Transcription
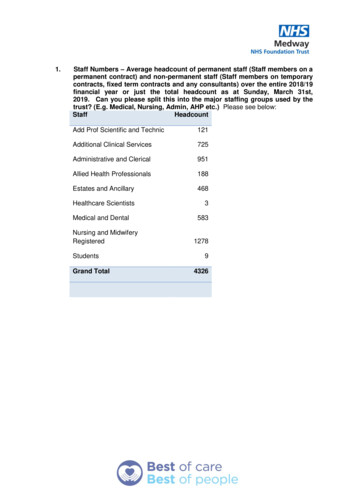
SCOPE OF PRACTICEFORMIDWIFERY EDUCATOR&NURSE PRACTITIONER MIDWIFEMinistry of Health & Family WelfareGovernment of IndiaJune, 2021
2SCOPE OF PRACTICEFOR MIDWIVESCONTENTS1 Introduction . P42 Definition of Midwife (International context) . P43 Definition of Nurse Practitioner Midwife (Indian context) . P44 Scope of Practice of Midwifery Educators and Nurse Practitioner Midwife . P6A. Pre-pergnancy care (Sexual and Reproductive Health)B. Antenatal careC. Care during labour and Birth(Intrapartum care)D. Ongoing care of women and Newborns (Postpartum care)5 Additional Roles & Responsibilities for Midwifery Educators. P86 Principles of Collaborative Care . P87 Annexures . P9Annexure 1 :Laboratory TestAnnexure 2 :MedicationsAnnexure 3 (a): Procedural Competencies/Skills that NPMs can performAnnexure 3 (b): Maternal and Newborn Conditions that an NPM can performAnnexure 4:SOPs for NPMs responsibilities
SCOPE OF PRACTICEFOR MIDWIVESList of FPPPHPPIUCDTdTSHAntenatal CorticosteroidsAcid Fast BacillusBirth Preparedness and Complication ReadinessComplete Blood CountComprehensive Emergency Obstetric and Neonatal CareCephalopelvic DisproportionCardiotocographyDilatation and CurettageDilatation and EvacuationDaily Fetal Movement CountDeep Venous ThrombosisExpressed breast milkEmergency Contraceptive PillsInternational Confederation of MidwivesIndian Nursing CouncilIntrauterine Contraceptive DeviceMidwifery EducatorMidwifery Led Care UnitMedical Methods of AbortionMedical Nutrition TherapyNurse Practitioner MidwifeNon-Stress-TestOral Contraceptive PillsOral Glucose Tolerance TestObstetric Led Care UnitPre EclampsiaPost Partum Family PlanningPost Partum HemorrhagePost Partum Intrauterine Contraceptive DeviceTetanus and Adult DiphtheriaThyroid Stimulating Hormone3
4SCOPE OF PRACTICEFOR MIDWIVESINTRODUCTIONThe Government of India (GoI) has launched the Midwifery Initiativeto improve the quality of service provision for strengtheningreproductive, maternal and neonatal health. This initiative will createa new cadre of “Nurse Practitioner in Midwifery” (NPM) who are skilled inaccordance with International Confederation of Midwives (ICM) competencies,knowledgeable and competent in providing skilled, compassionate, respectful,women centered care.These midwifery services will primarily be provided through ‘MidwifeLed Care Units’ (MLCUs). One of the key components of establishing theNPM cadre and embedding them in the health system is a clear “Scopeof Practice” which also guides their education, regulation and ongoingprofessional development to ensure optimal midwifery care.1. Definition of a Midwife (International Context)The ICM defines a Midwife as:“ a person who has successfully completed a midwifery educationprogramme that is duly recognized in the country where it is located andthat is based on the International Confederation of Midwives (ICM) EssentialCompetencies for basic midwifery practice and the framework of the ICMGlobal Standards for Midwifery Education; has acquired the requisitequalifications to be registered and/or legally licensed to practice midwiferyand use the title ‘midwife’ and who demonstrates competency in the practiceof midwifery.” (ICM1).2. Definition of a Nurse Practitioner Midwife (NPM) (IndianContext)An NPM is one who has successfully completed the 18 months' NursePractitioner in Midwifery training program designed by the Indian NursingCouncil (INC) based on the ICM essential competencies for basic midwiferypractice and recognized in India by the Ministry of Health and FamilyWelfare, Government of India, and who will be registered and licensed topractice midwifery in high caseload facilities across the country under thetitle ‘Nurse Practitioner Midwife', upon demonstrating competency in thepractice of les/definitions-files/2018/06/eng-definition of the midwife 2017.pdf
