Transcription
2-01229-4CURRENT PERSPECTIVESDeep Brain Stimulation for Addictive Disorders—Where Are We Now?Jason Yuen1,2 · Abbas Z. Kouzani3 · Michael Berk2 · Susannah J. Tye4,5,6,7 · Aaron E. Rusheen1 · Charles D. Blaha1 ·Kevin E. Bennet1,8 · Kendall H. Lee1,9 · Hojin Shin1 · Jee Hyun Kim2 · Yoonbae Oh1,9Accepted: 18 March 2022 The Author(s) 2022AbstractIn the face of a global epidemic of drug addiction, neglecting to develop new effective therapies will perpetuate the staggering human and economic costs of substance use. This review aims to summarize and evaluate the preclinical and clinicalstudies of deep brain stimulation (DBS) as a novel therapy for refractory addiction, in hopes to engage and inform futureresearch in this promising novel treatment avenue. An electronic database search (MEDLINE, EMBASE, Cochrane library)was performed using keywords and predefined inclusion criteria between 1974 and 6/18/2021 (registered on Open ScienceRegistry). Selected articles were reviewed in full text and key details were summarized and analyzed to understand DBS’therapeutic potential and possible mechanisms of action. The search yielded 25 animal and 22 human studies. Animal studies showed that DBS of targets such as nucleus accumbens (NAc), insula, and subthalamic nucleus reduces drug use andseeking. All human studies were case series/reports (level 4/5 evidence), mostly targeting the NAc with generally positiveoutcomes. From the limited evidence in the literature, DBS, particularly of the NAc, appears to be a reasonable last resortoption for refractory addictive disorders. We propose that future research in objective electrophysiological (e.g., local fieldpotentials) and neurochemical (e.g., extracellular dopamine levels) biomarkers would assist monitoring the progress of treatment and developing a closed-loop DBS system. Preclinical literature also highlighted the prefrontal cortex as a promisingDBS target, which should be explored in human research.Keywords Deep brain stimulation · Addiction · Biomarkers · Animal models · Neuromodulation · NeuropsychiatryIntroductionAddictive substances pose significant socioeconomicimpact on society and the healthcare system, costinghundreds of billion dollars annually in the USA alone [1,2]. Psychological and adjunctive pharmacological treatments are the current mainstay for addiction therapeutics.However, the risk of relapse remains high, with some citing relapse rates as high as 75 to 98% within 1 year oftreatment [3]. Investigations into new treatment modalities are urgently warranted. To develop novel therapiesfor addiction, researchers are focusing on the behavioraland neuroscience aspects in the biopsychosocial model(Fig. 1). Deep brain stimulation (DBS) in particular is* Jee Hyun Kimdrjeehyunkim@gmail.com4Queensland Brain Institute, The University of Queensland,St Lucia, QLD 4072, Australia* Yoonbae Ohoh.yoonbae@mayo.edu5Department of Psychiatry & Psychology, Mayo Clinic,Rochester, MN 55905, USA6Department of Psychiatry, University of Minnesota,Minneapolis, MN 55455, USA7Department of Psychiatry, Emory University, Atlanta,GA 30322, USA8Division of Engineering, Mayo Clinic, Rochester, MN 55905,USA9Department of Biomedical Engineering, Mayo Clinic,Rochester, MN 55905, USA1Department of Neurologic Surgery, Mayo Clinic, Rochester,MN 55905, USA2Deakin University, IMPACT, The Institute for Mentaland Physical Health and Clinical Translation, Schoolof Medicine, Geelong VIC 3216, Australia3School of Engineering, Deakin University,Geelong VIC 3216, Australia13Vol.:(0123456789)
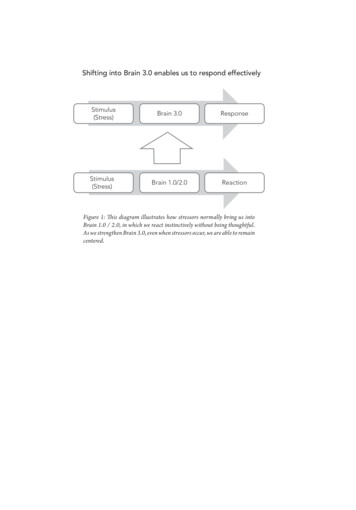
