Transcription
713.295.2295 1.888.760.2600COMMUNITYHEALTH CHOICE
TABLE OF CONTENTS 2 Table of ContentsIn this issue3Community NewsRendering Provider RequirementClaim Refund/Recoupment RequestsEnhanced Claims Requirements for CHIP Perinate ClaimsFQHC ReminderNew Electronic Payment MethodSterilization Consent FormsHHSC Notifications35Securing Your Web Portal AccessHealth Alert from DSHS: Infant Botulismand History of Honey PacifiersProvider Directory AccuracyFetal Testing Procedure Code UpdateProvider Access and After-Hours Availability38Shingles Vaccine Procedure Code toBecome a Medicaid BenefitIntegrating Postpartum Depression Screeninginto Routine Infant Medical CheckupsCorrection to Previous UpdateTHSteps Mental Health ScreeningChange for 12 to 18 Year OldsUpdate to TMPPMTHSteps Checkup TimelinessTexas Health Steps Postpartum Depression Screening BenefitTHSteps Checkup Documentation –Essential to Medical RecordsMedical AffairsTHSteps Medical Checkup Periodicity ScheduleCommunity Health Choice Prior AuthorizationGuide Changes Effective January 1, 2019Children of Traveling FarmworkersTherapy Wait ListTHSteps Provider Outreach Referral Service and How it WorksHead Start ProgramTHSteps Medical Checkup Billing Procedure CodesPharmacy CornerBilling THSteps Medical Checkup andOther Services on the Same DayWhat’s New for 2019?Pharmacy Prior Authorization Fax FormsHHSC’S Medical Transportation Program for Medicaid MembersDrug Samples23Beacon CornerSmoking and Mental Health2526Texas Health StepsCommunity AnnouncementSubstance Abuse Disorder Benefits toChange for Texas Medicaid22Network Management/Provider OperationsReminder: Vaccine Coverage for CHIP Perinatal MembersStanding Order Update for Medicaid Mosquito Repellent20ClaimsNational Drug Code (NDC)A New Look for a New Year!632CLIA RequirementComplianceCommunity’s Transportation Services for CHIP Members45Social Determinants of Health46Provider Continuing EducationAccess to Medical RecordsIntegrating Postpartum Depression Screeninginto Routine Infant Medical CheckupsMedical Supplies Physician Order Formfor Health Services (Title XIX)Online Provider Education — FreeContinuing Education (CE) HoursSpecial Investigations UnitTMHP Online Provider EducationPerformance ExcellenceVendor Drug Program Continuing Educationfor Prescribing ProvidersHEDIS Criteria: Weight Assessment and Counseling forNutrition and Physical Activity for Children and AdolescentsAntibiotic UseFocus on Moms and Babies: A Provider Tag-Team ApproachCommunityHealthChoice.org
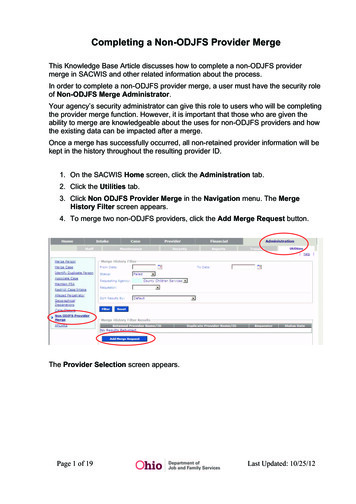
COMMUNITY NEWS 3 Table of ContentsCLIA RequirementBeginning January 1, 2019, Community will denyclaims for CLIA-waived lab services if Providerdoes not have a valid CLIA certification.Rendering ProviderRequirementBeginning February 1, 2019 Community willrequire Providers to bill using a RenderingProvider NPI for all claims submitted.Enhanced Claims Requirementsfor CHIP Perinate ClaimsObstetric Delivery Enhanced Claim Requirementsfor CHIP Perinate Program Claims:CHIP Perinate mothers are entitled to a maximum of2 postpartum visits. CHIP Perinate mothers' eligibilityends at the end of the month the baby was born.If a Provider calls to check benefits after themonth of the baby’s birth, they will be advisedthe CHIP Perinate mother is not eligible.CHIP Perinate mothers may receive theirpostpartum visits after their eligibility ends (atthe end of the month of the baby’s birth).Effective January 1, 2019, in order to bereimbursed for the postpartum visits, Providersmust bill using the CPT delivery codes that includepostpartum care. See below for a list of codes.The reimbursement amount for the procedure codesbelow includes both postpartum care visits. If the Providerbills any other code and the date of service is after theCHIP Perinate mother’s eligibility has ended, the Providerwill not receive payment for the postpartum care.If the claim was submitted with the incorrect code,Providers may re-submit the original delivery claim withthe correct code within the 120-day appeal deadline.Acceptable Bundled CodesProcedure CodeCode Description59410Vaginal delivery only (with or without episiotomy and/or forceps); including postpartum care59515C-Section delivery only; including