Transcription
Strengthening midwiferyleadership: a manifestofor better maternity carePromoting Supporting Influencing
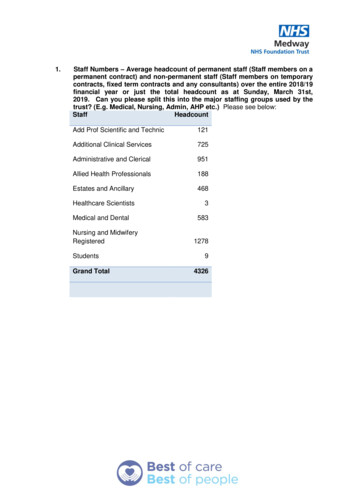
Strengthening midwifery leadership: a manifesto for better maternity careStrengthening midwifery leadership:a manifesto for better maternity careAround three-quarters of a million babies are born in the UK each year, makingchildbirth one of the most common reasons for admission to hospital and ourmaternity services a ‘shop window’ for the NHS.Everyone – NHS staff, politicians, the public and thosewho use the service – all want maternity care to be thebest and safest it can be. Midwives and all maternity staffwork hard to deliver that, and given the importance ofwhat we do the spotlight is rightly on maternity servicescontinually to improve.Despite all of this – the number of women who receivematernity care each year and the cost of gettingmaternity care wrong – the voice of midwifery canstruggle to reach the highest levels of managementwithin trusts and health boards, and within the healthservice more widely.A vital part of delivering that improvement is strong,effective midwifery leadership, focused on getting thebest out of every member of staff.This may be because midwives make up only around two percent of NHS staff, or possibly because maternity care servespredominantly healthy people through a natural life eventthat does not necessarily require medical intervention.“Strong and collective leadership isimportant to the development of apositive work environment” 1“High quality maternity leadership whichsupports innovation is essential” 2Whatever the reason, it is a situation that needs tochange. We need strong midwifery leadership to deliverthe high quality, safe maternity services that all of usstrive to provide. And in this manifesto the Royal Collegeof Midwives sets out seven steps to make that happen.“Effective leadership has a key role indeveloping safe, high quality services” 3The cost to the NHS of getting maternity care wrong canbe severe. Not only in terms of the damage that can bedone to lives, and even the loss of life, but financially too.Clinical negligence claims relating to obstetrics representedonly 10 per cent of the volume of claims received in2018/19 but accounted for half of their total value 4.12342 The Royal College of MidwivesGill WaltonChief ExecutiveRoyal College of MidwivesScottish Government & Grant, J (2017: page 59) The Best Start: a five-year forward plan for maternity and neonatal care in Scotland. Edinburgh: Scottish Government.Available: /National Maternity Review (2016:page 78) Better Births: improving outcomes of maternity services in England. Available: /02/national-maternity-review-report.pdfWelsh Government (2019:page 15) Maternity Care in Wales. A Five Year Vision for the Future (2019-2024). Available: n-for-the-future-2019-2024.pdfNHS Resolution (2019) Annual report and accounts 2018/19. Available: .org.uk 3
Strengthening midwifery leadership: a manifesto for better maternity care1A Director of Midwifery in every trustand health board, and more Heads ofMidwifery across the serviceProfessional input into theappointment of midwife leaders7We need a stronger midwifery leadership voice in every part of the NHS thatdelivers a maternity service.6A commitment to fund ongoingmidwifery leadership development45Strengthening and supportingsustainable midwifery leadershipin education and research3Specialist midwives in everytrust and health board2While it is routine for the most senior practising midwifewithin a trust or health board to be a Head of Midwifery,there are significantly fewer places where that role istaken by a Director of Midwifery. The difference is morethan just a title.Heads of Midwifery will typically focus on the operationaldelivery of maternity care locally. They will often reportinto a director of nursing within a trust or health boardand will not have direct input into or responsibility forstrategic, board-level decision-making.More consultant midwives1A lead midwife at a seniorlevel in all parts of the NHS,both nationally and regionallyA Director of Midwiferyin every trust and healthboard, and more Heads ofMidwifery across the serviceSeven stepsto strengthenmidwiferyleadershipDirectors of Midwifery, on the other hand, are leadersand advocates for safe, high quality maternity care,managing the strategic and operational delivery ofmaternity services locally. They are accountable for thestrategic planning of maternity services and the provisionof midwifery care, the provision of strategic, professionalleadership and advice, and act as both an advocate forwomen and the expert voice of the profession.Where midwifery leaders locally do not have direct accessto the board, but must instead feed into it via a director ofnursing, there is the risk of a damaging disconnect betweenstrategic direction and operational management. A directorof nursing will oversee the provision of nursing care in a widerange of areas, from A&E, cancer care, and geriatric medicine,for example, to radiology, surgery, and urology. Even withthe best will in the world the provision of maternity care willrarely be at the top of a director of nursing’s agenda.Nursing and midwifery are also distinct professions.The overall direction of midwifery care has diverged54 The Royal College of Midwivesfrom nursing, and continues to do so. Midwifery care isundergoing a fundamental shift towards a model of carebased in the community rather than centralised in bighospitals. It is also one of the few NHS services in whichpractitioners can cross the boundaries between primaryand secondary care every day. Given this divergence, thecurrent norm of having a director of nursing responsiblefor midwifery at board level is increasingly outdated.Additionally, there are issues relating to maternity care thatshould be important and strategic enough – the litigationrisk, for example – to require that a senior midwife has atleast the right of access to the board in their own right.Every trust or health board delivering maternity care shouldhave a Director of Midwifery, with a Head of Midwifery inevery maternity unit within the organisation (with exceptionsfor very small units). This would help protect people from therisk posed by dysfunctional maternity services by enablingproblems to be identified and escalated more quickly.It should be the role of the Head of Midwifery locally to leadtheir team and to manage the provision of local services.It would then be for the Director of Midwifery, as a seniormanager, not only to support the work of Heads of Midwiferybut also to contribute strategically to improve how maternityservices link into what is happening across health and socialcare sectors, both locally and more widely.“Front line teams do not operatein a vacuum; leadership is the keydeterminant of the organisational culturein which front line teams operate” 5Ibid (n2: page 72)www.rcm.org.uk 5
Strengthening midwifery leadership: a manifesto for better maternity care23A lead midwife at a senior level inall parts of the NHS, both nationallyand regionallyAs well as the parts of the NHS that deliver maternity services directly to thepublic, there are many other bodies involved in the delivery of healthcare. Theymonitor how well providers are doing, plan the future workforce, regulate staff,amongst many other functions. These bodies need a senior midwifery voice too.Maternity care should be among those services that havea guaranteed strategic voice at the top levels of seniorNHS management. After all, with three-quarters of amillion births taking place in the UK each year, childbirthis amongst the top reasons for admission to hospital, andclaims relating to obstetrics account for around half ofthe amount paid out in clinical negligence claims. It isvital for the NHS to focus on getting maternity care right.All NHS organisations in each part of the UK and at alllevels, from the national to the local, should have a leadmidwife in a senior position within that organisation. Theywould ensure that the strategic advice and the uniqueperspective of midwifery is appropriately articulatedwithin any new policy, standards and guidance.More consultant midwivesConsultant midwives are highly experienced and acknowledged clinical expertsin their field. They lead, support, coach, mentor, inspire and empower theirmidwifery colleagues. They are leaders with both the responsibility and theability to evaluate, develop and improve the provision of maternity services.We need more of them.Becoming a consultant midwife allows a midwife totake on a more senior role within the service whilstcontinuing to focus on the provision of care rather thanmore managerial tasks, such as management of staff. Thisenables them to focus solely on aspects of leadership thatare directly about the frontline of care, such as qualityimprovement, implementation of evidence-based practiceand service innovation.This is already recognised in some parts of the NHS. TheScottish Government employs a Chief Midwifery Advisorand following the publication of the NHS Long Term Plan 6,England now has its own Chief Midwifery Officer.As with midwives as a whole, there are fewer consultantmidwives than there should be. In our 2018 survey ofHeads of Midwifery, 44 per cent of those who respondedstated that they did not have a single consultant midwifein post. Of those who did, they employed the equivalentof less than one full-time consultant midwife (four-fifthsof one, to be exact).But there are notable exceptions, i.e. organisations withan important role to play in functions such as workforceplanning and development, and the inspection, monitoringand regulation of maternity care, that do not have a seniormidwife.More consultant midwives would mean better and safercare for women and their families 7. It would meansomeone of seniority and professional standing who is onthe ground, accessible to colleagues and on the frontlineof delivering care.“Individuals will only be able to makea difference if they are nurtured andsupported by strong leadership atlocal level” 8Given the national imperatives for high quality and safematernity care, there needs to be a focus on successionplanning and growth of the role of the consultantmidwife across all trusts and health boards.We would like to see at least one consultant midwife inevery maternity unit. For those responsible for providingservices in remote and rural areas, one option could beto appoint a consultant midwife across more than onetrust / health board, providing consistency and clarityof professional guidance for this very specific kind ofmidwifery service.We are all ambitious for our maternity services, what theycan achieve and how they can improve. To achieve thoseambitions, like the UK Government’s ambition to makeEngland one of the safest places in the world in which tohave a baby, we need strong clinical leadership visible andaccessible. This is exactly what recruiting more consultantmidwives would deliver.6NHS England (2019) The NHS Long Term Plan. Available /2019/01/nhs-long-term-plan.pdf6 The Royal College of Midwives78Wilson C, Hall L, Chilvers R (2018) Where are the consultant midwives? British Journal of Midwifery Vol 26:4: 254-260.Ibid (n2: page 85)www.rcm.org.uk 7
Strengthening midwifery leadership: a manifesto for better maternity care45Specialist midwives in every trust andhealth boardSpecialist midwives provide expert advice to colleagues and to womenand their families. They act as a resource on issues relating to their area ofspecialism, championing improvements in the trusts / health boards wherethey work. We need to expand this role throughout the NHS.Specialist mental health midwives are one example ofthis role. These midwives are experts who lead work toensure women with perinatal mental illnesses and theirfamilies receive the specialist care and support theyneed during pregnancy and in the postnatal period. Theysupport their maternity team colleagues to ensure thataffected women and families receive the best possiblecare, personalised to them 9.Other examples include specialist midwives who coverbereavement, diabetes, infant feeding and safeguarding.In far too many parts of the country however thesespecialist midwife posts do not exist, meaning womenare going without this specialist care and midwives arenot able to access knowledge and expertise that wouldimprove the quality of care they are able to provide.According to the RCM’s 2018 survey of Heads of Midwifery:It is also often the case that these specialist midwives areonly able to work on these specialisms for part of theirworking week. In that same survey, for example, eventhose Heads of Midwifery who had a maternal mentalhealth specialist midwife, employed an average of fourfifths of one midwife in that role. For smoking cessationspecialist midwives, it was just one-fifth of one midwife.Specialist midwife roles provide direct specialist andexpert care to women who need it and advice andguidance to colleagues. Without them, maternity serviceswould inevitably provide care that is not as good as itcould be.A range of specialist midwife roles should be the normin every trust / health board across the United Kingdom.The mix of specialisms will depend upon the needs of theservice locally. Midwives should have access to and beable to draw upon these midwives’ skills and experience asthey strive to deliver and improve care. two in three (69 per cent) reported not having asmoking cessation specialist midwife two in three (67 per cent) reported not having afemale genital mutilation specialist midwife two in five (41 per cent) reported not having asubstance misuse specialist midwife one in four (27 per cent) reported not having amaternal mental health specialist midwife9Maternal Mental Health Alliance/NSPCC/RCM (2013) Specialist Mental Health Midwives: what they do and why they matter. Available: .pdf8 The Royal College of MidwivesStrengthening and supportingsustainable midwifery leadership ineducation and researchIt is not just the NHS that plays an important role in delivering the midwiferyworkforce we need. Our universities train the next generation of midwives andthey employ the teachers and academic researchers upon whose work we relyto improve maternity care.There is national 10 and international 11 expert consensuson the fundamental importance of midwifery leadershipin education and the role of midwifery educatorsin the provision of high quality midwifery care. It isrecommended that midwifery leadership is positionedin high-level national policy, planning and budgetingprocesses to improve decision making about investmentsfor midwifery education 12.Lead Midwives for Education (LMEs) are experienced,practising midwife teachers who lead on the development,delivery and management of midwifery educationprogrammes 13. They help to ensure high standards inmidwifery education and are a vital intermediary betweenthe professional regulator (the Nursing and MidwiferyCouncil) and the universities.In addition, we need strong professorial midwiferyleadership within universities to promote, protect andsupport a strong and vibrant research community whosework continually improves the evidence upon which thevery best maternity care is based.Universities together with their partner trusts / healthboards must support and develop future midwiferyresearch leaders through clinical academic careerprogrammes, funded PhDs and post doctoral researchposts 14 as well as the creation of midwifery professorshipsin all institutions that provide midwifery education.To succeed in this role LMEs must have the seniority andauthority to exercise strategic influence over all universitybusiness that impacts on the development and delivery ofpre- and post-registration midwifery education.10 NMC/University of Nottingham (2010) The MINT Project. Midwives in Teaching. Evaluation of whether Midwife Teachers bring a unique contribution particularly in the contextof outcomes for women and their families. Available: Midwifery-Reports/MINT-report.pdf.11 ICM Global Standards for Midwifery Education (Amended 2013) Available: /education-files/2018/04/icm-standardsguidelines ammended2013.pdf12 UNPFA/Unicef/WHO/ICM (2019) Strenthening quality midwifery education for Universal Health Coverage 2030. Framework for Action. Available: 24738/9789241515849-eng.pdf?ua 113 ucators/the-role-of-lead-midwives-for-education/14 Council of Deans of Health (2018) Nursing, midwifery and allied health clinical academic research careers in the UK. Available: rg.uk 9
Strengthening midwifery leadership: a manifesto for better maternity care67A commitment to fund ongoingmidwifery leadership developmentProfessional input into the appointmentof midwife leadersOrganisations that offer career progression and personal development inleadership and management are more likely to attract and retain talent 15, andRCM members tell us that they believe leadership and management trainingwill improve their personal performance.Directors and Heads of Midwifery must have the skills, experience andcredibility to lead and manage maternity services. The appointment of the rightindividual is an important matter, and selection procedures within the NHSshould be focused on ensuring that the right people get into the right jobs.Programmes that include developing, mentoring, andcoaching can help workplaces retain existing talent,attract new staff and develop new thinking. Investingin leadership is also linked to higher performance and alearning culture.In this prolonged era of tight budgets it is all too easy fororganisations to cut back on training and development,and this has been the case in the NHS over many years.In our most recent survey, around a third (31 per cent) ofHeads of Midwifery said they have been forced to reduceaccess to training and development, with continuingprofessional development funding down by around half insome units.The NHS should instead be helping people to lead theservice through challenging times. In every corner of theUK, the health service has high ambitions for maternityservices, and in times of change it is critical to have thebest leaders to navigate through the challenges.The growing urgency of the need for leadershipdevelopment is underlined by the age profile of themidwifery profession. In Scotland, for example, in 2018,two in every five midwives were in their fifties or sixties.In Wales, the figure was 36 per cent, over one in three.Not every senior midwife will be in an older age category,and not every older midwife will be in a leadershipposition, but inevitably there will be a correlationbetween the two. Such large proportions of the midwiferyworkforce in these older age bands helps to emphasise theneed to act on midwifery leadership now, to prepare forthe future.We want to see NHS organisations across the UK commit toclear and funded plans to develop midwife leadership skills.We are seeing some good work. Health Education England,for example, is working with the NHS Leadership Academyto develop a leadership training offer to Local MaternitySystems (where commissioners and providers of maternityservices come together at the local level). They recognisethat the evidence demonstrates that “collaborative,compassionate and inclusive leadership” is most effectivein improving care and delivering better care outcomes 16.The best leaders need more than just skills and experience,as important as these attributes are. The best candidatesalso carry professional credibility and the confidence oftheir midwifery colleagues.We are hopefully seeing signs of this starting toemerge, for example with the involvement of an RCMrepresentative on the selection panel for the new post ofChief Midwifery Officer in England.This is as true for doctors as it is for midwives, which iswhy for senior medical appointments the medical royalcolleges are involved in the selection procedure. It wouldbe a small but important step to extend this conventionto midwifery, to include a senior RCM representative.Similar arrangements should be made for LMEs.We need to see more of this.The seven steps to strengthen midwifery leadership1A Director of Midwifery in every trust and health board, and more Heads of Midwiferyacross the service2A lead midwife at a senior level in all parts of the NHS, both nationally and regionally3More consultant midwives4Specialist midwives in every trust and health board5Strengthening and supporting sustainable midwifery leadership in education and research6A commitment to fund ongoing midwifery leadership development7Professional input into the appointment of midwife leaders15 NHS Improvement (2016) Developing People – Improving Care: a national framework for action on improvement and leadership development in NHS-funded services. /Developing People-Improving Care-010216.pdf16 Ministerial answer, dated 29th January 2019, from Baroness Manzoor to written parliamentary question [HL12864] from Baroness Tonge. Available: n/Lords/2019-01-15/HL12864/10 The Royal College of Midwiveswww.rcm.org.uk 11
Published August 2019The Royal College of Midwives15 Mansfield StreetLondonW1G 9NH0300 303 0444info@rcm.org.ukwww.rcm.org.ukPromoting Supporting Influencing
rarely be at the top of a director of nursing's agenda. Nursing and midwifery are also distinct professions. The overall direction of midwifery care has diverged from nursing, and continues to do so. Midwifery care is undergoing a fundamental shift towards a model of care based in the community rather than centralised in big hospitals.