J. Yuen et al.Fig. 1 Biopsychosocial model depicting the different dimensionsin consideration of addiction treatment. The stages of the addictioncycle of behavior are shown (inset) [140]. Interactions between components in different domains lead to addictive behaviors. Created withBiorender.coma neuroscience-based potential treatment for medicallyrefractory addictive disorders, given its diminishing surgical risks. “Medically refractory” cases have no formaldefinition, although these are generally regarded when conventional treatments repeatedly fail [4].Recent advances in neuromodulation techniques anddevices led the indication of DBS to include movementdisorders, such as Parkinson’s disease, to neuropsychiatric conditions, such as depression, Tourette’s syndrome,and obsessive–compulsive disorder (OCD) [5–8]. The useof DBS to reduce substance use has also been exploredin both preclinical and clinical settings [9–12], offering abeacon of hope to patients suffering from medically refractory addictive disorders. This review aims to summarizeand evaluate the potential therapeutic efficacy, mechanismsof action, and biomarkers involved in the use of DBS inthe treatment of addictive disorders. We cautiously reportthat DBS is promising to treat certain refractory addictivedisorders. Recommendations for the future directions arealso provided.Addiction Neurobiology: a Brief OverviewAddiction is a highly complex process involving multipleneurochemicals and brain structures. A highly simplifiedmodel highlights the central role of dopamine in mediating drug reward learning and drug seeking (compulsive)behaviors (Fig. 2). In essence, addictive drugs, such as thepsychostimulants and opioids, enhance synaptic concentrations of dopamine in forebrain subcortical structures, suchas the nucleus accumbens (NAc) [13]. These drugs of abusesignificantly enhance dopamine concentrations over andabove the ability of natural rewards, hijacking the system13Fig. 2 A simplified illustration of the neurotransmitters and neuroanatomical structures involved in the pathophysiology of addiction[13, 19, 20]. Other relevant areas are omitted for clarity. The effect ofdopamine receptors D1-R and D2-R is shown in inset. D1-R mediatesthe direct pathway (positive reinforcement) and D 2-R mediates theindirect pathway (negative reinforcement). Italic descriptions denotechanges secondary to chronic drug use. 5-HT, serotonin; onic acid receptor;D1/2R, dopamine 1/2 receptors; DA, dopamine; GABA, gammaaminobutyric acid; NAc, nucleus accumbens; NMDAR, N-methyld-aspartate receptor; VTA, ventral tegmental area. Created withBiorender.comand encoding a more biologically salient reward associationwith surrounding environmental cues [13]. Such Pavloviandrug-environmental conditioning can trigger the desire toseek more of the drug. For example, the drug associated cuescan elicit a surge of dopamine, which may manifest in drugcraving, seeking and ultimately use [14].Serotonin (5-HT) is another important neurotransmittermediating neuroplasticity, hedonic tone, motivational, andreinforcement processes, as well as cognitive functions [15,16]. 5-HT2A and 5-HT2C receptors in the prefrontal cortex(PFC), NAc, and ventral tegmental area in particular appearto be critical. 5-HT2A receptor increases, and 5-HT2C receptor decreases, striatal dopamine release [15]. The serotonergic neuroadaptations may be accountable for emotionalcomponents such as anhedonia and depression during drugwithdrawal [16]. Recent evidence in mice also suggest thatserotonin signaling via 5-HT1B receptor may attenuate transition from casual to compulsive cocaine use [17].Chronic drug use ultimately alters the homeostatic neuroplasticity in the brain which not only results in a sensitizeddopaminergic system [18], but also leads to changes in theglutamatergic system [13, 19, 20]. For example, calciumpermeable ionotropic glutamatergic AMPA receptors becomeupregulated relative to glutamatergic NMDA receptors [13,19, 20]. The changes in AMPA and NMDA receptors have
