Transcription
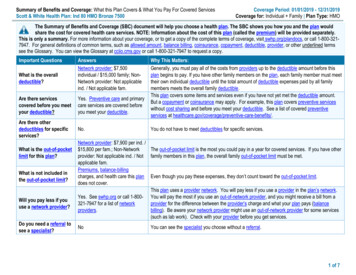
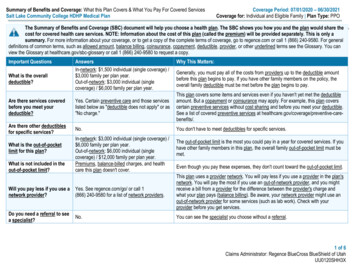
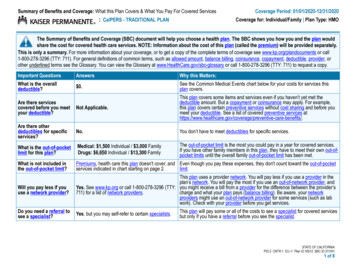
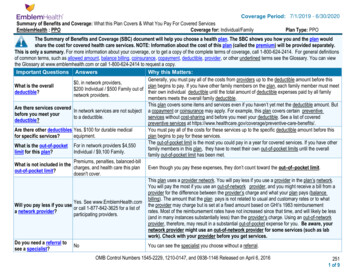
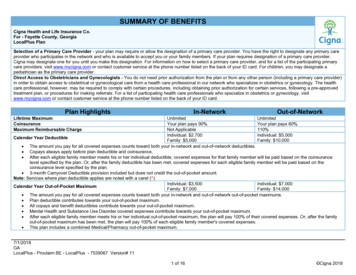
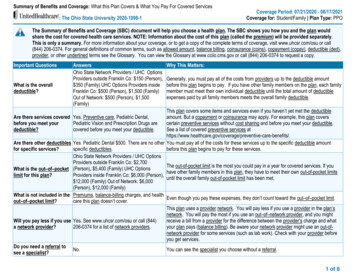
Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services: The Ohio State University 2020-1098-1Coverage Period: 07/21/2020 - 08/17/2021Coverage for: Student/Family Plan Type: PPOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan wouldshare the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately.This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, visit www.uhcsr.com/osu or call(844) 206-0374. For general definitions of common terms, such as allowed amount, balance billing, coinsurance (coins), copayment (copay), deductible (ded),provider, or other underlined terms see the Glossary. You can view the Glossary at www.cciio.cms.gov or call (844) 206-0374 to request a copy.Important QuestionsWhat is the overalldeductible?Are there services coveredbefore you meet yourdeductible?Are there other deductiblesfor specific services?What is the out–of–pocketlimit for this plan?What is not included in theout–of–pocket limit?Will you pay less if you usea network provider?Do you need a referral tosee a specialist?AnswersOhio State Network Providers / UHC OptionsProviders outside Franklin Co: 150 (Person), 350 (Family) UHC Options Providers insideFranklin Co: 500 (Person), 1,500 (Family)Out of Network: 500 (Person), 1,500(Family)Why This Matters:Generally, you must pay all of the costs from providers up to the deductible amountbefore this plan begins to pay. If you have other family members on the plan, each familymember must meet their own individual deductible until the total amount of deductibleexpenses paid by all family members meets the overall family deductible.This plan covers some items and services even if you haven’t yet met the deductibleYes. Preventive care, Pediatric Dental,amount. But a copayment or coinsurance may apply. For example, this plan coversPediatric Vision and Prescription Drugs arecertain preventive services without cost sharing and before you meet your deductible.covered before you meet your deductible.See a list of covered preventive services are-benefits/.Yes. Pediatric Dental 500. There are no other You must pay all of the costs for these services up to the specific deductible amountspecific deductibles.before this plan begins to pay for these services.Ohio State Network Providers / UHC OptionsProviders outside Franklin Co: 2,700The out-of-pocket limit is the most you could pay in a year for covered services. If you(Person), 5,400 (Family) UHC Optionshave other family members in this plan, they have to meet their own out-of-pocket limitsProviders inside Franklin Co: 6,000 (Person),until the overall family out-of-pocket limit has been met. 12,000 (Family) Out of Network: 6,000(Person), 12,000 (Family)Premiums, balance-billing charges, and healthEven though you pay these expenses, they don’t count toward the out–of–pocket limit.care this plan doesn’t cover.This plan uses a provider network. You will pay less if you use a provider in the plan’snetwork. You will pay the most if you use an out–of–network provider, and you mightYes. See www.uhcsr.com/osu or call (844)receive a bill from a provider for the difference between the provider’s charge and what206-0374 for a list of network providers.your plan pays (balance billing). Be aware your network provider might use an out-ofnetwork provider for some services (such as lab work). Check with your provider beforeyou get services.No.You can see the specialist you choose without a referral.1 of 8
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.What You Will PayCommon Medical EventServices You May NeedPrimary care visit to treat an injury or illnessIf you visit a health careprovider’s office orclinicSpecialist visitPreventive care/screening/immunizationDiagnostic test (x-ray, blood work)Imaging (CT/PET scans, MRIs)HealthSmart RXIf you have a testIf you need drugs totreat your illness orconditionGeneric drugsMore information about Preferred brand drugsprescription drugcoverage is available atwww.uhcsr.com/pdlNon-preferred brand drugsLimitations, Exceptions, & OtherPreferredOut-of-NetworkImportant InformationProvider (You In-Network Provider (Youwill pay theProviderwill pay theleast)most) 20 Copay pervisit; ded does 40% Coins40% Coinsnot applyMay not apply when related to surgery orPhysiotherapy. 20 Copay pervisit; ded does 40% Coins40% Coinsnot applyIncludes preventive services specified inthe health care reform law or benefitsprovided as mandated by state law.No ChargeNo Charge40% CoinsYou may have to pay for services thataren’t preventive. Ask your provider if theservices needed are preventive. Thencheck what your plan will pay for.10% Coins40% Coins40% �––––––––10% Coins40% Coins40% �––––––––10% Coinsded does notapply10% Coins10% Coinsded does not ded does notapplyapply20% Coinsded does notapply20% Coins50% Coinsded does not ded does notapplyapply50% Coinsded does notapply50% Coins50% Coinsded does not ded does notapplyapplyMinimum cost to the insured is 10 or thecost of the drug, whichever is less.Limited up to a 31 day supply perprescription.Minimum cost to the insured is 10 or thecost of the drug, whichever is less.Limited up to a 31 day supply perprescription.Minimum cost to the insured is 10 or thecost of the drug, whichever is less.*For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu2 of 8
