Transcription
Charcot Foot: Clinical Clues, DiagnosticStrategies, and Treatment PrinciplesValerie S. Marmolejo, DPM, University Place, WashingtonJonathan F. Arnold, MD, Great River Wound and Hyperbaric Medicine Clinic, West Burlington, IowaMario Ponticello, DPM, and Charles A. Andersen, MD, Madigan Army Medical Center, Tacoma, WashingtonAcute Charcot neuroarthropathy of the foot and ankle is often difficult to diagnose because of limited findings in the patient history, physical examination, imaging, and laboratory studies. Delay intreatment results in the development of rigid foot and ankle deformities, increasing the risk of ulceration, infection, and major lower extremity amputation. Acute Charcot neuroarthropathy should besuspected in any patient 40 years or older with obesity and peripheral neuropathy who presents withan acutely swollen foot following minimal or no recalled trauma and who reports minimal to no pain,particularly if radiography and laboratory markers of infection are normal. Magnetic resonance imaging or computed tomography should be performed in these cases. If changes consistent with acuteCharcot neuroarthropathy are observed, prompt immobilization and/or referral to a foot and anklesubspecialist is needed to minimize sequelae. Immobilization should continue until lower extremityedema and warmth resolve, and serial radiography shows evidence of osseous consolidation. Intranasal calcitonin salmon may have a role as adjunctive therapy. Although controversial, surgery may beindicated if there is severe dislocation or instability, concern for skin breakdown, or failure of conservative treatment to obtain a stable, plantigrade foot. (Am Fam Physician. 2018;97(9):594-599. Copyright 2018 American Academy of Family Physicians.)Charcot neuroarthropathy of the foot and experiencing a first episode. Consideration ofankle is an inflammatory condition affectingthe periarticular soft tissues and bone in personswith peripheral neuropathy, resulting in osseous subluxation, dislocation, and fracture, if thelower extremity is not immobilized.1 One in fourcases of acute Charcot foot is misdiagnosed, mostoften as cellulitis, gout, deep venous thrombosis,or a minor sprain2-13 (Table 1 2-8,14-16), which delaysdiagnosis by an average of seven months.2,17-19Without prompt treatment, the condition oftenresults in development of rigid foot deformities(i.e., the classic rocker-bottom foot [Figure 120]),increasing the risk of major lower extremityamputation by 15- to 40-fold.6This article reviews key elements of the historyand physical examination, imaging, and laboratory studies that can increase clinical suspicionfor acute Charcot neuroarthropathy in patientsCME This clinical content conforms to AAFP criteria forcontinuing medical education (CME). See CME Quiz onpage 565.Author disclosure: No relevant financial affiliations.these elements can assist with early and accuratediagnosis. Prompt initiation of lower extremity immobilization, with referral to a foot andankle subspecialist as needed, can minimize thesequelae (e.g., rigid foot deformity, ulceration,infection, amputation) and improve patients’quality of life.2-6,8-11,14,17,20-29HistoryThe diagnosis of acute Charcot neuroarthropathy should be considered in any patient 40 yearsor older with obesity and peripheral neuropathywho presents with a unilateral swollen limb andminimal or no associated pain.2-12,14,18-20,22-25,29-37Diabetes mellitus is the most common cause ofperipheral neuropathy in the United States. Thelifetime prevalence of Charcot neuroarthropathyin patients with diabetes ranges from 0.1% to 10%,increasing to 29% to 35% if peripheral neuropathyis present.2,3,12,24-26,30,38,39 Compared with those whohave type 2 diabetes, patients with type 1 diabetestend to have diabetes for a longer duration (24 8.4 years vs. 13 8.1 years) and be younger (42 10.2 years vs. 59 7.8 years) when acute CharcotDownloadedfrom theAmericanFamily Physician website at www.aafp.org/afp.Copyright 2018 American Academy of FamilyPhysicians.For the9private, pVolume97, Number1, 2018mercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