Deep Brain Stimulation for Addictive Disorders—Where Are We Now? become a hallmark process of neuroplasticity that underpinsbehavioral changes following chronic drug use [21]. Anotherneurobiological adaptation that occurs with chronic drug use isthe process of “dorsalization” [22]. Here, repeated exposure todrugs of abuse leads to recruitment of the circuit that projectsfrom the orbitofrontal cortex (OFC) to the dorsal striatum (caudate and putamen), where synaptic potentiation occurs at bothdopamine receptors 1 and 2 (D1-R and D 2-R) on GABAergicmedium spiny neurons (MSNs).Activation of D 1-Rs receptors causes excitation in the postsynaptic cell via cyclic adenosine monophosphate production(cAMP) production [23] that ultimately leads to promotionof long-term potentiation [24]. D1-R- and NMDA receptor–dependent activation of extracellular signal-regulatedkinase (ERK) in brain areas such as striatum is an importantpathway for drug-induced locomotor response and sensitization [25–28]. For example, systemic injection of D1-R- orNMDA antagonist prevents ERK phosphorylation triggeredby d-amphetamine in the mouse striatum [29]. In addition,cocaine-induced ERK phosphorylation and locomotor sensitization is prevented with mitogen-activated protein kinases/ERK kinase inhibitor or in mutant mice with alanine-replacedThr-34 residue of dopamine- and cAMP-regulated phosphoprotein (DARPP-32) [29]. D1-R MSN structural plasticitydepends on NMDA and DARPP-32 signaling [24]. Psychostimulants appear to affect ERK signaling via DARPP-32based D1-R- and NMDA intracellular pathways [29].Importantly, D1-R activation inhibits long-term depression, as revealed by D1-R antagonist unmasking long-termdepression [30]. In contrast, D 2-Rs can promote long-termdepression and prevent the induction of long-term potentiation [30]. However, D2-Rs are particularly sensitive todips in the tonic dopamine level, during which they activateprotein kinase A (PKA) to induce long-term potentiation[30–32]. Taken together, D 1-R and D 2-R are critical for bidirectional plasticity of striatal MSNs when dopamine levelsare high vs low to guide adaptive and maladaptive behaviors involved in reward learning [31, 32]. Therefore, D1-Rand D2-R signaling dynamically modulates cortico-striatalplasticity depending on the level of synaptic dopamine tofacilitate transition into persistent drug seeking and use.While DBS appears to target these processes involved inaddiction to reduce drug seeking and taking [10, 33–37],the potential therapeutic efficacy and mechanisms of actionof DBS in the treatment of addictive disorders are poorlyunderstood. We address this gap in the present review.MethodsA search was performed using keywords, such as “deep brainstimulation” and “addiction” in MEDLINE, EMBASE, andCochrane Library database between 1974 and 6/18/2021.Details of search criteria and inclusion and exclusion criteriaare given in Supplementary Information Appendix A. Searchresults are presented in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart(Fig. 3). This review was registered at the Open ScienceFramework [38]. The process yielded 47 papers (25 preclinical studies and 22 human studies), which were furtherreviewed in full text. The results of this literature search aresummarized in the sections below.Results and DiscussionPreclinical Models and Clinical CorrelationAnimal DBS studies in the selected literature (Table 1)predominantly used conditioned place preference (CPP) orself-administration paradigms (Fig. 4) to model addiction.Self-administration models have high construct, content, andface validity relative