What You Will PayCommon Medical EventServices You May NeedSpecialty drugsIf you have outpatientsurgeryFacility fee (e.g., ambulatory surgery center)Physician/surgeon feesEmergency room careIf you need immediatemedical attentionEmergency medical transportationUrgent careIf you have a hospitalstayIf you need mentalhealth, behavioralhealth, or substanceabuse servicesFacility fee (e.g., hospital room)Physician/surgeon feesOutpatient servicesInpatient servicesPreferredOut-of-NetworkProvider (You In-Network Provider (Youwill pay theProviderwill pay theleast)most)Limitations, Exceptions, & OtherImportant InformationLimited up to a 31 day supply perprescription.Same asSame asSame as above; Minimum cost to the insured is 40above; dedabove; dedded does notgeneric drug, 80 brand name drug, ordoes not apply does not apply apply 120 non-preferred brand drug, or thecost of the drug, whichever is less.Limited up to a 31 day supply perprescription10% Coins40% Coins40% �––––––––10% Coins40% Coins40% �––––––––10% Coins10% Coins10% CoinsMay be limited to use of emergency room 100 Copay 100 Copay 100 Copay per and supplies.per visit; ded per visit; ded visit; ded does The Copay will be waived if admitted todoes not apply does not apply not applythe Hospital.10% Coins10% Coins10% �–––––––– 25 Copay pervisit; ded does 40% Coins40% CoinsMay be limited to facility fees.not apply10% Coins40% Coins40% �––––––––10% Coins40% Coins40% �––––––––Based onBased onBased on settingsetting where setting where where service �–––––––service isservice isperformedperformedperformedBased onBased onBased on settingsetting where setting where where service �–––––––service isservice isperformedperformedperformed*For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu3 of 8
What You Will PayCommon Medical EventServices You May NeedOffice visitsIf you are pregnantChildbirth/delivery professional servicesChildbirth/delivery facility servicesIf you need helprecovering or haveother special healthneedsPreferredProvider (Youwill pay theleast)Based onsetting whereservice isperformedBased onsetting whereservice isperformedBased onsetting whereservice isperformedHome health care10% CoinsRehabilitation services10% CoinsHabilitation services10% CoinsSkilled nursing careDurable medical equipmentHospice servicesLimitations, Exceptions, & OtherOut-of-NetworkImportant InformationIn-Network Provider (YouProviderwill pay themost)Based onBased on setting Cost sharing does not apply for preventivesetting where where service is services when provided by a Preferredservice isperformedProvider or In-Network Provider.performedDepending on the type of services, aBased onBased on setting copayment, coinsurance, or deductiblesetting where where service is may apply. Maternity care may includetests and services described elsewhere inservice isperformedthe SBC (i.e. ultrasound).performedBased onBased on settingsetting where where service �–––––––service isperformedperformed100 visits maximum per Policy Year /40% Coins40% CoinsAdditional 250 visit maximum per PolicyYear for Private Duty Nursing40% Coins40% CoinsLimits per Policy Year as follows: 20 visits of physical therapy 20 visits of occupational therapy 20 visits of speech therapy 12 visits of manipulative therapy40% Coins40% CoinsSeparate physical, occupational andspeech therapy limits apply toRehabilitative and Habilitative �––––––10% Coins40% Coins40% Coins10% Coins40% Coins40% Coins10% Coins40% Coins40% CoinsSee your50% Coins; 50% Coins; dedIf your child needsplan’s Pediatric ded does not does not apply See your plan’s Pediatric Vision BenefitChildren’s eye examdental or eye careVision Benefit applyDetails. Age limits apply.*Details*For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu4 of 8
What You Will PayCommon Medical EventServices You May NeedChildren’s glassesChildren’s dental check-upPreferredProvider (You In-Networkwill pay theProviderleast)See your50% Coins;plan’s Pediatric ded does notVision Benefit applyDetailsSee your50% Coinsplan’s PediatricDental BenefitDetailsLimitations, Exceptions, & OtherOut-of-NetworkImportant InformationProvider (Youwill pay themost)50% Coins; ded See your plan’s Pediatric Vision Benefitdoes not apply Details. Age limits apply.*50% CoinsSee your plan’s Pediatric Dental BenefitDetails. Age limits apply.**For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu5 of 8