postpartum care59614Vaginal delivery only, after previous Cesarean delivery (with or withoutepisiotomy and/or forceps); including postpartum care59622Cesarean delivery only, following attempted vaginal delivery afterprevious Cesarean delivery; including postpartum careAdditional Claims Information Claims billed with the delivery codes 59409,59514, 59612, and 59620 will be denied. Global delivery codes (CPT Codes 59400, 59510,59610, 59618) will continue to not be reimbursable. Corrected claims can be submitted within 120days from the Explanation of Payment (EOP) datefor payment with the bundled procedures. Applicable modifier (U1, U2, U3) is required.Should you have additional questions, please contactyour Provider Engagement Representative or callthe Provider Services line at 713.295.2295.CommunityHealthChoice.org
COMMUNITY NEWS 4 Table of ContentsNew ElectronicPayment MethodIn early 2019, Community will partner with ChangeHealthcare and ECHO Health, Inc. to provide thesenew electronic methods. Many of our Providersalready work with Change Healthcare today.Below we have outlined the payment optionsand any action items needed by your office.1Virtual Card Services Going forward, if we don’thave a documented choice of payment for you,the default method of payment will now be virtualcard rather than a paper check. Virtual cards allowyour office to process our payments as credit cardtransactions. Virtual card payments are generallyreceived 7-10 days earlier than paper checks sincethere are no print and mail delays. Your office willreceive fax notifications, each containing a virtual cardwith a number unique to that payment transaction.Once the number is received, you simply enter thecode into your office’s credit card terminal to processpayment as a regular card transaction. If the card isnot processed within 30 days, the virtual transactionwill be voided and a paper check will automaticallybe sent to your office. To avoid delay please processthe card or notify us of your preference from theother options below. Normal transaction fees applybased on your merchant acquirer relationship.2EFT/ACH You can enroll for EFT/ACH by providingyour banking account information, and once yourenrollment is verified begin receiving payment viaelectronic funds transfer (EFT). Setting up EFT isa fast and reliable method to receive payment. Ifyou wish, each time a payment is made to you,you can elect to receive an email notification.You will need to provide a Change Healthcarepayment draft number and payment amountas part of the enrollment authentication.3Paper Check If there are concerns with electronicpayments, you must elect to opt out of Virtual CardServices or remove your EFT enrollment to receivepaper checks and paper explanation of payments.CommunityHealthChoice.org
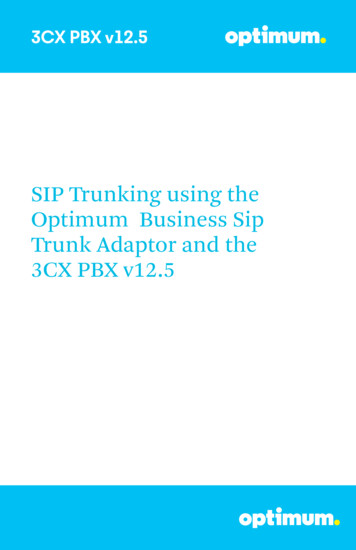
COMMUNITY NEWS 5 Table of ContentsA New Look for a New Year!Community is pleased to introduce our newly redesignedMember identification cards effective January 1, 2019. Weare excited to launch new Member identification cardsthat are easier to read for both Providers and Members.The new cards feature the following key components:Please feel free to contactyour Provider EngagementRepresentative if youhave additional questionsand concerns regardingour new look. Provider’s name, phone number, and address soMembers can quickly contact your practice Link for Members to navigate theirpersonalized Community account Instant Access for pharmacy andbehavioral healthcare needsRedesigned STAR Member IDKealthandHumanTEXASServicesNameMember IDPCP Name nn -vVl"Ul'IVl'llllHEAL1H CHOICEHelpful numbers Números útilesMember Services 24/7 Servicios para Miembros 24/7Talk to a nurse 24/7 Hable con una enfermera 24/71.888.760.2600 (toll-free gratis)1.888.332.2730Behavioral Health 24/7 Servicios para salud mental 24/71.877.343.3108DOBPCP Effective DateIn case of emergency, call 9-1-1 or go to the closest emergency room. After treatment, call your PrimaryCare Provider within 24 hours or as soon as possible.En caso de emergencia, llame al 9-1-1 o vaya a la sala de emergencias más cercana. Después de recibirtratamiento, llame al Proveedor de Cuidado Primario dentro de 24 horas o tan pronto como sea posible.PCP PhonePCP