to human addictive behaviors. Experimenter-administration models such as CPP can measuredrug-induced behavioral sensitization, such as increasedlocomotion, and are easier to perform. Both models alsoallow modeling of withdrawal symptoms during abstinenceand/or extinction phase, followed by relapse behaviors, suchas cue or drug-induced reinstatement. Most common DBSbrain targets in the selected animal studies (Table 1) were theNAc [33, 39–45], PFC [44, 46, 47], and subthalamic nucleus(STN) [10, 37]. The following sections will focus on thesethree most studied targets.NAc Electrical StimulationThe NAc is divided into core and shell subregions with different histopathological compositions, projections, and functions [48]. Studies suggest that the shell is responsible forreinforcing properties of novelty, rewards (both drug- andnon-drug-related), and drug relapse, whereas the core mediates spatial learning, conditioned responses, responses tomotivational stimuli, and impulsive choices [14, 49]. Thesefeatures of motivated behaviors suggest NAc shell underlying extinction and reinstatement behavior [50], and NAccore underlying the initial acquisition of drug taking andcue-elicited drug seeking [48]. However, there is synergybetween the two subnuclei, and both play a role in drugaddiction.Stimulation of either the core or shell subregions of theNAc using a range of low and high frequencies leads toreduced drug taking, seeking, or CPP in rats conditionedwith alcohol [34, 51, 52], nicotine [53], opioids [9, 37, 39,41, 46, 54–57], cocaine [10, 33, 35, 40, 42, 43, 47, 58, 59],or methamphetamine [45] (Table 1). Behavioral improvement was related to the timing of when electrical stimulation13
J. Yuen et al.Fig. 3 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of literature search. Other sources includethose found by reviewing the references from included paperswas given—that is, stimulation given before a self-administration session or CPP acquisition would reduce drug intakeor prevent CPP, respectively [39, 45]. When given duringabstinence or reinstatement, stimulation would diminishdrug or cue-induced drug seeking after extinction and/orforced abstinence phase [40–43, 45]. Such efficacy of stimulation during abstinence to prevent relapse is particularlypromising in the clinical context.While most animal and human studies (Table 2) showsuccess in modulating addictive behavior using NAc stimulation, there are two main issues. First, there is conflicting13evidence in animal studies regarding the efficacy of NAccore vs shell stimulation. Both high- and low-frequencystimulation (HFS, LFS) of NAc (electrodes placed acrosscore and shell) can reduce cocaine-primed drug seeking following 24 days of abstinence [43]. Other studies using coreas the DBS target showed reduced morphine-induced CPP[39], ethanol self-administration [51], and heroin reinstatement [41]. The shell was also shown to be an effective target for morphine-induced CPP [55], cocaine reinstatement[40], ethanol self-administration [44, 51, 52], and methamphetamine reinstatement [45]. In contrast, Vassoler et al.
Subcutaneous morphine72 mg pellet (for 72 h)vs placeboLong-Evans male PAG; midlinerats (N 29)targetBeaulieu andThorn (1986)[54]NA50Sprague–Dawley NAc core; rightrats of unspecifiedsex (N 32)Liu et al. (2008)[39]Sprague–Dawleymale rats(N 7–12/group)Long-Evans male NAc shell or NAccore (2 groups);rats (N 4–5/bilateralgroup)Vassoler et al.(2008) [40]Knapp et al.(2009) [51]NAc shell ordorsal striatum;bilateralSprague–Dawleymale rats(N 7–14/group)Levy et al.