achievingadequate primary stability of the implantat the time of MSBG. Most studies indicatethat less residual alveolar bone results inincreased implant failure rate. 101,126,127Therefore, studies have shown that idealresidual alveolar height, for immediateimplant placement with simultaneouscrestal approach MSBG, should be 5-6 mmto achieve primary stability of theimplant.107,125 However, Gonzalez, etal.,128 compared the success rate ofimmediate implant placement withsimultaneous crestal approach MSBG, inhealed extraction sites, with residualalveolar bone height of 4 mm and 4mm, which showed 100% and 98.51%success rates, respectively. Simultaneouscrestal approach MSBG and implantplacement can be achieved in verticalalveolar bone of less than 5 mm with ahigh success rate.The requirements for maxillary molarimplant placement, immediately after theflapless extraction, with simultaneouscrestal approach MSBG are: 1) adequatehorizontal dimension for diameter ofplanned implant; 2) no major soft tissuedefect, such as buccal or lingual fistula; 3)no oroantral communication (OAC) greaterthan 3-5 mm after the extraction; 4) nopurulent discharge from socket and/ormaxillary sinus after the extraction; 5) nomajor periapical and maxillary sinusinfection and/or pathology; 6) no morethan one alveolar wall defect; and 7) nosymptomatic maxillary sinusitis. If any ofthe mentioned criteria are not met, theimplant should be placed in a delayapproach. Comprehensive pre-operative
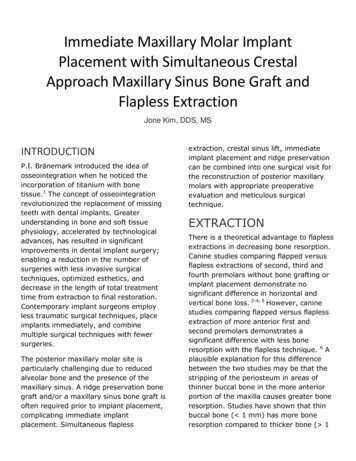
clinical and radiographic evaluations toselect an ideal surgical candidate for thistechnique are paramount to a successfulclinical outcome.Pre-operative radiographic evaluation formaxillary molar extraction should includethe following: 1) horizontal and verticaldimensions of interradicular bone; 2)evaluation of maxillary sinus, such asinfection, thickness of membrane andpathology; 3) presence of periapicalradiolucency, such as bone loss, infectionand lesion; 4) presence of OAC; and 5)evaluation of alveolar wall, such as walldefect, thickness of buccal bone andvertical and horizontal dimensions of thesocket wall. It is possible to perform thesurgery with a panoramic radiograph but acone beam CT (CBCT) is highlyrecommended for pre-operativeradiographic evaluation.(Figure 1A, B) Clinical evaluation formaxillary molar should include thefollowing: 1) status of adjacent teeth; 2)soft tissue evaluation (such as keratinizedtissue, gingival recession, swelling andfistula); 3) inter-occlusal and mesio-distalspace; 4) clinical signs of parafunctionalhabits; and 5) occlusion.Figure 1A. Cone beam CT of maxillary molar tooth.A. Maxillary molar tooth with divergent roots with adequateinterradicular bone for an immediate implant placement.Sinus is within-normal-limit (WNL).Figure 1B. Maxillary molar tooth with inadequateinterradicular bone for an immediate implant placement dueto convergent roots. Notice the roots are protruding into thesinus. Sinus is WNL.This technique is a preferred implanttreatment plan for many, if not all, of thepatients that desire an implant after theextraction when they are given delayed vs.immediate surgical options.If the extraction, RPBG, MSBG, andimplant placement are done in 2 or moresurgeries, the patient may select a nonimplant treatment option, due to increasedtreatment time, cost, and number ofsurgeries, even though an implant may bethe best treatment option and the patient’spreferred plan. The added benefit for thesurgeon is less operative procedures withless office visits.