AddressProvider ServicesEligibility, authorizations, benefts and claims:Provider.CommunityHealthChoice.org 713.295.2295Send claims to: Community Health Choice, Inc. P.O. Box 301424 Houston, TX 77230Electronic claims: Payer ID 48145For more information about your plan, log in to your Member Account at /Para más información sobre su plan, ingrese a su cuenta de Miembro enCommunityHealthChoice.org.TDIPharmacy: Navitus Health Solutions1.877.908.6023BIN: 610602PCN: NVTRXGroup: CHXRedesigned CHIP Member ID CHIP 1 TEXAS:::.::"'"" 'NameMember IDPCP NameCOMMUNfIY "'4HEALTH CHOICEMember Services 24/7 Servicios para Miembros 24/7Talk to a nurse 24/7 Hable con una enfermera 24/71.888.760.2600 (toll-free gratis)1.888.332.2730Behavioral Health 24/7 Servicios para salud mental 24/7PCP Effective Date1.877.343.3108In case of emergency, call 9-1-1 or go to the closest emergency room. After treatment, call your PrimaryCare Provider within 24 hours or as soon as possible.En caso de emergencia, llame al 9-1-1 o vaya a la sala de emergencias más cercana. Después de recibirtratamiento, llame al Proveedor de Cuidado Primario dentro de 24 horas o tan pronto como sea posible.PCP PhonePCP AddressCo-Payment: Office VisitHospitalHelpful numbers Números útilesERVisionGeneric/BrandSpecialtyFor more information about your plan, log in to your Member Account at /Para más información sobre su plan, ingrese a su cuenta de Miembro enCommunityHealthChoice.org.Provider ServicesEligibility, authorizations, benefts and claims:Provider.CommunityHealthChoice.org 713.295.2295Send claims to: Community Health Choice, Inc. P.O. Box 301424 Houston, TX 77230Electronic claims: Payer ID 48145TDIPharmacy: Navitus Health Solutions1.877.908.6023BIN: 610602PCN: NVTRXGroup: CHXCommunityHealthChoice.org
HHSC NOTIFICATIONS 6 Table of ContentsReminder: Vaccine Coverage for CHIP Perinatal MembersIn 2017, a notice was shared regarding coverageof vaccines for CHIP Perinatal (CHIP-P) Members.This notice serves as a reminder regarding whichvaccines are covered for CHIP-P Members.Key Details:The Tetanus, Diphtheria, and Acellular Pertussis(Tdap) vaccine is part of routine prenatal careand is a covered benefit in CHIP-P.This vaccine is recommended by the Centers forDisease Control and Prevention (CDC), AmericanAcademy of Pediatrics (AAP), and AmericanCollege of Obstetricians and Gynecologists(ACOG) as part of routine prenatal care: CDC: cinated.html ACOG: a-and-Pertussis-VaccinationGuidance:CHIP MCOs must ensure their Member services staff andProviders are aware this is a covered benefit and thatclaims are being appropriately reimbursed for this service.Resources:Original Notice: ine AAP: unityHealthChoice.org
HHSC NOTIFICATIONS 7 Table of ContentsHealth Alert from DSHS: Infant Botulismand History of Honey PacifiersNovember 16, 2018BACKGROUND: Honey can contain spores ofClostridium botulinum, an organism that producesa potent neurotoxin known to cause severe illnessin infants. Infant botulism occurs when C. botulinumspores in food, dust, or other materials are inhaledor ingested and germinate in the gut of infants whohave not yet developed mature intestinal flora. For thisreason, parents are advised not to feed honey (raw orotherwise) to children younger than 12 months old.Infant botulism: Symptoms of botulism in infantsunder 12 months of age typically start with constipationand may include poor feeding and/or weak sucking,weakness, drooping eyelids, loss of head control anddifficulty breathing. Severity can range from mildillness with gradual onset to paralysis, respiratoryfailure, and death. Prompt recognition of a suspectcase, administration of antitoxin, and initiation ofsupportive care can halt progression of the disease.The Texas Department of State Health Services willcoordinate confirmatory testing at the DSHS laboratory.To obtain the antitoxin (Baby BIG) for treatment,physicians can contact the DSHS Emerging and AcuteInfectious Disease Branch or the California InfantBotulism Treatment and Prevention Program.Recent trends: Cases are rare; between 2013 and 2017,Texas has averaged 7 to 8 cases of infant botulismannually. However, since August, four patients havebeen treated for infant botulism and have a historyof using a honey pacifier purchased