SCOPE OF PRACTICEFOR MIDWIVES The NPM is a responsible and accountable professional who works inpartnership with women to provide the necessary support, respectfulcare and advice to women and their families during pregnancy,childbirth and the postpartum periodThe NPM will function primarily in the MLCUs alongsideComprehensive Emergency Obstetric and Neonatal Care (CEmONC)centres, under the overall supervision of the Obstetrician at thefacility, as envisaged by GoI. MLCUs shall promote normality duringpregnancy, labour, birth and the postpartum period, early and timelydetection of complications, carry out first line emergency measures,refer and facilitate access to a full range of medical and surgical careas well as provide preventive careThe NPM will be able to competently perform the full scope of practiceas per the education and training curriculum laid down by INC inaccordance with MoHFW regulations and guidelines.They are fully responsible and accountable to provide care withintheir defined scope of practice in the countryThey have the authority within their area of expertise to: Educate and counsel women and their families on birthpreparedness and complication readiness (BPCR), care prior to,during and after pregnancy, care of the healthy newborn, healthytiming and spacing of pregnancy including postpartum familyplanning and other health Advocate for women’s needs, autonomy and agency Order and interpret diagnostic procedures and laboratory tests(Annexure 1) Prescribe selected medications (Annexure 2) Assess and triage women at the time of admission and refer thehigh-risk cases to the Obstetric Led Care Unit (OLCU) Provide care for women, and their newborns according to bestevidence during normal pregnancy, labour, birth and the postnatalperiod including identification and initial management of selectedcomplications during this period Consult with and refer to other professionals and services for careoutside of their scope of practice and ensure continuity of carefrom preconception to the postnatal period Document and review provision of care5
6SCOPE OF PRACTICEFOR MIDWIVESThe primary function of NPMs is to act professionally within their workenvironment to ensure the wellbeing of childbearing woman and hernewborn. NPMs should instill confidence in women for their capabilitiesin childbirth and empower them to assume responsibility for their health,to enable them to learn for themselves, to build on their strengths and toaccess services in a timely way.3. Scope of Practice for ME & NPMApplies to specialized midwifery care competencies gained through the 18months educational program that is competency-based education (Annexure3).This document is combined with and adapted from key competencies foressential midwifery practice (ICM 2019) and sets out the contours for NPMpractice in India as follows:A. Pre-pregnancy Care (Sexual and Reproductive Health) Provide Family planning counselling and servicesProvide Pre-conception care and counsellingPerform measures in prevention and screening for SexuallyTransmitted Infections and advice treatment based on the syndromicmanagement approachB. Antenatal care Determine health status of pregnant womenDetect and confirm pregnancy, estimate gestational age fromhistory, physical examination and advice on laboratory test from therecommended list of investigationsMonitor the progression of pregnancyAssess fetal and maternal wellbeingPromote and support healthy behaviors that improve women'swellbeing including ANC exercises.Detect, manage, and refer women with complicated pregnanciesProvide counselling to the women and their family on the following:Preparation of birth preparedness and complication readiness plan Antenatal education and anticipatory guidance related topregnancy, birth, breastfeeding, parenthood, postpartum family2For 2 hours after birth to the woman and newborn3Include management of shoulder dystocia; initial management fetal distress; cord prolapse etc