(2007) [35]130CPP induced by i.p.morphine10–60 mg/kg (increasingdose)160Cocaine selfadministrationFR1 (250 μg/kg perinfusion) progressingto FR5Alcohol (0–10% ethanol) 160self-administration200–500μA150 μA0–150 μA60 μs200 μs200–400μA20–200μA210 μs100 μsNA60400 μAPulse width CurrentHzStimulation parameters20, 100Cocaine (1 mg/kgLateralreducing to 0.5 mg/kg)hypothalamusself-administration.(100 Hz) or PFC(20 Hz, 100 Hz); Progressive ratiowas also assessed atbilateral0.5 mg/kgLocomotion followingcocaine challenge15 mg/kg (i.p.)Alcohol (1000–2018 mg/kg ethanol)via experimenterintubationBlack-hooded male Amygdaloidrats (N 27)complex;unilateral (sideunspecified)Pinel et al.(1975) [85]Behavioral paradigmSpecies and strain Target; laterality(sample size)Author and year5 minContinuousduring 2-hreinstatementsessionsAt 150 μA, but not at 100 μA or less, DBS inshell or core given prior to established alcoholself-administration sessions reduced alcoholconsumptionDBS in NAc immediately following 10 or 20 mg/kg cocaine prime attenuated cocaine-inducedreinstatement compared to sham DBS. DBS indorsal striatum had no effects on reinstatementStimulation was performed to induce kindling45 stimulations(until displaying at least 1 seizure), and alcohol(1 s duration),was administered after stimulation. The3 /day, 5 days/withdrawal syndrome observed 9 h followingweekalcohol administration in kindled (stimulated)animals was much more severe than that of thecontrolsLarge range of current applied to different rats30 min after(depending on analgesia threshold)naloxoneStim. attenuated morphine withdrawal behaviors,precipitatedesp. the recessive behaviors associated withwithdrawalautonomic changes (e.g., eye-twitching) lasting2 h or more30 min/day forDBS (100 Hz) in lateral hypothalamus or PFC10 daysreduced cocaine-, but not sucrose seeking. DBS(100 Hz) in the PFC also reduced cocaine takingin a progressive ratio self-administration testCocaine-induced locomotor hyperactivity wasexaggerated by lateral hypothalamus DBS butwas reduced by PFC DSBThe behavioral findings were accompanied byGluR1 alterations in the NAc (increased) and theVTA (variable depending on subregion)3 h (15-min trains Pre-conditioning DBS sessions preventedmorphine-induced CPP compared to shamwith 45-minintervals)DBS sessionMain outcomesTable 1 Summary of animal studies in deep brain stimulation and addiction, listed in chronological order. ACC , anterior cingulate cortex; BLA, basolateral amygdala; CPP, conditioned placepreference; EA, experimenter-administration; EtOH, alcohol (ethanol); FR, fixed ratio; GABA, γ–aminobutyric acid; HFS, high-frequency stimulation; i.p., intraperitoneal injection; LFS, lowfrequency stimulation; LH, lateral hypothalamus; (m)PFC, (medial) prefrontal cortex; NAc, nucleus accumbens; OD, once daily; OFT, open field test; PAG, peri-aqueductal gray; pCREB, phosphorylated cyclic AMP-response element binding protein; SA, self-administration; s.c., subcutaneous injection; STN, subthalamic nucleus; vHipp, ventral hippocampus; VTA, ventral tegmentalarea; NA, data not availableDeep Brain Stimulation for Addictive Disorders—Where Are We Now? 13
13Long-Evans male STN; bilateralrats (N 88)Rouaud et al.(2010) [59]Guo et al. (2013) Sprague–Dawley NAc core; mixed[41]male rats (N 54) unilateral orbilateralHome cage alcohol(10% ethanol) selfadministrationAlcohol-preferring NAc shell;male rats (N 20) bilateralHenderson et al.(2010) [52]0, 75, or150 μA100 μs200 μA140–150 60 μs50–130μA200 μA500 μs10–10060 μsPulse width CurrentHzStimulation parameters130Cocaine selfadministrationFR 1 (0.25 mg perinfusion)Progressive ratio wasalso assessed at0.25 mg per infusionCPP induced by cocaine(10 mg/kg i.p.)130Heroin selfadministrationFR1 (50 μg/kg perinfusion) paired with alight cueCocaine selfadministration0.25, 0.5, and 1 mg/kgi.v. for 21 daysReinstatement: 0, 5, 10,20 mg/kg i.pSprague–Dawley Lateral habenula;male rats (N NA) rightFriedman et al.