Transcription
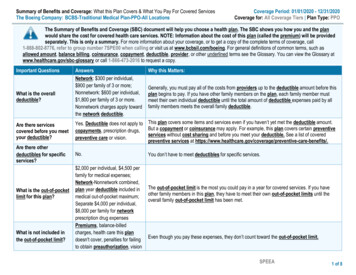
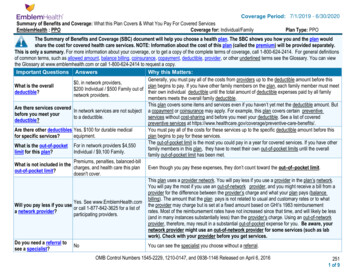
Coverage Period: 7/1/2019 - 6/30/2020Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered ServicesCoverage for: Individual/FamilyEmblemHealth : PPOPlan Type: PPOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan wouldshare the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately.This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 1-800-624-2414. For general definitionsof common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can viewthe Glossary at www.emblemhealth.com or call 1-800-624-2414 to request a copy.Important Questions AnswersWhy this Matters:Generally, you must pay all of the costs from providers up to the deductible amount before this 0, in network providers,plan begins to pay. If you have other family members on the plan, each family member must meetWhat is the overall 200 Individual / 500 Family out oftheir own individual deductible until the total amount of deductible expenses paid by all familydeductible?network providers.members meets the overall family deductible.This plan covers some items and services even if you haven’t yet met the deductible amount. ButAre there services coveredIn network services are not subject a copayment or coinsurance may apply. For example, this plan covers certain preventivebefore you meet yourto a deductible.services without cost-sharing and before you meet your deductible. See a list of covereddeductible?preventive services at e-benefits/.You must pay all of the costs for these services up to the specific deductible amount before thisAre there other deductibles Yes, 100 for durable medicalequipment.plan begins to pay for these services.for specific services?The out-of-pocket limit is the most you could pay in a year for covered services. If you have otherWhat is the out-of-pocket For in network providers 4,550family members in this plan, they have to meet their own out-of-pocket limits until the overallIndividual / 9,100 Family.limit for this plan?family out-of-pocket limit has been met.Premiums, penalties, balanced-billWhat is not included in thecharges, and health care this plan Even though you pay these expenses, they don’t count toward the out–of–pocket limit.out-of-pocket limit?doesn't cover.This plan uses a provider network. You will pay less if you use a provider in the plan’s network.You will pay the most if you use an out-of-network provider, and you might receive a bill from aprovider for the difference between the provider’s charge and what your plan pays (balancebilling). The amount that the plan pays is not related to usual and customary rates or to whatYes. See www.EmblemHealth.comthe provider may charge but is set at a fixed amount based on GHI’s 1983 reimbursementWill you pay less if you useor call 1-877-842-3625 for a list ofrates. Most of the reimbursement rates have not increased since that time, and will likely be lessa network provider?participating providers.(and in many instances substantially less) than the provider’s charge. Using an out-of-networkprovider, therefore, may result in a substantial out-of-pocket expense for you. Be aware, yournetwork provider might use an out-of-network provider for some services (such as labwork). Check with your provider before you get services.Do you need a referral toNoYou can see the specialist you choose without a referral.see a specialist?OMB Control Numbers 1545-2229, 1210-0147, and 0938-1146 Released on April 6, 20162511 of 9
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.CommonMedical EventIf you visit a healthcare provider’s officeor clinicIf you have a testWhat You Will PayServices You May NeedNetwork ProviderOut-of-Network Provider(You will pay the least)(You will pay the most)Primary care visit to treat Preferred: 0 co-pay per visit0% coinsurancean injury or illnessParticipating: 15 co-pay per visitPreferred: 0 co-pay per visit0% coinsuranceSpecialist visitParticipating: 30 co-pay per visitPreventivecare/screening/No charge0% coinsuranceimmunizationDiagnostic test (x-ray, 20 co-pay per visit0% coinsuranceblood work)Imaging (CT/PET scans, 50 co-pay per visit0% coinsuranceMRIs)Generic drugs (Tier 1)Not coveredNot coveredPreferred brand drugsNot coveredNot covered(Tier 2)Non-preferred brandNot coveredNot covereddrugs (Tier 3)If you need drugs totreat your illness orconditionMore information aboutprescription drugcoverage is available atwww.EmblemHealth.com. Specialty drugsFacility fee (e.g.,If you have outpatient ambulatory surgerycenter)surgeryPhysician/surgeon feesEmergency room careIf you need immediate Emergency medicaltransportationmedical attentionUrgent careFacility fee (e.g., hospitalIf you have a hospital room)stayPhysician/surgeon fee*Limitations, Exceptions, & OtherImportant Information-----None----Lower co-pay applies when a PreferredProvider refers-----None---------None----Pre-certification required-----None----------None-----Not coveredNot coveredNot coveredNot coveredPlease check with your employer.CoveredNot covered0% coinsuranceNot covered-----None---------None-----Not covered20% coinsuranceNo air ambulance or ambulette service 50 co-pay per visit0% coinsurance-----None-----Not coveredNot coveredPlease check with your employer.Covered0% coinsurance-----None-----* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.2512 of 9