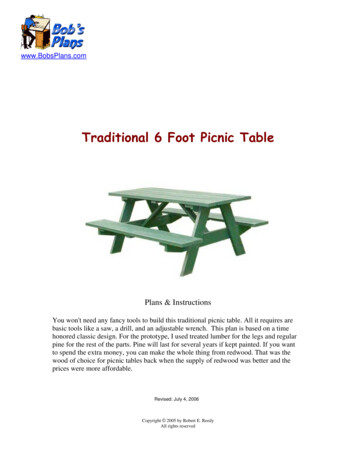
CHARCOT FOOTSORT: KEY RECOMMENDATIONS FOR PRACTICEEvidenceratingClinical recommendationReferencesIn patients with suspected acute Charcot neuroarthropathy, early and accurate diagnosis andprompt immobilization reduce the incidence of rigid foot deformity development, whichincreases patient quality of life and reduces the risk of ulceration, infection, and amputation.C2-6, 8-11, 14,17, 20-29The diagnosis of acute Charcot neuroarthropathy should be considered in any patient 40 yearsor older with obesity and peripheral neuropathy who presents with a unilateral swollen limband minimal or no associated pain.C2-12, 14,18-20, 22-25,29-37Acute Charcot neuroarthropathy should be considered in patients with recurrent cellulitis butno systemic or laboratory findings concerning for infection.C2-14, 22, 30,38, 42Bilateral weight-bearing radiography is recommended to allow for comparison between bothfeet in persons with suspected acute Charcot neuroarthropathy. Clinicians should look for signsof subtle subluxations or ligamentous avulsion, which denote impeding osseous instability.C2-4, 9-12, 14,20, 22-26,30, 38, 39A consistent, good-quality patient-oriented evidence; B inconsistent or limited-quality patient-oriented evidence; C consensus, diseaseoriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to http://www.aafp.org/afpsort.TABLE 1FIGURE 1Common Misdiagnoses of Acute ellulitisErysipelasAcute inflammatory arthritisDeep venousthrombosisOsteomyelitisGoutFractureSeptic arthritisPlantar enous insufficiencyInformation from references 2 through 8, and 14 through 16.neuroarthropathy develops.6,31 Patients with type 1 diabetesalso tend to be less obese and more prone to recurrent eventsof Charcot neuroarthropathy than patients with type 2 diabetes.32 An A1C level greater than 9% is associated with a 30%increased risk of developing Charcot neuroarthropathy.31Misdiagnosis of acute Charcot neuroarthropathy mayoccur when it presents in patients who have peripheralneuropathy from etiologies other than diabetes, such asalcoholism, use of chemotherapeutic agents, inherited disorders, or trauma.34 Other factors that increase the risk ofacute Charcot neuroarthropathy include a history of footulceration; retinopathy; nephropathy, renal failure, or renaltransplantation; rheumatoid arthritis; iron deficiency anemia; or obesity.6,12,31 Between 25% and 50% of patients recallno trauma or inciting event, and the same number do notreport pain.2,5-10,14,17-20,22,23,39 If an inciting event is recalled, itis often minor, such as walking a long distance or sustaining a minor sprain. Patients who recall an inciting event areMay 1, 2018 Volume 97, Number 9Classic rocker-bottom foot associated with untreatedCharcot neuroarthropathy.Reprinted with permission from Sommer TC, Lee TH. Charcotfoot: the diagnostic dilemma [published correction appears inAm Fam Physician. 2002;65(12):2436-2438]. Am Fam Physician.2001;64(9):1593.more likely to report pain, often described as a constant discomfort not severe enough to stop ambulation.5,9,12Physical Examination and Laboratory StudiesPatients with acute Charcot neuroarthropathy are usuallyafebrile with normal vital signs. More than 70% of the time,patients have unilateral lower extremity edema (Figure 2)with associated erythema and increased warmth (2 C to8 C [3.6 F to 14.4 F]) with no open wound.2,4,10,11,14,17,18,20-22,39Peripheral neuropathy can be confirmed with use of aSemmes-Weinstein monofilament test. Deep tendon reflexesare also severely impaired, particularly the Achilles tendonreflex.6 Lower extremity edema extends down to the foot,which is particularly swollen around the affected joints.14www.aafp.org/afp American Family Physician 595