SCOPE OF PRACTICEFOR MIDWIVES planning and change in the family.Self-care in normal pregnancy at every contactPregnancy options and care to women with unintended ormistimed pregnancySafe abortion services and post abortion care to womenPost-partum & Post- abortal Family Planning MethodsC. Care during labour and birth (Intrapartum Care) Confirm onset of labourProvide supportive respectful care to all women in normal labourat term and in immediate postnatal period 2(e.g. facilitate alternatebirthing positions, birth companionship chosen by women, facilitateinformed choices/rights-based care)Identify complications during labour, childbirth and the immediatepostpartum period, and provide immediate management3 andreferral when indicatedAssist physiological birthing processes leading to a safe birth andactive management of the third stage of labour for the prevention ofpostpartum hemorrhageProvide immediate essential newborn care (warmth, early initiationof breastfeeding, delayed cord clamping, Vitamin K, eye and cord care)Perform neonatal resuscitation when indicatedIdentify newborn complications, perform immediate managementand when indicated, initiate a timely referralPerform and repair episiotomy for evidence based indications withthe woman’s consentRepair perineal, vaginal and vulval lacerations (excluding 3rd /4thdegree or complicated tears)D. Ongoing care of women and newborns (Postpartum Care) Provide postnatal care which focuses on continuing health assessmentof women and infant, health education, intake of IFA & Calcium,support for breastfeeding, detection of complications and provisionof family planning servicesSupport maternal and infant bonding and healthy child-rearingpractices7
8SCOPE OF PRACTICEFOR MIDWIVES Identify postpartum complications in the women and newborn,provide immediate management and when indicated, initiate referralpromptlyCounsel on postpartum family planning servicesProvide anticipatory guidance to the woman and her family on promptrecognition of danger signs in both the mother and baby and seekimmediate care4. Additional Roles & Responsibility for MEIn addition to the above-mentioned roles illustrated from points A to D, theME’s will have the following additional responsibilities: Play a dual role of imparting training to the NPMs at State MidwiferyTraining Institutes alongside performing clinical practice themselves Supervise the NPMs during their clinical practice sessions Mentor and handhold the NPMs during and after the training5. Principles of Collaborative CareWhile NPMs are a specialized cadre of nurse-midwives in India and are fullyresponsible and accountable for care within their defined scope of practice,they work within a health care system that recognizes the need for consultation,collaboration and referral between health care professionals. Collaborationbetween NPMs, Obstetricians, Pediatricians and Medical Officers In-charge(MO) requires confidence, trust and effectivecommunication. When effectivecollaboration occurs, the specialists can extend their contribution to thecare of women and newborns experiencing complications and requiringspecialized care.NPMs can also be involved in the care of women with high-risk pregnancies,pregnancy related complications and women/newborns as part of themultidisciplinary team. In these situations, the overall accountability restswith the Obstetrician/Mo I/c of the hospital/health center.