in Mexico.Investigators noted that these honey pacifiers andother food-containing pacifiers are available forsale at retailers as well as online, and that parentsmay not be aware of their potential danger.Recommendations: Infants (children less than 12months of age) should not be given honey, or pacifierscontaining honey or other food products, because ofthe risk of contracting infant botulism. Consumptionof honey is widely recognized as a risk factor for infantbotulism by healthcare and public health professionals.Infant botulism is a serious illness that requiresurgent medical attention. All suspect cases shouldbe immediately reported to public health officials.For more information, contact DSHS at 512.776.7676.CommunityHealthChoice.org
HHSC NOTIFICATIONS 8 Table of ContentsStanding Order Update for Medicaid Mosquito RepellentAn update to the 2018-19 Texas Medicaid Standing Order for Mosquito Repellent isnow available for use with the Texas Medicaid mosquito repellent benefit. The benefitis for people enrolled in Medicaid (both traditional and managed care) and CHIP.The revised standing order is signed by Dr. Lisa Glenn. The document iseffective Nov. 1 and is valid for one year from the date it was signed. Theprevious standing order signed by Dr. Rajendra Parikh is valid throughOct. 31. Pharmacies may directly obtain a copy of the renewed standingorder upon request by emailing VDP Formulary@hhsc.state.tx.us.Refer to the Mosquito Repellent Benefit for Pharmacies (PDF) for more information: A prescription from a valid healthcare Provider is required for any pharmacy/pharmacist not operating under a standing order, for the dispensingof mosquito repellent to people enrolled in Medicaid or CHIP People enrolled in the Healthy Texas Womenprogram do not require a prescription People enrolled in the CSHCN program require a prescriptionfor mosquito repellent from a healthcare Provider.CommunityHealthChoice.org
HHSC NOTIFICATIONS 9 Table of ContentsFetal Testing Procedure Codes 59020 and59025 Updated Effective January 1, 2019Information posted November 16, 2018Note: Texas Medicaid managed care organizations(MCOs) must provide all medically necessary,Medicaid-covered services to eligible clients.Administrative procedures such as prior authorization,pre-certification, referrals, and claims/encounter datafiling may differ from traditional Medicaid (fee-forservice) and from MCO to MCO. Providers shouldcontact the client's specific MCO for details.Effective for dates of service on or after January 1,2019, the interpretation and technical componentsof fetal testing procedure codes 59020 and 59025will become benefits of Texas Medicaid for femaleclients who are 10 through 55 years old.Procedure codes 59020 and 59025 will beupdated to include the following:Procedure CodeComponentPlace of ServicePayable Provider Types59020*InterpretationOffice, inpatient hospital,outpatient hospitalNurse practitioner (NP),clinical nurse specialist(CNS), physician assistant(PA), physician, andcertified nurse midwife(CNM) ProvidersTechnicalInpatient hospital,outpatient hospitalNP, CNS, PA, physician,CNM ProvidersTotal**Inpatient hospital,outpatient hospitalNP, CNS, PA, physician,CNM ProvidersInterpretation, technicalOffice, inpatient hospital,outpatient hospitalNP, CNS, PA, physician,CNM Providers59025* The total component of procedure code 59020 will remain a benefit in the inpatient and outpatient hospitalsettings. **The total component of procedure code 59025 will also remain a benefit in the office setting.The total and technical components of procedure codes59020 and 59025 will be denied when submitted forthe same date of service as an ambulatory surgicalcenter claim for the same procedure code.Note: New benefts that are adopted by TexasMedicaid must complete the rate hearingprocess to receive public comment on proposedTexas Medicaid reimbursement rates.The total component of procedure codes 59020 and59025 will be denied when submitted for the samedate of service, by the same Provider, as deliveryprocedure code 59410, 59515, 59614, or 59622.After the rate hearing, expenditures must be approvedbefore the rates are adopted by Texas Medicaid.For more information, call the TMHPContact Center at 1.800.925.9126.CommunityHealthChoice.org