(2010) [58]Behavioral paradigmSpecies and strain Target; laterality(sample size)Author and yearTable 1 (continued)1-h continuousstimulationDBS was appliedthroughouteach behavioralsession1 h on 1 h offDBS stage 2:24 h when freeaccess wasallowed againFor 15 min atstart of taskDBS sessionDaily DBS (75 and 150 μA) sessions duringabstinence reduced subsequent cue- and heroininduced drug seeking, except for DBS only in theleft NAc. DBS increased pCREB but decreasedΔFosB in NAc core and shellDBS did not affect locomotion, nor spatial learningand memoryLFS alone appeared to have superior effect onseeking behavior compared to HFSWith DBS consisting of a combination between 10and 100 Hz, drug seeking behavior was reducedin self-administration, extinction and relapsephasesLesioning actually increases drug seeking behavior(increased number of presses during extinction)Tests controlled by forced swim test (depressionlike behavior), open-field test (locomotion), etcWestern blot showed elevated glutamatergicreceptor subunits NR1 and GluR1 andscaffoldingProtein PSD95, but not GABA Ab, protein levelsin VTA with cocaine SA but normalized afterDBSDBS reduced cocaine seeking behavior duringboth self-administration and extinction training,as well as lever-pressing behavior duringreinstatementDBS given prior to established alcohol selfadministration sessions reduced alcoholconsumption and preference over water. DBSgiven prior to alcohol-induced relapse following4–6 weeks of abstinence also reduced alcoholconsumption and preference over waterDBS decreased cocaine but not food takingProgressive ratio tests showed that DBS decreasesmotivation to attain cocaine but increasedmotivation to attain food. Similar dissociationwas observed with CPP, with DBS reducingcocaine CPP but increasing food CPPMain outcomesJ. Yuen et al.
Morphine EA5 mg/kg i.p.progressing to90 mg/kg i.p. over12 daysReinstatement—2.5 mg/kg i.pBehavioral paradigmSprague–Dawleymale rats(N 5–12/group)Alcohol-preferring NAc shell;female rats (N 7) unilateralNAc shell;bilateralSprague–Dawleymale rats(N 6–12/group)C57BL/6transgenic malemice (N 6–12/group)Long-Evans male NAc; righthemisphererats (N 6–8/group)Pushparaj et al.(2013) [53]Vassoler et al.(2013) [42]Wilden et al.(2014) [34]Creed et al.(2015) [33]Hamilton et al.(2015) [43]Cocaine selfadministrationFR1 (500 μg/kg perinfusion) progressingto FR3Locomotor sensitizationinduced by cocaine20 mg/kg i.pAlcohol (15% ethanol)self-administrationNicotine SA0.03 mg/kg i.v.per infusion under aFR-5 thenprogressive ratioscheduleReinstatement dosewas 0.15 mg/kg s.cNAc shell or core; Cocaine selfbilateraladministrationFR1 (250 μg/kg perinfusion) progressingto FR5Sprague–Dawley NAc shell;male rats (N 25) bilateralMa et al. (2013)[55]Insular cortex;bilateralSpecies and strain Target; laterality(sample size)Author and yearTable 1 (continued)90 μs100 μs12 or13020 or16060 μs160100 μs90 μs13015060 μs13050–200μA50 μAMain outcomesContinuousduring 2-hreinstatementsessions30 min60 minDBS of NAc shell, but not core, immediatelyfollowing 10 mg/kg cocaine prime attenuatedcocaine-induced reinstatement compared to shamDBS (0 μA)DBS of NAc shell induced c-Fos expressionlocally and in the infralimbic cortexDBS (200 μA but not 100 μA) starting 5 min priorto and throughout established daily alcohol selfadministration sessions reduced alcohol taking.Alcohol taking resumed at baseline levels postDBS sessionsDBS at 130 Hz, but not at 12 Hz, givenimmediately before test transiently suppresseslocomotor sensitization. DBS had no behavioraleffects when applied 4 or 24 h before testDBS at 130 Hz 24 h before did not affect cocaineevoked plasticityDBS at 12 Hz in combination with a D 1-Rantagonist reversed cocaine-inducedhyperlocomotion