CHARCOT FOOTFIGURE 2ABExamples of increased edema of the left lower extremity compared withthe right secondary to acute Charcot neuroarthropathy (A and B).FIGURE 3ABPatients with these findings may havebeen previously treated for cellulitis.Acute Charcot foot should be considered in patients with recurrent cellulitisbut no systemic or laboratory findingsconcerning for infection.2-14,22,30,31,38Antibiotic therapy does not resolvesymptoms, which may have led to previous hospital admission. Symptomresolution may occur during hospitalization because patients spend moretime in bed; however, symptoms mayreturn after discharge when patientsare ambulatory, which may lead to amisdiagnosis of recurrent cellulitis.Although acute Charcot neuroarthropathy can coexist with cellulitis,osteomyelitis, or open wounds of thelower extremity, the latter two are morecommon with recurrent episodes.Imaging StudiesVENOUS DUPLEXULTRASONOGRAPHYVenous duplex ultrasonography maybe performed when deep venousthrombosis is suspected. Resultsshould be normal in acute Charcotneuroarthropathy.RADIOGRAPHYRadiography should be the primaryimaging study. Although the characteristic bony destruction of Charcotneuroarthropathy can take six to 12months to become visible on radiography, initial imaging serves as a baseline and allows fordetection of subtle changes denoting instability. Subtle subluxations and small flecks of bone secondary to ligamentousavulsion fractures may be present, signaling instability andimpending osseous destruction2-4,9-12,14,17,20-26,30,38,39 (Figures3 and 4). More than 60% of all Charcot neuroarthropathyevents affect the midfoot.12,24 Osseous overlap in the midfoot can make subtle subluxations and minimally displacedfractures difficult to visualize.41-43 For this reason, bilateralweight-bearing radiography is recommended for comparison of both feet.2,3,17,20,21Compared with the right foot (A), bilateral foot radiography revealsincreased soft tissue volume and irregularities about the tarsometatarsaljoint of the left foot (B) secondary to acute Charcot neuroarthropathy.Pedal pulses are most often palpable and can be describedas bounding if unobscured by edema.6 The increase in skintemperature can assist in diagnosis and resolution of theCharcot process.35 Less expensive, industrial-grade, noncontact infrared thermometers have been shown to be as reliable in detecting temperature of the skin as a more expensivemedical infrared thermometer.36Erythema secondary to the inflammation of acute Charcotneuroarthropathy can be differentiated from infection byelevating the affected extremity above the level of the heartfor five to 10 minutes. Erythema secondary to acute Charcot neuroarthropathy will dissipate, whereas erythema frominfection will not.13 Laboratory markers of infection, such aswhite blood cell count, C-reactive protein level, and erythrocyte sedimentation rate, are usually normal.11,12,14,17,25,38,40596 American Family PhysicianMAGNETIC RESONANCE IMAGINGMagnetic resonance imaging (MRI) in the acute phase ofCharcot neuroarthropathy can demonstrate periarticularwww.aafp.org/afp Volume 97, Number 9 May 1, 2018
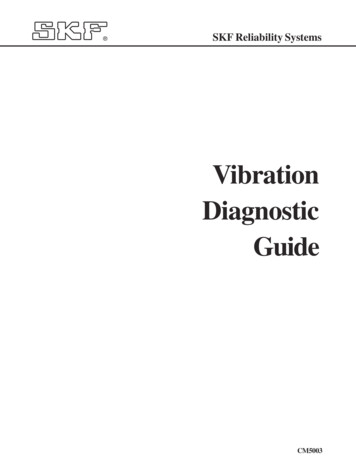
CHARCOT FOOToften negative.4,12 There is limited literature available on theaid of nuclear bone scanning in the diagnosis of acute Charcot neuroarthropathy. Because of the nonspecific natureof the study, radiography and MRI are recommended overnuclear medicine studies.FIGURE 4TreatmentIMMOBILIZATIONOblique radiographs of acute Charcot foot initiallyread as normal; arrows identify ligamentous avulsionfractures with subsequent medial dislocation of thenavicular.bone marrow edema (Figure 5), adjacent soft tissue edema,joint effusion, and microtrabecular or stress fractureswhen radiography results are normal.5,24,33,37,44,45 A studythat followed 71 cases (59 patients) of acute Charcot neuroarthropathy over 12 years concluded that radiographywas insufficient in diagnosing midfoot fractures; that anybone marrow edema present on MRI