HHSC NOTIFICATIONS 10 Table of ContentsProcedure Code T4528 with Modifier U1No Longer a Benefit January 1, 2019Information posted November 16, 2018Note: Texas Medicaid managed care organizations(MCOs) must provide all medically necessary, Medicaidcovered services to eligible clients. Administrativeprocedures such as prior authorization, precertifcation, referrals, and claims/encounter datafling may differ from traditional Medicaid (fee-forservice) and from MCO to MCO. Providers shouldcontact the client's specifc MCO for details.Effective for dates of service on or after January 1, 2019,procedure code T4528 with modifier U1 will no longerbe a benefit of Texas Medicaid or the Children withSpecial Health Care Needs (CSHCN) Services Program.Procedure code T4528 without modifier U1 willremain a benefit of Texas Medicaid and the CSHCNServices Program. Providers may refer to the currentTexas Medicaid Provider Procedures Manual,Durable Medical Equipment, Medical Supplies,and Nutritional Products Handbook, subsection2.2.14.2, “Diapers, Briefs, Pull-ons, and Liners” forbenefit information about procedure code T4528.For more information, call the TMHP Contact Centerat 1.800.925.9126 or the TMHP-CSHCN ServicesProgram Contact Center at 1.800.568.2413.Shingles Vaccine Procedure Code 90750 to Becomea Benefit of Texas Medicaid January 1, 2019Information posted November 16, 2018Note: Texas Medicaid managed care organizations(MCOs) must provide all medically necessary, Medicaidcovered services to eligible clients. Administrativeprocedures such as prior authorization, precertifcation, referrals, and claims/encounter datafling may differ from traditional Medicaid (fee-forservice) and from MCO to MCO. Providers shouldcontact the client's specifc MCO for details.Note: New benefts that are adopted by Texas Medicaidmust complete the rate hearing process to receive publiccomment on proposed Texas Medicaid reimbursementrates. After the rate hearing, expenditures must beapproved before the rates are adopted by Texas Medicaid.For more information, call the TMHPContact Center at 1.800.925.9126.Effective for dates of service on or after January 1, 2019,shingles vaccine procedure code 90750 will becomea benefit for clients who are 50 years of age and olderas follows:Place of ServiceWhen Services are Provided byOfficeNurse practitioner, clinicalnurse specialist, physicianassistant, physician, pharmacy,pharmacist, and certifiednurse midwife ProvidersHomeNurse practitioner, clinical nursespecialist, physician assistant,physician, and federally qualifiedhealth center ProvidersOutpatient hospitalHospital ProvidersOther locationNurse practitioner, clinical nursespecialist, physician assistant,and physician ProvidersCommunityHealthChoice.org
HHSC NOTIFICATIONS 11 Table of ContentsSubstance Use Disorder Benefits to Changefor Texas Medicaid January 1, 2019Information posted November 16, 2018Substance Use Disorder Benefits to Changefor Texas Medicaid January 1, 2019Information posted November 16, 2018Note: Texas Medicaid managed care organizations(MCOs) must provide all medically necessary,Medicaid-covered services to eligible clients.Administrative procedures such as prior authorization,pre-certification, referrals, and claims/encounter datafiling may differ from traditional Medicaid (fee-forservice) and from MCO to MCO. Providers shouldcontact the client's specific MCO for details.Effective for dates of service on or afterJanuary 1, 2019, substance use disorder (SUD)benefits will change for Texas Medicaid.Overview of Benefit ChangesMajor changes to this medical benefitpolicy include the following: Updated benefit language Prior authorization changes Procedure code updates Diagnosis code updatesUpdated Benefit LanguageSUDs are chronic, relapsing medical illnesses that requirean array of best practice medical and psychosocialinterventions of sufficient intensity and duration toachieve and maintain remission and support progresstoward recovery. SUD may include problematic useof alcohol, prescription drugs, illegal drugs (e.g.,cannabis, opioids, stimulants, inhalants, hallucinogens,“club” drugs, other synthetic euphoriants), and othersubstances that may be identified in the future.Treatment for SUD is a benefit