and plasticity. DBS at 12 Hzhad no effects by itselfA single DBS session did not affect cocaine taking.Daily DBS 20 or 160 Hz sessions during 14 daysof abstinence led to attenuated cocaine seekingfollowing a 5 mg/kg cocaine prime when tested1 day, but not 14 days, after the last DBS sessionCPP training was first given with increasing dosesof morphine; naloxone then given to precipitate“withdrawal.”DBS prevented drug seeking behavior (in terms of CPPmeasurements) during re-instatement of morphinePlace navigation studies were performed (Morriswater maze) to assess learning and memory—nochange by DBSDBS significantly attenuated nicotine taking, underHFS started fromboth FR5 and progressive ratio schedules, as well5 min beforeas nicotine seeking behavior induced by cues andbehavioralpriming; no effect on food taking behaviorsessions andlasted throughout HFS of brain slices containing the insular regionwas found to inactivate insular neuronsthe sessions60 min, 5 /dayfor 30 daysDBS session100 or 200 65 minμA150 μA50 μA2 V (stim.voltages)Pulse width CurrentHzStimulation parametersDeep Brain Stimulation for Addictive Disorders—Where Are We Now? 13
13Wistar male rats(N 18)Wistar male rats(N 32)Batra et al.(2017) [45]Wade et al.(2017) [37]STN; bilateralNAc shell;bilateralNAc shell,infralimbiccortex, era Sprague–Dawley Ventral capsule/male rats (N 87) ventral striatumet al. (2016)(VS); bilateral[56]Wistar male rats(N 6–15/group)Hadar et al.(2016) [44]90 μs100 μs60 μs60 μs13020 or130130130Home cage alcohol (5,10, or 20% ethanol)and water twobottle choice selfadministrationMorphine EA5 mg/kg s.c./day for4 days with CPPtrainingHeroin SA60 μg/kg i.vFR13- or 12-h sessions5 days per weekMethamphetamine selfadministrationFR1 (0.05 mg/kg perinfusion)DBS sessionMain outcomes25,50,100, or150 μA20 min (duration Methodology was unclear (e.g., interval betweenof 1 s every 5 s)doses and shock). Short-term stimulation wasgivenDBS at 50 and 100 μA stimulation reversedpassive avoidance memory attenuation bymorphine. DBS at 25 and 150 μA had no effects24 h or 4 daysCompared to sham DBS, 4 days of NAc shell5.25 VDBS led to augmented alcohol-induced relapse(stim.following chronic abstinence. Acute (24 h)voltages)DBS reduced alcohol-induced relapse. DBS ininfralimbic cortex or striatum had no effects onbehavior. Acute NAc DBS (24 h) increased localdopamine levels in alcohol-exposed rats100–20060 min/dayHFS of dorsal VS impaired extinction trainingμAover 9 days ofand extinction memory but no effect for HFS ofextinctionventral VSLFS of dorsal VS strengthened extinction memorywhen tested 2 or 9 days after the cessation ofstimulationBoth HFS and LFS increased c-Fos expression ininfralimbic PFC, but only LFS increased c-Fos inthe basal amygdala and the medial portion of thecentral amygdala200 μA3hThe first two daily sessions of DBS priorto self-administration sessions reducedmethamphetamine taking compared to shamDBS, while the remaining 3 DBS sessions hadno effects. These DBS sessions reduced cueinduced reinstatement when tested 20–28 dayslater50–130Throughout theSTN HFS attenuated re-escalation of heroin intakeμASA sessionspost-abstinence in rats with extended access toheroinSTN HFS inhibited substantia nigra,entopeduncular nucleus, and NAc shell(measured with brain mapping analyses ofimmediate-early gene expression) but not PFC,and silenced STN neurons (measured usingrecording ex vivo)Pulse width CurrentNAHzStimulation parameters60Behavioral paradigmPrelimbic cortex; Light–dark shockright hemisphere passive avoidancereversed by morphine(10, 20, or 40 mg/kg) i.pSpecies and strain Target; laterality(sample size)Mehdipour et al. Wistar male rats(2015) [46](N 6 in eachgroup)Author and yearTable 1 (continued)J. Yuen et al.