SCOPE OF PRACTICEFOR MIDWIVESLaboratory TestsLaboratory n/RoutineTORCH InfectionsTORCH InfectionsUTIUTIUncomplicated MalariaSeverePE / e PE/ EclampsiaTBin PregnancyThyroidDisordersTB in PregnancyAnnexure 1Annexure 1MaternalMaternal Laboratory tests to orderLaboratorytests to orderPregnancy test(Serum/Urine)Haemoglobin,Blood Count (CBC)*Pregnancy testComplete(Serum/Urine)Haemoglobin,CompleteBlood group, Rhtyping Blood Count (CBC)*HepatitisB (HBsAg)/Hepatitis C (HCV DNA)*Blood group,Rh typingMulti-reagentUrinedipsticksHepatitis B (HBsAg)/ Hepatitis C (HCV DNA)*75gm Oral GlucoseMulti-reagentUrineTolerancedipsticks Test (OGTT)75 gm Oral Glucose Tolerance Test (OGTT)Rapid POC tests: HIV, syphilis. RPR for syphilis ifavailableRapid POC tests: HIV, syphilis. RPR for syphilis ifTORCHavailablePanel*Multi-reagentTORCH Panel*Urine dipsticks: albumin, sugarnitrites, leucocytes,Multi-reagentUrineblooddipsticks: albumin, sugarUrinemicroscopynitrites, leucocytes, bloodUrine cultureand sensitivity*microscopyRapidtest: Malaria/ thick drop or thin smearUrine cultureand sensitivity*Urine dipsticks:AlbuminRapidtest: Malaria/ thick drop or thin smearThyroidStimulatingHarmone (TSH)*Urine dipsticks:AlbuminSputumAcid-FastHarmoneBacillus (AFB)Thyroid forStimulating(TSH)*to Indicationin individualSputum*Subjectfor Acid-FastBacillus(AFB) pregnant women*Subject to Indication in individual pregnant women779
10SCOPE OF PRACTICEFOR MIDWIVESAnnexure 2MedicationsConditionPrevention/RoutinePreterm labourIV dia, Gonorrhoea,Vaginal candida infection,BV/Trichomoniasis)UTIHypertensive disorders inPregnancyManagement of PPHPuerperal infectionConditionPreventive treatmentPossible serious illness,severe umbilical infectionor severe skin infectionGonococcal eye infectionVaccinationsMaternalMedications to prescribeFolic Acid, Iron Folic Acid tabletsCalcium with Vit D3AlbendazoleTd vaccineMedical-Nutrition Therapy for potential gestational diabetes(Women with GDM will be referred for ANC with OBGYNs)Antenatal corticosteroidsNormal salineRinger’s LactateParacetamol tabletsFor the imazolevaginal pessariesFor the partner:Tetracycline /Doxycycline/CiprofloxacinAmoxicillin, NitrofurantoinLoading dose of Magnesium SulphateOxytocinAmpicillin, Metronidazole and GentamycinNewbornMedications to prescribeVitamin K1ART prophylaxis for newborns of HIV ycinBirth dose BCG ‘0’ dose Polio Hepatitis followed by the routine immunization as perUIP8
SCOPE OF PRACTICEFOR MIDWIVESAnnexure 3(a)Procedural competencies/skills that NPMs can perform independently,in collaboration or referNPM can do independentlyNPM can do undersupervision/CollaborationANTENATAL CAREHealth assessment – medical andobstetric history collection, physicaland obstetric examinationUrine pregnancy testEstimation of Hemoglobin usingSahli’s Hemoglobinometer/DigitalHemoglobinometerUrine testing for albumin and sugar ,Testing blood sugar by 75 gm OGTTusing Glucometer and MNTPreparation of peripheral smear formalariaPoint of care HIV testPoint of care syphilis testPreparation of woman for USGCounsel on use of Kick chart / DFMC(daily fetal movement count) in the3rd trimester; evaluate reduced kickcountsPreparation and recording of CTG /NSTAntenatal counseling – diet, exercise,rest, personal care, birth preparedness,complication readiness, Post PartumFamily PlanningAdministration of TdPrescription of iron and folic acidtablets, albendazole tablets, calciumPrenatal counseling and care ofgeneral and vulnerable groups suchas adolescent pregnant womanManagement of mild andmoderate anemia (7-9%)Medical Nutrition therapy(MNT)Women with UncomplicatedMalariaNPM should referWomen with high riskpregnancy or anyother complication.(Refer to Annexure 3b)Women with severe( 7gm%) anemiaWomen with GDM notcontrolled by MNTWomen with SevereMalariaWomen with HIVWomen with STIs/ RTIReduced fetalmovements/No fetalmovementsNon reassuringNST/CTG9Women withcomplications(RefAnnexure 3b)11