SURGICAL TECHNIQUE FORIMMEDIATE MAXILLARYMOLAR IMPLANT PLACEMENTWITH SIMULTANEOUSMAXILLARY SINUS BONEGRAFT AND FLAPLESSEXTRACTIONtissue is then gently pushed away from thetooth. Freeing up the crestal gingival tissueslightly allows for reduced trauma to thesoft tissue from any instruments that willbe in close contact during the extraction. Aperiosteal elevator can also be used to freeup the crestal gingival tissue. No incision ismade and interdental papilla is notdetached from the bone during theextraction.Pre-operative RegimenNext, a periotome (Dowell, RanchoCucamonga, Calif.) is used to separatebuccal bone from mesiobuccal tomesiodistal and palatal bone from thetrunk and root of the tooth. Use of aperiotome will reduce the incidence ofalveolar bone fracture and, moreimportantly, can be used to preserve thebuccal bone in the socket, instead ofhaving the buccal bone attached to theroot during the extraction. Then a straightelevator or slightly curved elevator isplaced into the sulcus to gently subluxatethe tooth. After adequate subluxation, ifthere is enough tooth structure, anattempt is made to extract the tooth byusing a modified upper forcep (KarlSchumacher, Linden N.J.). Using amodified forcep that has smaller andnarrower beaks will reduce trauma to thealveolar bone and soft tissue, compared toa conventional upper forcep.The patient is given the following preoperative antibiotic regimen: 1) If thepatient has no allergic reaction topenicillin, the patient takes 2 grams ofamoxicillin 1 hour prior to surgery andthen 1 gram bid for 5 days; 2) If allergic topenicillin, the patient takes 600 mgclindamycin 1 hour prior to surgery andthen 150 mg qid for 5 days. Just prior tosurgery, the patient’s mouth is rinsed withchlorohexidine gluconate for approximately15-20 seconds.Flapless ExtractionAs mentioned previously, the mostimportant aspect of the extraction is notwhether the flap is made, but rather that itis focused on minimizing the removal ofbone. Therefore, the extraction techniqueshould concentrate on preserving thealveolar bone, especially the buccal andinterradicular bone.After local anesthetic is administered, thefirst step is to gently free up the crestalgingival tissue away from the toothwithout stripping off any of the periosteumfrom the alveolar bone. To do this, a 2/4molt curette (Hu-Friedy, Chicago, Ill.) isplaced into the gingival sulcus, includingthe interdental gingival tissue. The softDuring the extraction, with a forceps oreven with an elevator during subluxation,the crown of the tooth can fracture,leaving part of the crown, trunk or roots inthe socket. If part of the crown or trunk isin the socket, it is sectioned to separatethe multi-rooted maxillary molar tooth intomultiple single roots.134The goal is tosection the multi-rooted maxillary molartooth and remove the roots individually.However, during sectioning, be cognizant
to avoid removal of the buccal andinterradicular bone, which is located justbelow the root trunk. Trunk length isapproximately 4 mm.15Since maxillary molar teeth have 3 roots,section the remaining crown or trunk into3 parts: mesiobuccal, distobuccal andpalatal root.(Figure 2) To accomplish this, a ½ or #2round bur (SS White, Lakewood, N.J.) isused with a surgical handpiece. Duringtrisecting of the roots, it is not necessaryto touch the bone with the round bur.Preserving the interradicular bone is crucialfor an immediate implant placementbecause this may be the only source ofbone for the primary stability of theimplant.Figure 2. Multi-rooted maxillary molar tooth is sectionedinto 3 separate roots, mesio-buccal (MB), disto-buccal (DB)and palatal (P) roots.After trisecting the roots, a small elevatoror 2/4 molt curette can be used tocomplete the separation of the roots andthen, using the same instrument,subluxate and extract the roots. A thinperiotome or root tip pick can also be usedto loosen and remove the roots. If theroots are firmly embedded in the socketand difficult to extract, a ½ round bur canbe used to section the roots, mesio-distallyor bucco-lingually, and then remove thesectioned roots using appropriateinstruments. All 3 roots can be removed inthis manner.After extraction of the three roots, thesocket needs to be carefully examined forany potential complications. The followingshould be evaluated: sinus floor andmembrane, socket wall, interradicularbone and presence of infection. If the sinusfloor is difficult to visualize, the Valsalvamaneuver can be gently performed tocheck for oroantral communication. After athorough examination, the socket is gentlycuretted to remove any granulation tissueand periapical lesion. However, this stepshould be done with caution if the sinusmembrane is exposed or perforated.After careful curetting, thoroughly reevaluate the socket. Depending on theclinical findings, the surgeon will decide atthis time whether or not to continue withthe next step, modify the treatment planor abort the surgery. Whether to continue,modify, or abort the surgery will dependupon several factors: 1) sinus membraneperforation and size of perforation; 2)vertical and horizontal dimensions ofinterradicular bone; 3) size and location ofbony wall defect; and 4) presence andextent of periapical and sinus infection.Based on these factors and clinicalfindings, the final decision will depend onwhether the alveolar ridge can bepreserved, the implant can attain primarystability, and a sinus bone lift can bepredictably performed. If the decision ismade to continue with the surgery, thenext step is the crestal approach MSBG.
Crestal Approach to the MSBGFrom the pre-operative CBCT and socketevaluation, approximate vertical andhorizontal dimensions of the interradicularbone are estimated. Ideal bucco-lingualand mesio-distal position of the implant isusually the mid-crest of the interradicularbone. The author’s crestal approachmaxillary sinus bone grafting technique issimilar to the technique that was describedby Cosci and Luccioli,129 where “lifting”drills are used to perforate the sinus floorwithout perforating the sinus membrane.The first drill used in the crestal approachMSBG is a 1.3 mm pilot drill (Salvin,Charlotte, N.C.) at 800 RPM, with copiousnormal saline or sterile water irrigation.The depth of the drilling is approximately1-2 mm short of the estimated verticaldimension of the interradicular bone.During drilling with a pilot drill, the suddenfeel of denser bone may indicate that thedrilling depth is at or close to the sinusfloor, which is composed of cortical bone.Cortical bone will feel denser compared tomedullary bone and the surgeon’s tactilesensations should be able to differentiatebetween cortical and medullary boneduring drilling. The next drill used is a 2.0mm twist drill, again 1-2 mm shy ofestimated vertical length of theinterradicular bone. After each drillingsequence, measure the depth of the drillsite with a depth gauge or probe. It isimportant not to drill through the sinusfloor with the twist drill, as this willincrease the likelihood of sinus membraneperforation. After using the 2.0
of 67 months. 77 Immediate implant survival rates are similar for extraction sites with or without perapical lesions. There are several factors that are important to ridge alteration and survival after immediate implant placement: thickness of buccal wall, horizontal bone gap and initial primary implant stability.7,57,63,78Thicker bone in the .