Degoulet et al.(2021) [10]Male ListerHooded rats(N 84)STN; bilateralCocaine SAFR1 progressing torandom interval until120 sPunishment sessions(foot shock) alsoapplied (rats dividedinto shock-resistantand shock-sensitivesubgroups)Sprague–Dawley Infralimbic cortex, Cocaine selfadministrationmale rats (N 6–8/ prelimbiccortex, anterior FR1 (250 μg/kg pergroup)infusion) progressingcingulate cortex,to FR5BLA or vHipp;bilateralGuercio et al.(2020) [47]150 μA50–150μA8, 30, or 80 μs130150 μA60 μs160100 μsOrbitofrontalcortex; bilateralWistar male rats(N 108)Fakhrieh-Aslet al. (2020)[9]13 orCPP induced by130subcutaneousinjections of morphine3–7 mg/kg (increasingdose)Anterior insularcortex; bilateral150 μAPulse width Current90 μsHzStimulation parameters130CPP induced bysubcutaneous injectionof morphine (10 mg/kg)Behavioral paradigmSprague–Dawleymale rats(N 9–15/group)Species and strain Target; laterality(sample size)Chang et al.(2020) [57]Author and yearTable 1 (continued)DBS turned onand intensitywas increasedto reachpredeterminedparametersprior to startof behavioralsession, andcontinuedduring sessionContinuousduring 2 hreinstatementsessions20 or 40 min,once daily11 or 14 daysduringextinction orabstinenceDBS session14 days of DBS during abstinence attenuated theexpression of morphine-CPP but CPP relapsed10 days after the cessation of DBS. Elevendays of DBS during CPP extinction facilitatedextinction acquisition as well as alleviatingmorphine-induced reinstatementOFT and novel object recognition test showedno impairment to locomotion and recognitionmemoryProteomic analysis revealed the expression levelsof 8 morphine-regulated proteins in the anteriorinsula were reversely changed by HF-DBSHFS but not LFS given daily for 3 days ofconditioning significantly prevented CPPacquisitionHFS but not LFS given daily for 6–10 days ofextinction facilitated extinction acquisition andblocked morphine-induced reinstatementDBS did not cause any changes in locomotoractivity, novel objection recognition memory, noranxiety-like behaviorDBS at BLA, vHipp, and infralimbic corteximmediately following 10 mg/kg cocaine primeattenuated cocaine-induced reinstatementcompared to sham DBS (0 μA), but BLA andvHipp also attenuated sucrose reinstatementAnterior cingulate cortex and prelimbic cortexDBS did not attenuate either30 Hz but not 130 Hz DBS reduced pathologicalcocaine seeking during treatment, whereas130 Hz actually increased seeking behavioracutelyCompulsive, i.e., shock-resistant ratsexhibit pathological STN low-frequencyoscillations (LFP) during cocaine escalation(especially 20 Hz)Main outcomesDeep Brain Stimulation for Addictive Disorders—Where Are We Now? 13
J. Yuen et al.demonstrated that stimulation of the NAc shell but not thecore attenuated cocaine-induced reinstatement [42].The contradicting evidence above may be explained bythe large activation volume of stimulation pulses, such thatpulses centered on the core may also affect the shell, andvice versa. From human studies, the volume of activationwas estimated to be between 30 and 120 mm3 [60] and thehuman NAc volume is around 700 m m3 [61]. However,for adult Sprague–Dawley rats, the total volume of NAc isapproximately 5 m m3 with the NAc core making up halfof that [62]. Therefore, neighboring structures could beco-stimulated in rats. Notably, the core and shell divide isfunctionally present in humans
refractory addictive disorders, given its diminishing sur-gical risks. "Medically refractory" cases have no formal denition, although these are generally regarded when con-ventional treatments repeatedly fail [4 ]. Recent advances in neuromodulation techniques and devices led the indication of DBS to include movement