was likely to progressto cortical fracture if unprotected ambulation was allowed;and that cortical fractures were a significant marker forimpending deformity development.33 Performing MRIis recommended when radiography results are inconclusive and patients exhibit key clinical elements outlined inTable 2.The mainstay of treatment of Charcot neuroarthropathy isimmobilization in a total contact cast, which increases thetotal surface area of contact to the entire lower extremity,distributing pressure away from the foot. Immobilizationshould continue until lower extremity edema and warmthresolve and serial radiography shows evidence of osseousconsolidation, which typically occurs after three to fourmonths but can take up to 12 months.2-5,10,13,14,17,20,21,26-30,33Computed tomography and MRI may also be used todetermine resolution. Bone scanning is not recommendedfor determining resolution because osseous remodeling cancontinue for up to one year, resulting in prolonged increaseduptake in the affected area due to remodeling. Removablewalking boots and braces that incorporate the entire lowerleg have also been used and are better tolerated by patientsthan cast immobilization, in addition to reducing the riskof iatrogenic complications that can occur with casting.28,38However, these removable devices require a longer durationof immobilization.18,23,28SURGERYAlthough controversial, surgery may be indicated in theacute phase of Charcot neuroarthropathy in cases ofsevere dislocation or instability, if there is concern for skinFIGURE 5COMPUTED TOMOGRAPHYComputed tomography is useful for visualizing all bones ofthe foot, particularly the midfoot, which is difficult to seewell on radiography.41-43 It is recommended when MRI iscontraindicated for the patient.BONE SCANSIncreased tracer uptake to the affected joint occurs in allthree phases of a bone scan when acute Charcot neuroarthropathy is present. White blood cell–tagged scans areMay 1, 2018 Volume 97, Number 9Magnetic resonance imaging shows increased bonemarrow edema (circled in white) consistent withacute Charcot neuroarthropathy of the midfoot.www.aafp.org/afp American Family Physician 597
CHARCOT FOOTThis article updates previous articles on this topic by Sommerand Lee, 20 and Caputo, et al.14TABLE 2Key Elements That Should IncreaseClinical Suspicion for Acute CharcotNeuroarthropathyAge 40 years or older for patients with type 1 diabetesmellitusAge 50 years or older for patients with type 2 diabetesComputed tomography shows osseous fracture(s), particularly about the midfootDiagnosis of type 1 or 2 diabetes for 10 years or moreIncreased tracer uptake in all three phases of a bone scanand negative white blood cell–tagged scanMagnetic resonance imaging shows periarticular bonemarrow edema, which enhances on postcontrast imagesMinimal or no foot painNo systemic or laboratory findings concerning forinfectionNo trauma or only minor trauma reportedObesityPeripheral neuropathy of any etiologyRadiography reveals increased soft tissue volume, subtlesubluxations, or ligamentous avulsion fractures, particularly about the midfootTreatment for recurrent cellulitisUnilateral edematous, erythematous, warm limb with noopen woundsVenous duplex ultrasonography is negative for deepvenous thrombosisbreakdown, or if conservative treatment fails to obtain astable, plantigrade foot.1,2,9,17,23,46-48BISPHOSPHONATESA systematic review of 10 small heterogeneous studies concluded that the adjunctive use of bisphosphonates duringconservative management of acute Charcot neuroarthropathy was not effective.49INTRANASAL CALCITONINA single randomized controlled trial of 32 patients withacute Charcot neuroarthropathy who were treated with castimmobilization and oral calcium supplementation compared 200 IU of intranasal calcitonin salmon daily withno adjunctive therapy. A significantly greater reduction inmarkers of bone turnover in the intervention group wasnoted at three and six months, suggesting