of Texas Medicaid forindividuals who meet the criteria for a substancerelated disorder, as outlined in the current editionof the American Psychiatric Association’s Diagnosticand Statistical Manual of Mental Disorders (DSM).SUD treatment services are individualized, ageappropriate medical and psychosocial interventionsdesigned to treat an individual’s problematic use ofalcohol or other drugs, including prescription medication.SUD services may include the following: Withdrawal management services Individual and group SUD counselingin an outpatient setting Residential treatment services Medication assisted treatment Evaluation and treatment (or referral for treatment) forco-occurring physical and behavioral health conditionsLevel of care (e.g., outpatient, residential, inpatienthospital) and specific services provided must adhere tocurrent evidence-based industry standards and guidelinesfor SUD treatment, such as those outlined in the currentedition of the American Society of Addiction Medicine’sTreatment Criteria for Addictive Substance-Relatedand Co-Occurring Conditions, as well as the licensurerequirements outlined in Texas Administrative Code (TAC)Title 25 Chapter 448 pertaining to Standards of Care.SUD treatment services (outpatient or residential)may only be delivered in a licensed chemicaldependency treatment facility (CDTF). Medicationassisted treatment (MAT) may also be delivered byappropriately trained physicians, nurse practitioners(NPs), clinical nurse specialists (CNSs), andphysician assistants (PAs) in the office setting.SUD withdrawal management in an inpatient hospitalsetting may be provided for individuals who meethospital level of care requirements as a result of theseverity of their withdrawal syndrome and/or the severityof their co-occurring conditions. These services maybe reimbursed as general hospital inpatient services.CommunityHealthChoice.org
HHSC NOTIFICATIONS 12 Table of ContentsThe treatment setting and the intensity or level ofservices will vary depending on the severity of theindividual’s SUD and what is clinically appropriate.The intensity or level of services refers to thenumber of hours of services per week, as well asthe types of services the individual receives.Upon admission into a treatment setting, a faceto-face multi-dimensional assessment must beconducted by a qualified credentialed counselor(QCC) or intern as defined in DSHS TAC §448.101to determine a course of treatment that ismedically necessary and clinically appropriate.The assessment must be signed off by a QCC.Evaluation, Treatment, or Referralfor Co-Occurring ConditionsCDTFs shall facilitate access to physical health, mentalhealth, and ancillary services if those services are notavailable through the program and are necessaryto meet treatment goals or individual needs.Individuals in residential CDTFs commonly requiremedications unrelated to their SUD treatment for whichcosts are not covered in the reimbursement for SUDor MAT services. These medications, if included in theMedicaid formulary, may be obtained and reimbursedthrough the individual’s Medicaid pharmacy benefit.Individuals in residential CDTFs also commonly requireother services that are benefits of Texas Medicaid, butnot included in the CDTF rate. Claims for these servicescan be submitted by the appropriate Providers.CDTFs should screen each individual for risk forcontracting tuberculosis, Hepatitis B and C, HIVantibody, and sexually transmitted infections, andif appropriate, provide access to testing and followup. Testing may be performed on site and billed bythe ordering Provider if appropriate testing facilitiesare available that are compliant with the rules andregulations for the Clinical Laboratory ImprovementAmendments (CLIA). Providers that do not complywith CLIA are not reimbursed for laboratory services.Withdrawal Management ServicesWithdrawal management, formerly known asdetoxification, is the medical and behavioraltreatment of individuals experiencing or potentiallyexperiencing withdrawal symptoms as a resultof ceasing or reducing substance use.Withdrawal management involving opioids, alcohol,sedatives, hypnotics, or anxiolytics will vary dependingon the severity of the withdrawal symptoms experiencedbut will