CommonMedical EventServices You May NeedOutpatient servicesIf you need mentalhealth, behavioralhealth, or substanceabuse servicesInpatient servicesOffice visitsChildbirth/deliveryprofessional servicesWhat You Will PayOut-of-Network ProviderNetwork Provider(You will pay the least)(You will pay the most)Preferred: 0 co-pay per visit0% coinsuranceNo prior approval requiredParticipating: 15 co-pay per visit 500 co-pay peradmission/ 1,250 maximum 300 co-pay per admission/ 750Pre-certification requiredper calendar year. 20% tomaximum per calendar yearmax of 2,000 per person percalendar year.No charge0% coinsurance-----None----No charge0% coinsuranceIf you are pregnantChildbirth/delivery facilityNo chargeservices0% coinsuranceHome health care 50 deductible per episode;20% coinsurance insuranceRehabilitation servicesIf you need helprecovering or haveother special healthneedsHabilitation servicesSkilled nursing careDurable medicalequipmentIf your child needsdental or eye careHospice servicesChildren’s eye examChildren’s glassesChildren’s dental checkup*Limitations, Exceptions, & OtherImportant InformationNo chargePreferred: 0 co-pay per visit0% coinsuranceParticipating: 30 co-pay per visitPreferred: 0 co-pay per visit0% coinsuranceParticipating: 30 co-pay per visitNot coveredNot covered-----None----Enhanced schedule increases thereimbursement of the basic program's nonparticipating provider fee schedule, onaverage, by 75%. Pre-certification requiredcontact NYC Healthline at 1-800-521-9574.200 visits per member per plan year.Preauthorization required.Coverage limited to 16 visits per calendaryear. Pre-certification required for additionalvisitsNot coveredNot coveredNot covered-----None----Pre-certification required on greater than 100 deductible; 50% of usual 2,000 call NYC Healthline at 1-800-521and customary charge9574.Not covered-----None----Not covered-----None----Not covered-----None-----Not coveredNot covered 100 deductible-----None-----* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.2513 of 9
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Hearing aids Acupuncture Routine foot care Long-term care Cosmetic surgery Weight loss programs Most coverage provided outside the United States Dental care Non-emergency care when traveling outside the U.S.Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Bariatric surgery (Prior Approval required) Private-duty nursing Infertility treatment (Prior Approval required) Chiropractic care Routine eye careYour Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for thoseagencies is: New York State Department of Financial Services at 1-800-342-3736 or www.dfs.ny.gov/, U.S. Department of Health and Human Services at 1-877-2672323 x1565 or www.cciio.cms.gov, U.S. Department of Labor, Employee Benefits Security Administration at 1-866-444-3272 html or www.dol.gov/ebsa/healthreform. Other coverage options may be available to you too, including buyingindividual insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call1-800-318-2596.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your right, look at the explanation of benefits you will receive for that medical claim. Your plan documents alsoprovide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance,contact:EmblemHealthBy Phone:Please call the number on your ID card.In writing:EmblemHealthGrievance and Appeals DepartmentP.O. Box 2801New York, NY 10116-2807Website: www.emblemhealth.comFor All Coverage TypesNew York State Department of Financial ServicesBy Phone: 1-800-342-3736In writing:New York State Department of Financial ServicesConsumer Assistance UnitOne Commerce PlazaAlbany, NY 12257Website: www.dfs.ny.gov* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.2514 of 9