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Bariatric surgery Cosmetic surgery not specifically provided in the Dental care (Adult),not specifically provided for in Hearing aids Infertility treatment Long-term care Routine foot care Weight loss programspolicy.the policy.Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Chiropractic care Private-duty nursing Routine eye care (Adult) Non-emergency care when traveling outside theU.S.Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for thoseagencies is: Ohio Department of Insurance at 1-800-686-1526 or visit http://www.insurance.ohio.gov/Pages/default.aspx. Other coverage options may be available toyou too, including buying individual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visitwww.HealthCare.gov or call 1-800-318-2596.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents alsoprovide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance,contact: Ohio Department of Insurance at 1-800-686-1526 or visit oes this plan provide Minimum Essential Coverage? YesIf you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from therequirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? YesIf your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.*For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu6 of 8
Language Access Services:Spanish (Español): Para obtener asistencia en Español, llame al 1-866-260-2723.Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-866-260-2723.Chinese (中文): � 1-866-260-2723.Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-866-260-2723.––––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next section.––––––––––*For more information about limitations and exceptions, see plan or policy document at www.uhcsr.com/osu7 of 8
About these Coverage Examples:This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different dependingon the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharing amounts (deductibles, copayments andcoinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different health plans. Pleasenote these coverage examples are based on self-only coverage.Peg is Having a Baby(9 months of in-network pre-natal care and ahospital delivery) The plan’s overall deductible Specialist copayment Hospital (facility) coinsurance Other coinsurance 150 2010%10%Managing Joe’s type 2 Diabetes(a year of routine in-network care of a wellcontrolled condition) The plan’s overall deductible Specialist copayment Hospital (facility) coinsurance Other coinsurance 150 2010%10%Mia’s Simple Fracture(in-network emergency room visit and follow upcare) The 500plan’s overall deductible Specialist40% copayment Hospital40% (facility) coinsurance Other40%coinsurance 150 2010%10%This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility ServicesDiagnostic tests (ultrasounds and blood work)Specialist visit (anesthesia)This EXAMPLE event includes services like:Primary care physician office visits (includingdisease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services(physical therapy)Total Example CostTotal Example CostTotal Example Cost 12,800In this example, Peg would pay:Cost Sharing 7,400In this example, Joe would pay:Cost Sharing 1,900In this example, Mia would pay:Cost SharingDeductibles 150Deductibles 150Deductibles 150Copayments 40Copayments 200Copayments 140Coinsurance 1,300Coinsurance 200Coinsurance 100What isn’t coveredLimits or exclusionsWhat isn’t covered 60The total Peg would pay is 1,550Limits or exclusionsThe total Joe would pay isWhat isn’t covered 60 610Limits or exclusionsThe total Mia would pay isThe plan would be responsible for the other costs of these EXAMPLE covered services. 0 3908 of 8
NON-DISCRIMINATION NOTICEUnitedHealthcare StudentResources does not treat members differently because of sex, age,race, color, disability or national origin.If you think you were treated unfairly because of your sex, age, race, color, disability or nationalorigin, you can send a complaint to:Civil Rights CoordinatorUnited HealthCare Civil Rights GrievanceP.O. Box 30608Salt Lake City, UTAH 84130UHC Civil Rights@uhc.comYou must send the written complaint within 60 days of when you found out about it. A decisionwill be sent to you within 30 days. If you disagree with the decision, you have 15 days to ask usto look at it again.If you need help with your complaint, please call the toll-free member phone number listed onyour health plan ID card, Monday through Friday, 8 a.m. to 8 p.m. ET.You can also file a complaint with the U.S. Dept. of Health and Human Services.Online laint forms are available one: Toll-free 1-800-368-1019, 800-537-7697 (TDD)Mail: U.S. Dept. of Health and Human Services. 200Independence Avenue, SWRoom 509F, HHH Building Washington, D.C. 20201We also provide free services to help you communicate with us. Such as, letters in otherlanguages or large print. Or, you can ask for free language services such as speaking with aninterpreter. To ask for help, please call the toll-free member phone number listed on your healthplan ID card, Monday through Friday, 8 a.m. to 8 p.m. ET.NDLAP-FO-001 (1-17)
Bariatric surgery Cosmetic surgery not specifically provided in the policy. Dental care (Adult),not specifically provided for in the policy. Hearing aids Infertility treatment Long-term care Routine foot care Weight loss programs Other Covered Services