that daily intranasal calcitonin may be an effective adjunctive treatment.50However, no studies of calcitonin have reported patientoriented outcomes.598 American Family PhysicianData Sources: A PubMed search was performed of peerreviewed journals, restricted to the English language with norestriction on date, using the key words acute, stage 0, Charcot,and Charcot neuroarthropathy. Each reference was manuallysearched for additional pertinent references. This review includedstudies of all levels of evidence. We also searched the Agencyfor Healthcare Research and Quality evidence reports, U.S. Preventive Services Task Force, Cochrane Database of SystematicReviews, Clinical Evidence, evidence-based guidelines from theNational Guideline Clearinghouse, and the Institute for ClinicalSystems Improvement. Search date: April 10, 2017.The opinions or assertions contained herein are the private viewsof the authors and are not to be construed as official or reflectingthe views of the Department of the Army or the Department ofDefense.The AuthorsVALERIE S. MARMOLEJO, DPM, is a freelance medical writerwith Scriptum Medica, University Place, Wash.JONATHAN F. ARNOLD, MD, ABPM-UHM, CWSP, is the medical director of Great River Wound and Hyperbaric MedicineClinic, West Burlington, Iowa.MARIO PONTICELLO, DPM, FACFAS, FAPWCA, is chief of thelimb preservation service at Madigan Army Medical Center,Tacoma, Wash.CHARLES A. ANDERSEN, MD, FACS, FAPWCA, is chief ofwound care and a staff vascular surgeon at Madigan ArmyMedical Center.Address correspondence to Valerie S. Marmolejo, DPM, Scriptum Medica, 9416 42nd St. W., University Place, WA 98466(e-mail: vlsdpm@gmail.com). Reprints are not available fromthe authors.References1. Rogers LC, Frykberg RG, Armstrong DG, et al. The Charcot foot in diabetes. Diabetes Care. 2011;34(9):2123-2129.2. Pakarinen TK, Laine HJ, Honkonen SE, Peltonen J, Oksala H, Lahtela J.Charcot arthropathy of the diabetic foot. Current concepts and reviewof 36 cases. Scand J Surg. 2002;91(2):195-201.3. Wukich DK, Sung W, Wipf SA, Armstrong DG. The consequences ofcomplacency: managing the effects of unrecognized Charcot feet.Diabet Med. 2011;28(2):195-198.4. Chantelau E. The perils of procrastination: effects of early vs. delayeddetection and treatment of incipient Charcot fracture. Diabet Med.2005;22(12):1707-1712.5. Chantelau E, Richter A, Ghassem-Zadeh N, Poll LW. “Silent” bone stressinjuries in the feet of diabetic patients with polyneuropathy: a report on12 cases. Arch Orthop Trauma Surg. 2007;127(3):171-177.6. Foltz KD, Fallat LM, Schwartz S. Usefulness of a brief assessment batteryfor early detection of Charcot foot deformity in patients with diabetes.J Foot Ankle Surg. 2004;43(2):87-92.7. Gill G, Benbow S, Tesfaye S, Kaczmarczyk E, Kaye L. Painless stress fractures in diabetic neuropathic feet. Postgrad Med J. 1997;73(858):241-242.www.aafp.org/afp Volume 97, Number 9 May 1, 2018
CHARCOT FOOT8. Giurini JM, Chrzan JS, Gibbons GW, Habershaw GM. Charcot’s diseasein diabetic patients. Correct diagnosis can prevent progressive deformity. Postgrad Med. 1991;89(4):163-169.9. Lee L, Blume PA, Sumpio B. Charcot joint disease in diabetes mellitus.Ann Vasc Surg. 2003;17(5):571-580.10. Shah MK, Hugghins SY. Charcot’s joint: an overlooked diagnosis. J LaState Med Soc. 2002;154(5):246-250.11. Milne TE, Rogers JR, Kinnear EM, et al. Developing an evidence-basedclinical pathway for the assessment, diagnosis and management ofacute Charcot Neuro-Arthropathy: a systematic review. J Foot AnkleRes. 2013;6(1):30.12. Baglioni P, Malik M, Okosieme OE. Acute Charcot foot. BMJ.2012;344:e1397.13. Brodsky JW. Outpatient diagnosis and care of the diabetic foot. InstrCourse Lect. 1993;42:121-139.14. Caputo GM, Ulbrecht J, Cavanagh PR, Juliano P. The Charcot foot indiabetes: si
May 01, 2018 · Mario Ponticello, DPM, and Charles A. Andersen, MD, Madigan Army Medical Center, Tacoma, Washington CME This clinical content conforms to AAFP