12SCOPE OF PRACTICEFOR MIDWIVESAnnexure 3(a)Procedural competencies/skills that NPMs can perform independently,in collaboration or referNPM can do independentlyNPM can do TAL CAREIdentification,assessmentof womanHealthassessment– medicalandin labour history collection, physicalobstetricand obstetric gh Dopplerand Cardiotocography(CTG)Estimationof HemoglobinusingPlottingHemoglobinometer/Digitaland interpretation ationduringlabourUrinetestingfor albuminandsugar ,includingclinicalpelvimetryTesting blood sugar by 75 gm OGTTusing Glucometer and MNTPreparation offorperipheralbirth– Settingofupof theroom / unitPointcareHIVdeliverytestSupportive,care of womenPointof carerespectfulsyphilis testin labour – ambulation,positions,Preparationof woman forUSGhydration,birthcompanionshipCounsel on use of Kick chart / DFMCPain managementduringlabour:non(dailyfetal movementcount)in therd trimester; evaluate reduced kick–pharmacological3Conductionof delivery as percountsprotocol– facilitatenormalof CTG /Preparationand recordingphysiologicalbirthingNSTIdentify perineal and vaginal tearsAntenatal counseling – diet, rof 1st and2nddegreecomplicationreadiness,Postperineal and vaginal tears PartumFamily PlanningAdministration of TdEssential newbornPrescriptionof ironcareand folic acidNewbornresuscitationtablets, albendazole tablets, calciumPrenatal counseling and care ofActive managementof thirdstageofgeneraland vulnerablegroupssuchlabouras adolescent pregnant womanInsertion of PPIUCDExamination of placentaCare during fourth stage of labourInitiation of breast feeding andlactation managementAssessment and weighing of newbornAdministration of Vitamin KPostnatal assessment andcare-women and newbornManagement of mild andmoderate anemia (7-9%)Medical Nutrition therapy(MNT)Women with UncomplicatedMalariaPharmacologic painmanagementNPM should referWomen with high riskpregnancy or anyother complication.complication.((ReferRefer toto AnnexureAnnexure 3b)3b)Non reassuring CTGWomen with severeCPD,contracted( 7gm%)anemiapelvis,cervical dystociaProlongedlabour,Women withGDM notobstructedlabour,controlled by MNTother complicationsWomen with SevereMalariaWomen with HIVWomen with STIs/ RTIReduced fetalmovements/No fetalmovementsProlonged 2nd secondstage,vaccum, forceps,Non reassuringObstructedNST/CTG labourSuspected cervicaltearsManagement of 3rd and4th degree perineal,vaginalNeonatalcomplicationsWomen with9complications(RefAnnexure 3b)Care of small/pre- term newborn Sick newbornNewbornPOSTNATALCARE10Women with high riskpregnancy or anyother complication.
SCOPE OF PRACTICEMIDWIVESAnnexure FOR3(a)Procedural competencies/skills that NPMs can perform independently,in collaboration or referNPM can do independentlyAdministration of Vitamin KNewbornNPM can do undersupervision/CollaborationPOSTNATAL CAREANTENATALPostnatalassessmentand andHealth assessment– medicalcare-womenand collection,newborn physicalobstetric historyand obstetric examinationUrine pregnancy testPerineal/ EpisiotomycareusingManagement of mild andEstimationof HemoglobinBreast Hemoglobinometer/DigitalcareSahli’smoderate anemia (7-9%)Postnatal counseling – diet, ygiene,testing foralbuminand sugar ,Medical Nutrition therapyTesting blood ofsugarby 75gm rnGlucometerand MNTof sexualand, resumptionPreparationperipheralsmear forWomen with Uncomplicatedactivity, and ofreturnto fertility,malariaconsumption of IFA and calcium for 6 MalariaPointof care HIV testmonthsPoint of carefamilysyphilistestPostpartumplanningNEWBORN CAREPreparation of woman for USGKangarooMotherCareCounsel on use of Kick chart / DFMCIdentificationof minorcount)disordersof(daily fetal movementin therd3trimester;evaluatereducedkicknewborn and their managementcounts immunization–as per theNeonatalPreparationand recordingof CTG /UniversalImmunizationProgramNSTCARE OF WOMAN WITH COMPLICATIONSIdentification of antenatalAntenatalcounselingcomplicationspre- – diet, exercise,rest,personal care, icationreadiness,PostPartumantepartum hemorrhage, diabetes,FamilythyroidPlanningdisorders& medical disordersinpregnancy of TdAdministrationPrescription of iron and folic acidGlucosealbendazoleChallenge cecounselingtest/OGTTand care ofgeneraland vulnerable groups suchusingGlucometerasadolescentHypertensive pregnantDisorderswomanof Pregnancy- Gestational HTN,management of Severe PEidentification, diagnosis andadministrationof loadingadministration of loading dose of9dose of MgSO4 and antiMgSO4 for severe PE/eclampsiahypertensive drugs11NPM should referWomen with high riskpregnancy or anyother Annexure3b)3b)Women with severe( 7gm%) anemiaPostnatalcomplications(ReferWomen with GDMnottoAnnexure3b)controlled by MNTWomen with SevereMalariaWomen with HIVWomenwith STIs/ RTITuballigationReduced fetalSicknewborn fetalmovements/NomovementsNon reassuringNST/CTGWomen with severepreeclampsia/eclampsia,severe anemia, APH,diabetes, thyroiddisorders& medicaldisorders in pregnancyWomen with GDM notcontrolledby MNTWomen withcomplications(RefAnnexure 3b)Severepre-eclampsia/eclampsia13
consumption of IFA and calcium for 6monthsSCOPE OF PRACTICEFORMIDWIVES14Postpartumfamily planningNEWBORN CARETuballigation es/skillsthat NPMs can perform independently,Identification of minor disorders ofSick newbornin collaboration or refernewborn and their managementNeonatalper theNPMimmunization–ascan do independentlyNPM can do underNPM should referUniversal Immunization Programsupervision/CollaborationCARE OF WOMANWITH CARECOMPLICATIONSANTENATALIdentificationof fetaldistressandand itsFetaldistressantenatalsevereHealth assessment– medicalWomenwith yor andobstetric hemorrhage,diabetes,severeAPH,Refer toanemia,Annexure3b)Prepare for Vacuum rdersdiabetes,thyroidUrine pregnancytestDiagnosisof MalpresentationsandMalpresentations andinpregnancydisorders&Management of mild andEstimation of erral entationHemoglobinometer/Digitalmoderate anemia (7-9%)( 7gm%)anemiaCordor Cord ProlapseCordprolapsedGlucoseChallenge TestWomen with GDM notHemoglobinometerInitialstabilizationand /controlledby GDMMNT notGlucoseTolerancetest/OGTTreferral(dependingupon theUrinetestingfor albuminandstagesugarof,Medical Nutrition therapyWomenwithusing y 75 begmcapableOGTT(MNT)controlled by Severeofinitialmanagementanddeliveryifusing Glucometer and MNTpre-eclampsia/managementof Severe PEsecondstageofofdiagnosislabour. andidentification,Preparationperipheralsmear forWomenwith UncomplicatedWomenwith Severeeclampsiaadministrationof loadingDiagnosisof PretermLabour–correctAntenatal corticosteroidsPretermDeliveryadministrationof loadingdose ds)MgSO4severePE/eclampsiaPointofforcareHIV testWomen with HIVadministration of AntenatalhypertensivedrugsPoint of care syphilis testWomen with STIs/ RTICoticosteroids as per indication and referPreparation of woman for USGPrepare for Breech deliveryCounsel on use of Kick chart / DFMC(depending upon the stage of labour).(daily fetal movement count) in theMidwivesshould be capable of initialrd trimester; evaluate reduced kick3management and delivery if secondcountsof labour.stagePreparationrecording pregnancyof CTG /Diagnosisof andRH(Negative)NSTDiagnosis and management of STIsAntenatalcounseling – diet, exercise,during sandcare,referralcomplicationreadiness,Post PartumProlonged labourFamily PlanningPrepare for Forceps birthAdministration of TdManual removal of thePrescription of iron and folic acidplacenta(already separated placenta)tablets, albendazole tablets, calciumDiagnosis and management of PPH Prenatal counseling and care ofBimanual Compression of uterus,general and vulnerable groups suchBalloon Tamponade for Atonic uterus,as adolescent pregnant womanAortic Compression for PPH,Prescription and administration offluids, uterotonics and electrolytesthrough intravenous route.Identification and first aidmanagement of obstetric shockDiagnosis and initial management ofpuerperal sepsis11Administration of Anti-DimmunoglobulinManual removal of theplacentaStabilize and refer9Stabilize and referStabilize and refer12Breech deliveryReduced fetalmovements/No fetalmovementsNon reassuringDeliveryof RHNST/CTG(Negative) pregnancySTIs withcomplicationsProlonged labourForceps BirthMorbid adherentplacentaWomen withcomplications(RefAnnexure 3b)Management ofpuerperal sepsis
consumption of IFA and calcium for 6monthsPostpartum family planningSCOPE OF PRACTICENEWBORN CAREFOR MIDWIVES 15Tuballigation es/skillsthat NPMs can perform independently,Identification of minor disorders ofSick newbornin collaboration or refernewborn and their managementNeonatalper theNPMimmunization–ascan do independentlyNPM can do underNPM should referUniversal Immunization Programsupervision/CollaborationCARE OF WOMANWITH reHealthassessment– medicalandWomen epreobstetrichistorycollection, physicalpregnancyor IdentificationsuspectedDVTStabilize and referDVTanditsandobstetric ofexaminationothercomplication.(antepartum hemorrhage, diabetes,severeanemia,APH,managementRefer to andreferManagementofUrine pregnancy testin pregnancydisorders&complications– UTI, ObstetricpostpartumManagement of mild andEstimationof nancycomplications(RefertofistulasetcSahli’s Hemoglobinometer/Digitalmoderate anemia (7-9%)( 7gm%) re3b)Hemoglobinometercontrolledby GDMMNT notRISK NEWBORNGlucoseTolerancetest/OGTTUrinetestingfor albuminand sugar HIGH,MedicalNutrition therapyWomenwithFeedingof high-risknewborn–AssistingSicknewbornusing GlucometerTestingbloodsugar by75 gm OGTT(MNT) in neonatalcontrolledby iveDisordersofPregnancyGestationalHTN,Severeusing Glucometer and MNTpre-eclampsia/managementof Severe eparationofdiagnosisperipheralsmearforWomenwith UncomplicatedWomenwith Severeeclampsiaadministration of loading(Naso/orogastrictube ) dose ofadministrationof aAdministrationmedication – oral / dose of MgSO4 and antiPointofforcareHIVoftestWomen with HIVhypertensivedrugsparenteralPoint of care syphilis testWomen with STIs/ RTINeonataldrugPreparationof calculationwoman for USGOxygenadministration11Counsel on use of Kick chart / DFMCCareneonatein incubator(dailyoffetalmovementcount)/in thewarmer/ ventilator3rd trimester;evaluate reduced kickcountsCareof neonate on phototherapyAssist in exchangetransfusionPreparation and recording of CTG /Organizedifferent levels of neonatalNSTcareTransportationof high-risknewbornAntenatalcounseling– diet, exercise,rest, personal care, birth preparedness,FAMILY PLANNINGcomplicationreadiness,Post PartumFamily planningcounselingFamilyPlanningDeterminemedical eligibility, supportAdministrationof Tdinformed decisionmaking andPrescriptionofironandacidprovide contraceptiveoffolicchoicetablets,tablets, calcium(except albendazolepermanent methods).Prenatal counselingand care ofProvisionofgeneraland vulnerablegroups such Condoms(Nirodh)as adolescent pregnant woman OCP’s( Mala-N , Chhaya) ECP (Ezy Pill)9 Injectables(Antara)Insertion and removal of IntervalIUCDInsertion and removal ofPPIUCD/PAIUCD13Reduced rmovementsNon reassuringNST/CTGPermanent method ofSterilizationWomen withcomplications(RefAnnexure 3b)
Neonatal drug calculationOxygen administrationSCOPE OF PRACTICEFORMIDWIVES16Careof neonate in incubator /NeonatalintubationAnnexure3(a) /ventilatorwarmer / ventilatorCareof neonate competencies/skillson phototherapyAssistexchangeProceduralthatinNPMscan perform independently,transfusionin collaboration or referOrganize different levels of neonatalcare NPM can do independentlyNPM can do underNPM should referTransportation of high-risk NATALCAREFamilyplanningcounselingPreparationof thewomanforandAssist in Tubectomy,Health assessment– medicalWomen with high riskPostpartumsterilizationobstetric historycollection,physicalpregnancy orany ofDeterminemedicaleligibility,support VasectomyPerman
Competencies for basic midwifery practice and the framework of the ICM Global Standards for Midwifery Education; has acquired the requisite qualifications to be registered and/or legally licensed to practice midwifery and use the title 'midwife' and who demonstrates competency in the practice of midwifery." (ICM1). 2.