For HMO CoverageNew York State Department of HealthBy Phone: 1-800-206-8125In writing:New York State Department of HealthOffice of Health Insurance ProgramsBureau of Consumer Services – Complaint UnitCorning Tower – OCP Room 1607Albany, NY 12237Email: managedcarecomplaint@health.ny.govWebsite: www.health.ny.govConsumer Assistance ProgramNew York State Consumer Assistance ProgramBy Phone: 1-888-614-5400In writing:Community Health Advocates633 Third Avenue, 10th FloorNew York, NY 10017Email: cha@cssny.orgWebsite: www.communityhealthadvocates.orgFor Group Coverage:U.S. Department of LaborEmployee Benefits Security Administration at 1-866-444-EBSA (3272)Website: www.dol.gov/ebsa/healthreformDoes this plan provide Minimum Essential Coverage? YesIf you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from therequirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? YesIf your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.Language Access Services:Spanish (Español): Para obtener asistencia en Español, llame al 1-800-624-2414Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-800-624-2414Chinese (中文): � 1-800-624-2414Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' ––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next ––––––––* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.2515 of 9
This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will bedifferent depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharingamounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion ofcosts you might pay under different health plans. Please note these coverage examples are based on self-only coverage.Peg is having a babyManaging Joe’s type 2 diabetesMia’s Simple Fracture(9 months of in-network pre-natal care and ahospital delivery)(a year of routine in-network care of a wellcontrolled condition)(in-network emergency room visit and follow upcare) 0n The plan’s overall deductible 30n Specialist (cost sharing)n Hospital (facility) cost sharing Check with youremployer 132n Other cost sharing 0n The plan’s overall deductible 30n Specialist (cost sharing)n Hospital (facility) cost sharing Check withyour employer 1,320n Other cost sharingn The plan’s overall deductible 0 30n Specialist (cost sharing)Check with yourn Hospital (facility) costemployersharing 595n Other cost sharingThis EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility Services Diagnostictests (ultrasounds and blood work) Specialistvisit (anesthesia)This EXAMPLE event includes serviceslike: Primary care physician office visits(including disease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy) 12,800Total Example CostIn the example, Peg would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Peg would pay is 0 420 0 132 552Total Example CostIn the example, Joe would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Joe would pay is 7,400 0 670 0 1,320 1,990Total Example CostIn the example, Mia would pay:Cost SharingDeductiblesCopaymentsCo-insuranceWhat isn’t coveredLimits or exclusionsThe total Mia would pay isThe plan would be responsible for the other costs of these EXAMPLE covered services. 1,900 37 260 0 595 8922516 of 9
ATTENTION: Language assistance services, free of charge, are available to you. Call1-877-411-3625. TTY/TDD: 711.Español (Spanish)ATENCIÓN: Usted tiene a su disposición, gratis, servicios de ayuda para idiomas. Llame al 1-877-411-3625 (TTY/TDD: 711).中文 (Traditional 協助服務。請致電 1-877-411-3625 (TTY/TDD: 711)。Pусский (Russian)ВНИМАНИЕ! Вам доступны бесплатные услуги переводчика. Звоните по тел. 1-877-411-3625 (служба текстового телефонаTTY/TDD: 711).Kreyòl Ayisyen (Haitian Creole)ATANSYON: Gen sèvis èd nan lang gratis ki disponib pou ou. Rele nimewo 1-877-411-3625 (TTY/TDD: 711).한국어 (Korean)주의: 귀하에게 언어 지원 서비스가 무료로 제공됩니다. 1-877-411-3625(TTY/TDD: 711)번으로 전화하십시오.Italiano (Italian)ATTENZIONE: sono disponibili servizi gratuiti di assistenza linguistica. Chiami il numero1-877-411-3625 (TTY/TDD: 711). ( אידיש Yiddish).(TTY/TDD: 711) 1-877-411-3625 רופט . זיינען דא צו באקומען פאר אייך , אהן קיין פרייז , שפראך הילף סערוויסעס : אכטונג বাাংলা (Bengali)মন োন োগ দি : ভোষো সহোয়তো পদিনষবোগুদি আপ োি জ য দব োমূনিয উপিব্ধ আনে। 1-877-411-3625 (TTY/TDD: 711)ম্বনি ফ োকরু ।Polski (Polish)UWAGA: dostępna jest bezpłatna pomoc językowa. Prosimy zadzwonić pod numer 1-877-411-3625 (TTY/TDD: 711).Group Health Incorporated (GHI), HIP Health Plan of New York (HIP), HIP Insurance Company of New York and EmblemHealth Services Company, LLC are EmblemHealth companies. EmblemHealth ServicesCompany, LLC provides administrative services to the EmblemHealth companies.10-9127 1/18
( العربية Arabic).(TTY/TDD: 711) أو 1-877-411-3625 اتصل على الرقم ، تتوفر لك خدمات المساعدة اللغوية مجانا : يرجى االنتباه Français (French)ATTENTION : une assistance d’interprétation gratuite est à votre disposition. Veuillez composer le1-877-411-3625 (TTY/TDD : 711). ( اردو Urdu) ) پر کال کر یں۔ TTY/TDD: 711( 1-877- 411-3625 مفت دستیاب ہیں۔ ، آپ کے لیے زبان سے متعلق اعانت کی خدمات : توجہ دیں Tagalog (Tagalog)NANANAWAGAN NG PANSIN: Mayroon kang magagamit na mga serbisyo para sa tulong sa wika nang walang bayad. Tawaganang 1-877-411-3625 (TTY/TDD: 711).Ελληνικά (Greek)ΠΡΟΣΟΧΗ: Διατίθενται για σας υπηρεσίες γλωσσικής βοήθειας, δωρεάν. Καλέστε το 1-877-411-3625 (για άτομα με προβλήματαακοής (TTY/TDD): 711).Shqip (Albanian)VINI RE: Shërbime ndihmore për gjuhën, falas, janë në dispozicionin tuaj. Telefononi në 1-877-411-3625 (TTY/TDD: 711).
ATTENTION: Language assistancefree of charge,are available to you. CallNOTICE TY/TDD:711.laws and does not discriminate on the basis of race, color, national origin, age,EmblemHealthcomplies withFederal civil rightsdisability, or sex. EmblemHealth does not exclude people or treat them differently because of race, color, national origin, age,Español or(Spanish)disability,sex.ATENCIÓN: Usted tiene a su disposición, gratis, servicios de ayuda para idiomas. Llame al 1-877-411-3625 (TTY/TDD: 711).EmblemHealth:中文 (TraditionalProvidesChinese)free aids and services to people with disabilities to ��服務。請致電 1-877-411-3625 (TTY/TDD: 711)。– Qualified sign language interpretersPусский(Russian) information in other formats (large print, audio, accessible electronic– WrittenВНИМАНИЕ! Вам доступны бесплатные услуги переводчика. Звоните по тел. 1-877-411-3625 (служба текстового телефонаformats, other formats)TTY/TDD: 711). Provides free language services to people whose first language is not English,Kreyòl Ayisyen (Haitian Creole)such as:ATANSYON: Gen sèvis èd nan lang gratis ki disponib pou ou. Rele nimewo 1-877-411-3625 (TTY/TDD: 711).– Qualified interpreters한국어–(Korean)Information written in other languages귀하에게 언어 지원 서비스가 무료로 제공됩니다. 1-877-411-3625(TTY/TDD: 711)번으로 전화하십시오.If주의:youneed these services, please call member services at 1-877-411-3625(TTY/TDD:Italiano (Italian) 711).ATTENZIONE: sono disponibili servizi gratuiti di assistenza linguistica. Chiami il numeroIf you believe that EmblemHealth has failed to provide these services or discriminated in another way on the basis of race, color,1-877-411-3625 (TTY/TDD: 711).national origin, age, disability, or sex, you can file a grievance with EmblemHealth Grievance and Appeals Department, PO Box 2844,New York, NY 10116, or call member services at 1-877-411-3625. (Dial 711 for TTY/TDD services.) You can file a grievancein ( אידיש Yiddish)person, by mail or by TDD: 711) 1-877-411-3625 רופט . זיינען דא צו באקומען פאר אייך , אהן קיין פרייז , שפראך הילף סערוויסעס : אכטונג help you. You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office of Civil Rightselectronicallythrough the Office of Civil Rights Complaint Portal, available at ocrportal.hhs.gov/ocr/portal/lobby.jsf or by mail orবাাংলা (Bengali)phone at U.S. Department of Health and Human Services, 200 Independence Avenue SW, Room 509F, HHH Building,মন োন োগ দি : নষবোগুদি আপ(dialোি 1-800-537-7697জ য দব োমূনিয 3625 (TTY/TDD: 711) ম্বনি ফ ো করু ।Washington,1-800-368-1019,for TTYComplaintforms are available at hhs.gov/ocr/office/file/index.html.Polski (Polish)UWAGA: dostępna jest bezpłatna pomoc językowa. Prosimy zadzwonić pod numer 1-877-411-3625 (TTY/TDD: 711).Group Health Incorporated (GHI), HIP Health Plan of New York (HIP),
Coverage Period: Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services EmblemHealth : PPO Coverage for: Individual/Family Plan Type: PPO OMB Control Numbers 1545-2229, 1210-0147, and 0938-1146 Released on April 6, 2016 251