typically involve medications to treat symptomsin addition to supportive care, observation, andmonitoring. Withdrawal management involvingstimulants, inhalants, and cannabis typically involvessupportive care, observation and monitoring, andmedications to treat withdrawal symptoms as required.Withdrawal management may be performed in anoutpatient setting for individuals experiencing mild tomoderate withdrawal symptoms that can be successfully,as well as safely, managed outside of a residential settingor an inpatient hospital. Withdrawal management in aresidential setting may be required for individuals whosemultidimensional assessment indicates one or more ofthe following circumstances that would make outpatientwithdrawal management unsafe and/or unsuccessful: A level of severity of withdrawal, medical,and/or mental health complication Sufficient challenges with readiness to change,ability to stop using, and/or social supportWithdrawal management in an inpatient hospital settingmay be required for individuals whose severity of medicalwithdrawal (e.g., impending delirium tremens, severewithdrawal seizures), comorbid medical conditions(e.g., severe liver impairment, acute pneumonia,endocarditis, dementia), and/or comorbid psychiatricconditions (e.g., severe suicidality, acute and unstablepsychosis or mania) requires a hospital level of care.Individual and Group SUD Counselingin an Outpatient SettingCounseling for substance use disorders is designed toassist individuals in developing a better understandingof their SUD, help to establish treatment goals and plansfor achieving those goals, and provide interventionsto assist individuals in accordance with the plan. Theoverall intent of the service is to assist individuals inunderstanding their SUD and developing the skillsand supports needed to address their SUD over time.Counseling may be done individually or in a group settingwith multiple members. Group counseling sessionsare limited to a total of 16 individuals per session.CommunityHealthChoice.org
HHSC NOTIFICATIONS 13 Table of ContentsOutpatient counseling services are appropriate for thefollowing:Residential SUD treatment services may only be providedby a licensed CDTF. Individuals with less severe disordersMedication Assisted Treatment Individuals who are in the early stages of change As a step down from more intensive services Individuals who are stable but for whomongoing monitoring is appropriateNote: For individuals unable or unwilling to accessSUD treatment services at a CDTF, psychotherapydelivered by a licensed practitioner of the healingarts (LPHA) may be an alternative treatmentoption to address an individual’s SUD.Outpatient services may be appropriate at thestart of treatment, throughout treatment, or afteran episode of residential or inpatient treatment,depending on individual acuity, severity, comorbidity,needs, or preferences. Outpatient services canaddress active symptoms as well as provide ongoingtreatment for individuals in partial or full remissionwho need continuing help to maintain progress.Abstinence should not necessarily be a requirementfor participation in outpatient services.Residential Treatment ServicesResidential treatment programs provide a structuredtherapeutic environment where individuals reside withstaff support and deliver comprehensive substanceuse disorder treatment with attention to co-occurringconditions as appropriate. The frequency and durationof services should be based on meeting the individual’sneeds and achieving the individual’s treatment goals.Residential services are appropriate for individualswho require a structured therapeutic environment tostabilize SUD and develop coping and recovery skills.Residential treatment programs may specialize in theunique needs of a specific population such as adolescentsor pregnant or parenting women with children.Episodes of residential treatment may be requiredfor individuals with more severe SUD, moresignific
Continuing Education (CE) Hours TMHP Online Provider Education : Vendor Drug Program Continuing Education for Prescribing Providers : CommunityHealthChoice.org : Claims billed with the delivery codes 59409, . TDI : Provider Services : Provider.CommunityHealthChoice.org 713.295.2295 : Send claims to: