Transcription
Original researchCaroline SE Homer ,1 Sabera Turkmani,1,2 Alyce N Wilson,1 Joshua P Vogel,1Mehr Gul Shah,3 Helga Fogstad,3 Etienne V Langlois 3To cite: Homer CSE, Turkmani S,Wilson AN, et al. Enhancingquality midwifery care inhumanitarian and fragilesettings: a systematic review ofinterventions, support systemsand enabling environments.BMJ Global Health2022;7:e006872. doi:10.1136/bmjgh-2021-006872ABSTRACTIntroduction Women and children bear a substantialburden of the impact of conflict and instability. The numberof people living in humanitarian and fragile settings (HFS)has increased significantly over the last decade. Theprovision of essential maternal and newborn healthcareby midwives is crucial everywhere, especially in HFS.There is limited knowledge about the interventions,support systems and enabling environments that enhancemidwifery care in these settings. The aim of this paper isHandling editor Seye Abimbola to identify the factors affecting an enabling environmentfor midwives in HFS and to explore the availability and Additional supplementaleffectiveness of support systems for midwives.material is published online only.Methods A structured systematic review was undertakenTo view, please visit the journalto identify peer- reviewed primary research articlesonline (http:// dx.d oi. org/ 10. published between 1995 and 2020.1136/b mjgh- 2021-0 06872).Results In total, 24 papers were included from Afghanistan,Bangladesh, Nigeria, Democratic Republic of Congo, SouthReceived 12 July 2021Sudan and Sudan, Ethiopia, Pakistan, Uganda and Liberia.Accepted 19 December 2021There were two broad themes: (1) the facilitators of, andbarriers to, an enabling environment, and (2) the importanceof effective support systems for midwives. Facilitators were:community involvement and engagement and an adequatesalary, incentives or benefits. Barriers included: security andsafety concerns, culture and gender norms and a lack of Author(s) (or theiremployer(s)) 2022. Re- useinfrastructure and supplies. Support systems were: education,permitted under CC BY- NC. Noprofessional development, supportive supervision, mentorshipcommercial re- use. See rightsand workforce planning.and permissions. Published byConclusion More efforts are needed to develop andBMJ.implement quality midwifery services in HFS. There is1Maternal, Child and Adolescent an urgent need for more action and financing to ensureHealth Program, Burnet Institute,better outcomes and experiences for all women, girls andMelbourne, Victoria, Australiafamilies living in these settings.2Faculty of Health, UniversityPROSPERO registration number CRD42021226323.of Technology Sydney, Sydney,New South Wales, AustraliaPartnership for Maternal,Newborn & Child Health(PMNCH), World HealthOrganization (WHO), Geneva,Switzerland3Correspondence toProfessor Caroline SE Homer; Caroline. homer@b urnet. edu.a uINTRODUCTIONIn 2020, before COVID- 19, approximately23% of the world’s population was estimatedto be living in fragile settings, including 168million people in need of humanitarianassistance and protection.1–3 Women andKey questionsWhat is already known? In 2018, it was estimated that nearly 136 millionpeople were living in humanitarian settings, withsignificant impacts on the health and well- being ofpregnant women, girls and newborn babies. Midwives are essential to the provision of maternaland newborn services in all settings.What are the new findings? There are considerable challenges in providing mid-wifery services, especially to ensure the safety andsecurity of midwives and other health workers. Community engagement and support are essentialto provide quality midwifery services.What do the new findings imply? Strong partnerships with communities should becreated when midwifery services are developed andimplemented in humanitarian and fragile settings. Safety and security for midwives are essential, bothin their health facilities and when travelling to provide care.children bear a substantial burden of theimpact of humanitarian crises and fragilesettings. The number of non- displacedwomen and children living dangerously closeto armed conflict increased from 185 millionwomen and 250 million children in 2000 to265 million women and 368 million children in 2017.4 5 Maternal and child healthoutcomes for those in humanitarian andfragile settings (HFS) are often poor6 andare not on track to meet global, national orregional health targets.7 Nine of 10 countrieswith the highest neonatal mortality rates arein conflict.8 In these settings, health facilities are often not functional, and pregnantHomer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872 1BMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.Enhancing quality midwifery care inhumanitarian and fragile settings: asystematic review of interventions,support systems andenabling environments
BMJ Global HealthMETHODSWe undertook a mixed- methods systematic review. Aninitial protocol was registered and published with PROSPERO in January 2021 (CRD42021226323) and theprotocol reported according to the Preferred Reporting2Items for Systematic Reviews and Meta- Analyses checklist.17 18 Our approach was to search, screen and identifyeligible peer- reviewed studies using qualitative and/orquantitative data collection and analysis methods.19Defining HFS and an enabling environmentThere is no universally agreed definition of an HFS. Thisreview takes its definition of humanitarian settings fromthe Inter- Agency Working Group on Reproductive Healthin Crises as contexts ‘‘ in which an event or series ofevents has resulted in a critical threat to the health, safety,security, or well- being of a community or other largegroup of people. The coping capacity of the affectedcommunity is overwhelmed, in- country infrastructure isdisrupted, and external assistance is required. This canbe the result of events such as armed conflicts, naturaldisasters, epidemics, or famine and often involves population displacement’ (OECD, p2).2 20 Fragile settings arethose that have a combination of exposure to risk andinsufficient coping capacity of the state, systems and/or communities to manage, absorb or mitigate thoserisk.2 Fragility can lead to negative outcomes includingviolence, poverty, inequality, displacement and environmental and political degradation.2Humanitarian settings and fragile states frequentlyoverlap. To reflect this, the classification of HFS usedin this paper categorises countries across a spectrumof fragility with four groupings: highest fragility, veryhigh fragility, high fragility and fragile settings. This wasbased on triangulation of data from five classifications ofhumanitarian and fragile states, that is, OECD,2 WorldBank,21 Fragile State Index,22 the INFORM SeverityIndex,23 and UNOCHA data on humanitarian responseplans.1 More information on the composite HFS classification can be found in online supplemental file 1.We took the UNFPA definition of an enabling environment as one where midwives ‘ can practise to theirfull scope, are accountable for independent decisionswithin the regulated standard operating procedure,work within a functional health infrastructure withadequate human resources, equipment and supplies,have access to timely and respectful consultation,collaboration and referral, be safe from physical andemotional harm and have equitable compensation,including salary and working conditions’ (UNFPA,p34).24 Support systems included education, trainingand supervision, mentorship, psychosocial supportand schemes for continuous quality improvement.25Eligibility criteriaPeer- reviewed primary research articles in English,published between 1995 and 2020, were eligibleregardless of research design. Specifically, we includedprimary studies that used qualitative study designssuch as ethnography, phenomenology, case studies,grounded theory studies and qualitative process evaluations. We also included studies that used both qualitative methods for data collection (eg, focus groupHomer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872BMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.women and girls lack access to trained providers withmidwifery skills.9 10Providing quality care for women and children in anycontext requires a competent and motivated workforceworking within an enabling environment.11 Midwivesare critical for the provision of sexual, reproductive,maternal, newborn, child and adolescent healthcare. Ithas been shown that increases in the coverage of interventions delivered by midwives could save lives.12 Forexample, a substantial increase in coverage of midwiferyservices (25% increase every 5 years) would avert an estimated 41% of maternal deaths, 39% of neonatal deathsand 26% of stillbirths. This would equate to 2.2 millionfewer deaths per year by 2035. Even a more modestincrease in coverage of midwife- delivered interventions(10% increase every 5 years) would avert 1.3 milliondeaths per year by 2035.Midwives provide maternity services as well as otherpreventive health and treatment services. These include:promotion of breastfeeding; immunisation; immediatenewborn care; comprehensive abortion care and post- abortion care; contraceptive services; screening andtreatment of postnatal depression; and better supportfor victims of gender- based violence.13 A shortage ofmidwives is a significant barrier to the provision ofquality sexual, reproductive, maternal, newborn, childand adolescent health services.14 This is especially thecase in HFS where midwives, who are mostly women, maybe deterred from working in these environments due tosecurity concerns.9 10 15The importance of effective midwifery services isevident, yet there is limited knowledge about the interventions, support systems and enabling environments thatcan enhance quality midwifery care in HFS. A supplementpublished with the 2021 State of the World’s MidwiferyReport presented three case studies from Bangladesh,Somalia and the refugee camps in Europe, in a projectknown as the Operational Refugee and Migrant MothersApproach.16 While this provided a unique and importantperspective, it highlighted limited understanding of therole that midwives can play in HFS. The aim of this paper,therefore, is to present the findings of a systematic reviewof the literature on quality of midwifery services in HFS.It identifies and analyses evidence to inform future solutions to enhance quality midwifery care. The review setout to identify:1. Factors affecting an enabling environment for midwives in order to provide high- quality maternity services in HFS.2. Availability and effectiveness of the support systems formidwives.
BMJ Global HealthSearch strategiesSearches were conducted between November andDecember 2020. Databases searched were: PubMed/MEDLINE; Academic Search Complete (EBSCO);EMBASE; CINAHL (EBSCO); Web of Science; Scopus;Nursing and Allied Health (ProQuest); Maternity andInfant Care (Ovid). We conducted an online hand searchby checking reference lists of identified articles. With thesupport of librarians, a search strategy was created usingpredefined terms and synonyms for the intervention,population and setting (online supplemental file 2).Study selectionTitles and abstracts of all search results were importedinto Endnote and duplicates removed. The online reviewsoftware Covidence was used to screen titles, abstractsand full texts.28 Two authors independently reviewedeach title and abstract against the eligibility criteria, withpotentially relevant articles included for full- text review.Full texts were recovered and independently assessedfor eligibility by two reviewers. Disagreements at anystage were resolved by discussion or by involving a thirdreviewer. Where more than one paper reported the samestudy, the papers were collated to ensure the primarystudy was the unit of interest.We used the Mixed Method Appraisal Tool (MMAT)for assessing the quality of studies.29 MMAT is a qualityassessment instrument for quantitative, qualitative andmixed- methods studies in a single tool.30Homer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872Patient and public involvementPatients and the public were not directly involved in thisreview.AnalysisThe findings of each study were imported into NVivoV.12. Coding process was undertaken with a focus onour two research objectives: factors affecting an enablingenvironment and the availability and effectiveness ofsupport systems for midwives.We initially took an inductive approach. We identifiedand extracted categories and concepts that emergedfrom the data and developed codes highlighting the keyissues. As we proceeded through the coding, additionalideas emerged which were organised as concepts.31 Thenext stage was to undertake a deductive process using ourtwo objectives to identify other concepts relating to theseareas specifically. A mind map was developed in NVivoto connect the concepts with our objectives and builda comprehensive picture of the issues.32 Our objectivesdeveloped into the two key themes and we identified aseries of subthemes.We summarised the findings by type of publication,method, context of the study, type of intervention andlevel of fragility. As studies varied in their method,context and outcomes used, it was not possible to pooldata for a formal meta- analysis.33 We therefore undertook a narrative synthesis.31 Narrative synthesis has beenused in previous systematic reviews where the quantitative and qualitative results are integrated to inform thefindings.34 35 We did not undertake any assessment ofmeta- bias(es), such as publication bias across studies orselective reporting within studies.RESULTSIn total, 2500 citations were identified and imported intoEndnote and Covidence (table 1).18 36 After irrelevantand duplicate citations were removed, 461 potentiallyeligible papers were identified (figure 1). We were ableto screen the full text of 422 papers, identifying 39 papersfor assessment. During a data extraction and qualityassessment phase, a further 15 papers were excluded,as there was inadequate or vague information about thestudy population or interventions. For example, it wasunclear whether midwives were included in the study ortheir contribution could not be identified. Ultimately,24 papers were included in the review. Included articleswere summarised and categorised according to their relevance to the objectives of the study (table 2).Of the 24 studies, 14 were qualitative, 7 mixedmethods and 3 quantitative. Most studies were descriptive (n 16). Of the countries included, seven are low- income countries and three are lower- middle- incomecountries.21 Three countries are categorised as havinghighest fragility, two as very high fragility, two as highfragility and three as fragile settings. These countriesincluded Afghanistan,37–43 Bangladesh,44–48 Nigeria,49–523BMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.discussions, individual interviews, observation, diaries,document analysis, open- ended survey questions) andqualitative methods for data analysis (eg, thematicanalysis, framework analysis, grounded theory). Wealso included randomised trials, non- randomised trials,controlled before- and- after studies, interrupted timeseries and repeated measures26 and mixed- methodsstudies, provided they were primary studies and relevant to the review question.The population of interest was midwives/nurse- midwives,according to the scope of practice defined by the International Confederation of Midwives,27 as well as the women,girls and children in their care. Any practices or interventions that targeted health workers working outside thescope of midwifery practice were excluded. Interventionsthat focused on nurses, obstetricians and gynaecologists,paediatricians or community health workers were excluded.Eligible studies were categorised according to the four categories: highest fragility, very high fragility, high fragility orfragile settings.We excluded case reports or case series, letters, editorials,commentaries, reviews, study protocols, conference abstractsor other article types that did not provide primary data and/or were not peer- reviewed. Specific cost- effectiveness studieswere also excluded but studies that included costing data aspart of implementation and feasibility were included.
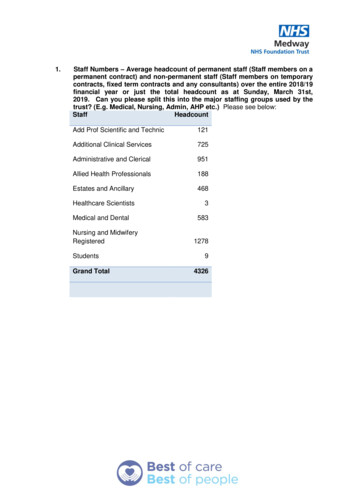
BMJ Global HealthData sourceResultsDuplicateremovedUnrelated articlesremovedReviewed abstractsand titlesCINAHL (EBSCO)Pubmed/Medline237236185236113766858Web of Science2682478663Nursing and Allied Academic Search Complete (EBSCO)74469822812287763737NA21267792461Maternity & Infant Care (OVID)Hand searchedTotal232477 ( 23 handsearch)NA, not available.Democratic Republic of Congo (DRC),53 54 South Sudanand Sudan,55 56 Ethiopia, Pakistan, Uganda and Liberia.Afghanistan (n 7), Bangladesh (n 5), Nigeria (n 4),DRC (n 2) made up most of the studies (table 2). TheFigure 14definition and scope of practice for midwives were oftenunclear for some countries, such as Nigeria, SouthSudan, DRC and Ethiopia. However, studies in Afghanistan, Bangladesh, Pakistan, Sudan and Liberia specifiedPRISMA flow chart showing search results, screening and included papers.Homer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872BMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.Table 1 Results of database search
Target groupMidwives anddoctorsCompareMidwiferyperformancegraduates andof midwiferystudentsgraduates whowere selectedthroughcommunitymobilisationwith thosewho admittedthrough a nationalexamination.Assessmentof emergencyobstetric andnewborn caretraining/servicesAssessment ofMidwives, doctorsmidwifery services and care assistantsto explore cultureof care.Assess midwifery Midwives, doctorsservices toand senior officialsexplore underlyingissues for staffbehavioursInterventionMixed method/retrospectivesurvey.MW studentrecords of the178 trainees werereviewed anddata extracted fordemographics,selection method,performancein knowledgeand skills, anddeployment statusand location.Quantitative/cross- sectionalstudy142 midwives and82 doctorsQualitative/ethnographicstudy23 Interviews wereconducted withsenior doctorsand midwives,resident doctors,newly qualifiedmidwives andcare assistants (2senior midwives8 midwives with 6months–10 23 Interviews wereconducted withsenior doctorsand midwives,resident doctors,newly qualifiedmidwives and careassistantsMethodologyContinued96% of midwifery graduates selected by communities wereemployed, compared with 74% chosen by the Institute of HealthSciences (IHS) and 82% by the National University EntranceExamination (NUEE). 63% of community- selected graduates wereworking in rural locations, compared with 43% recruited by IHSand 9% by the NUEE. While fewer midwifery graduates selectedby communities had completed high school and their academicperformance was slightly lower during training, there was nodifference in their pass rates and acquisition of practical skills.Over 90% of facilities had essential equipment for newbornresuscitation, including a mucus extractor, bag and mask. Morethan 80% of providers had been trained on newborn resuscitation,but midwives were more likely than doctors to receive such trainingas part of preservice education (59% and 35%, respectively,p 0.001). Training was associated with greater knowledge(p 0.001) and clinical skills (p 0.05) in a multivariable model thatadjusted for facility type, provider type and years of experienceoffering emergency obstetric and newborn care services.Most staff members were simply endeavouring to survive in atough working environment where the lack of a shift systeminevitably resulted in staff exhaustion, poor performance and theconstant risk of mistakes leading to censure by management.Doctors and midwives concurred that they did not provide careas they had been taught and blamed the workload, lack of ashift system, insufficient supplies and inadequate support frommanagement.Although healthcare providers generally look the same in hospitalsacross the globe, this study reveals they have different ways ofunderstanding the world. They may work in a ‘caring’ professionbut perceive the purpose of work from innate social norms andvalues, which, for example, can result in guarding their skills ratherthan sharing them. A sense of responsibility to strangers mightclash with kinship obligations, the institutional culture, and thewider social environment. Furthermore, public health institutionsmay not only provide care, they may also be lucrative sources ofincome for political elites.Results/outcomesBMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.Homer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872Highest Fragility Midwifery trainingin post- conflictAfghanistan: tensionsbetween educationalstandards and ruralcommunity needsAfghanistanMansoor, 2012404Highest Fragility Assessing thecapacity for newbornresuscitation andfactors associatedwith providers'knowledge and skills:a cross- sectionalstudy in AfghanistanAfghanistanKim,2013393Highest Fragility Villains or victims?An ethnography ofAfghan maternity staffand the challenge ofhigh- quality eclassificationHighest Fragility Parallel worlds: Anethnography of care inan Afghan nFirst author, yearCharacteristics of included studies#Table 2BMJ Global Health5
Homer CSE, et al. BMJ Global Health 2022;7:e006872. doi:10.1136/bmjgh-2021-006872Zainullah, 201443Bogren,20184578TitleInterventionFragile SettingBangladeshOpportunities,challenges andstrategies whenbuilding a midwiferyprofession. Findingsfrom a qualitativestudy in Bangladeshand NepalHighest Fragility Establishing midwiferyin low- resourcesettings: Guidancefrom a mixed- methodsevaluation of theAfghanistan midwiferyeducation programmeHighest Fragility Factors influencing theretention of midwivesin the public sectorin Afghanistan: Aqualitative assessmentof midwives in eightprovincesWomenTarget groupAssess strategiesfor establishmentof midwiferyEducationMidwivesEvaluation of costs Midwivesand graduateperformanceoutcomes ofthe two typesof preservicemidwiferyeducationprogrammesEvaluation ofMidwives and otherfactors associated stakeholderswith midwifery(MW) deploymentHighest Fragility ‘The midwife helpedTo exploreexperiences ofme. Otherwise Imidwifery carecould have died’:women’s experienceof professionalmidwifery services inrural Afghanistan—aqualitative study in theprovinces Kunar tan6Wood,201342Thommesen, 202041 Afghanistan5CountriesFirst author, yearContinuedQualitativeQuantitativeanalysis ofmidwiferygraduates’performance andcost analysisto estimate theresource requiredto educate amidwife. midwiferyschool graduates(n 138)QualitativeStakeholdersn 33, MWstudents n 35,MW currentlyemployed n 17;MWs formerlyemployed n 16,CHWs n 16Qualitative/exploratory study39 womenparticipated—25who had givenbirth during thelast 6 months,11 mothers- in- law and threecommunitymidwives in theprovinces of Kunarand LaghmanMethodologyContinuedGlobal and national standards brought together midwiferyprofessionals and stakeholders, and helped in the establishmentof midwifery associations. The challenges were nationalcommitments without a full set of supporting policy documents,lack of professional recognition, and competing views, interestsand priorities.Graduates (n 101) achieved an overall mean competency scoreof 63.2% (59.9%–66.6%) on the clinical competency assessmentcompared with 57.3% (49.9%–64.7%) for Institute of HealthSciences graduates (n¼37). Reproductive health activitiesaccounted for 76% of midwives' time over an average of 3months. Approximately 1% of childbirths required referral orresulted in maternal death. On the basis of known costs for theprogrammes, the estimated cost of graduating a class with 25students averaged US 298 939, or US 10 784 per graduate.Several factors affect a midwife throughout her career in thepublic sector, including her selection as a trainee, the trainingitself, deployment to her preassigned post, and working in clinics.Overall, appropriate selection is the key to ensuring deploymentand retention later on in a midwife’s career. Other factors thataffect retention of midwives include civil security concerns in ruralareas, support of family and community, salary levels, professionaldevelopment opportunities and workplace support, and inefficienthuman resources planning in the public sector.Many of the women greatly valued the trained midwives’ life- savingexperience, skills and care, and the latter were important reasonsfor choosing to give birth in a clinic. Women further appreciatedmidwives’ promotion of immediate skin- to- skin contact andbreastfeeding. However, some women experienced rudeness,discrimination and negligence on the part of the midwives.Moreover, relatives’ disapproval, shame and problems withtransport and security were important obstacles to women givingbirth in the clinics.Results/outcomesBMJ Glob Health: first published as 10.1136/bmjgh-2021-006872 on 20 January 2022. Downloaded from http://gh.bmj.com/ on January 21, 2022 by guest. Protected by copyright.6#Table 2BMJ Global Health
Homer CSE, et al. BMJ Global Health 2022;7:e006872. angladeshBangladeshBogren, 2018Bogren, 201847Bogren, 201548Zaman, 202044101112Countries9First author, yearContinuedFragile SettingFragile SettingFragile SettingFragile SettingFragileclassificationInterventionTarget groupMethodologyExperiences of a newcadre of midwives inBangladesh: findingsfrom a mixed methodstudyTowards a midwiferyprofession inBangladesh—asystems approach fora complex worldDevelopment of acontext- specificaccreditationassessment toolfor affirming qualitymidwifery education inBangladeshMidwivesAssessexperiencesof Midwiferystudents ontheir midwiferyeducation andtheir first clinicalpost as qualifiedmidwifeMidwivesAssess howMidwivesstakeholderspromote midwiferyprofessionAssess thefeasibility ofdevelopment of acontext- specificaccreditationassessment toolfor midwiferyeducationMixed methodInterviewing329 midwivesand conductingsix focus groupdiscussions with43 midwivesand midwiferystudents.Qualitative/explorative study.Governmentn 4; academian 3; Professionalassociation n 3;donors n 9; NGOsn 6Mixed methods(using quantitativeand descriptivequestionnaire).123 nursingeducatorsteaching the 3years diplomamidwiferyeducationprogramme.What preventsAssess midwifery Midwifery students Qualitativemidwifery quality care services in relation67 midwiferyin Bangladesh? Ato quality of carestudentsfocus group enquirywith midwiferystudentsTitleContinuedMost of the midwives were satisfied with different dimensionsof their education programme, with the exception of the levelof exposure they had to the rural communities during theirprogramme. Out of 329 midwives, 50% received tuition feewaivers, while 46% received funding for educational materialsand 40% received free accommodation. The satisfaction withthe various aspects of the current posting was high and nearly allmidwives reported a desire to work in the public sector in the longrun. However, a significant proportion of the midwives expressedconcerns with equipment, accommodation, transport and prospectof transfers.Collaboration between organisations was valued, as more couldbe achieved compared with what an individual organisation coulddo. Significant results of this were that two midwifery curricula andfaculty developments had been produced. Although collaborationwas mostly seen as something positive to move the systemforward, the approach to reach the set goal varied with differentinterests, priorities and concerns, both on individual organisationallevel and at system level. Frequent struggles between individualphilosophies and organisational mandates were seen as competinginterests for advancing the national priorities. It would appear thatnewcomers with innovative ideas were denied access on the sameterms as other actors.Provides insight into the development of a context- specificaccreditation assessment tool for Bangladesh. Importantcomponents to be included in this accreditation tool are presentedunder the following categories and domains: ‘organisation andadministration’, ‘midwifery faculty’, ‘student body’, ‘curriculumcontent’, ‘resources, facilities and services’ and ‘assessmentstrategies’. The identified components were a prerequisite toensure that midwifery students achieve the intended learningoutcomes of the midwifery curriculum, and hence contribute toa strong midwifery workforce. The components further ensurewell- prepared teachers and a standardised curriculum supportedat policy level to enable effective deployment of professionalmidwives in the existing health system.Professional barriers include heavy workloads with a shortage ofstaff who were not utilised to their full capacity within the healthsystem. The reason for this was a lack of recognition in themedical hierarchy, leaving midwives with low levels of autonomy.Economical barriers were reflected by lack of supplies and hospitalbeds, midwives earning only low and/or irregular sala
The importance of effective midwifery services is evident, yet there is limited knowledge about the inter-ventions, support systems and enabling environments that can enhance quality midwifery care in HFS. A supplement published with the 2021 State of the World's Midwifery Report presented three case studies from Bangladesh,