Transcription
COREMetadata, citation and similar papers at core.ac.ukProvided by Springer - Publisher ConnectorDiabetes Ther (2013) 4:1–11DOI 10.1007/s13300-012-0017-4REVIEWGlucose Meters with Built-In Automated BolusCalculator: Gadget or Real Value for Insulin-TreatedDiabetic Patients?Ides M. Colin Isabelle ParisTo view enhanced content go to www.diabetestherapy-open.comReceived: November 5, 2012 / Published online: December 19, 2012Ó The Author(s) 2012. This article is published with open access at Springerlink.comABSTRACTthe quality of life of ABC users. It appears that,Self-monitoring of blood glucose is now widelyas long as the education provided by caregiversremains a top priority, BGMs with a built-inrecognized as efficacious to enhance andABC (more than just electronic gadgets) can befacilitate diabetes management. More than justa means of recording and storing data, someregarded as bringing real value to insulintreated patients with diabetes.blood glucose meters (BGMs) are now designedwith an embedded automated bolus calculator(ABC) with the goal to propose patientsrecommendations about insulin dosage. Thegrowing literature in this field tends to claimthat these new smart BGMs make patient’s lifeeasier and decision making safer. The mainKeywords: ycemia;Self-monitoring; Quality of lifeINTRODUCTIONpurpose of this review is to verify whether BGMswith a built-in ABC indeed improve thewillingness and the ability of insulin-treatedpatients to make adequate therapeutic decisionsand positively impact the metabolic control andI. M. Colin (&) I. ParisUnité d’Endocrino-Diabétologie, Département deMédecine Interne, CHR Saint Joseph-Hôpital deWarquignies, 7000 Mons, Belgiume-mail: decadesconvincingly demonstrates that adequate andsustainable metabolic control in people withdiabetesresultsinbettermicro-andmacrovascular outcomes [1–6]. In addition,when this control occurs early on, it mayconfer a so-called metabolic memory [6].However, it must be admitted that suchachievement remains elusive in a significantproportion of patients, as more than 60% ofthem are not reaching the advised glycatedEnhanced content for this article isavailable on the journal web site:www.diabetestherapy-open.comhemoglobin (HbA1c) goal of \7% [7].In addition to marked improvements in themedicaltreatmentofdiabetes,increasing123
Diabetes Ther (2013) 4:1–112evidence indicates that regular assessment ofvariability, and reduced fear and rate ofblood glucose (BG) levels may help insulin-hypoglycemia.treated patients to achieve better glycemiccontrol. Self-monitoring of BG (SMBG)contributes to better adjustment of therapies,and helps to reach treat-to-target goals. Moreimportantly, SMBG can act as an educationaltool to support patients to better adhere to theirtreatment [8–16]. SMBG may provide fruitfulfeedback about how nutrition therapy, physicalactivity, and medications influence BG levelsand alerts about hypo- and hyperglycemia [15].However, some patients are reluctant to useSMBG due to the pain associated with fingersticks and the cost associated with SMBGsupplies. Additionally, some patients areunable to interpret SMBG data and translate itinto appropriate therapeutic decisions [15].One way to improve SMBG acceptance is toprovide therapy algorithms to support patients[especially those treated by multiple dailyinjection (MDI) or continuous subcutaneousinsulin infusion (CSII)] when interpreting theirvalues, and to react accordingly. Such tools arealready on the market.METHODSPremeal Short-Acting Insulin DoseCalculationsFor SMBG to be considered useful, it should beused regularly and correctly at the very least.This goal is achieved when patients andhealthcare providers (HCPs) know how totranslate the data into appropriate insulin doseadjustments [16]. To help patients make theright decision, software has been developed tocalculate doses of short-acting insulin beforemeals. This type of software has been availablein insulin pumps for over 10 years, but was onlyrecently integrated into BGMs and mobiledevice applications [17]. MDI- and atics before deciding on a premealshort-acting insulin dose, at least three-timesdaily. Patients are supposed to calculate theirinsulin dose based on the following formula:glucose load ðgÞIGRðaBGLÞ ðtBGLÞþ ½IOB CFInsulin dosage ðU) ¼The question raised in this review is whether BGInsulin dosage is expressed in units (U). Themeters (BGMs) with a built-in automated bolusfirst part of the equation corresponds to adivision between the glucose load and thecalculator (ABC) represent an added value inpatient performance and ability to make theinsulin to glucose (or carbohydrate) ratioright therapeutic decisions, which may impactboth metabolic control and quality of life. A(IGR). The glucose load, expressed in grams(g), represents the amount of glucose intendedliterature search was carried out using Medlineto be consumed, whereas IGR represents howmany grams of ingested glucose 1 U of insulinand PubMed to select papers where an ABC wasused in addition to SMBG. The papers quoted incovers. According to Walsh et al., IGR isthis review were selected to bring insights intospecificquestionsconcerningimprovedcalculated as: 5.7 9 weight (kg)/total daily dose(TDD) [18]. The correction dose, the second partcapability of patients to make therapeuticdecisions, treatment satisfaction, improvedof the equation, is calculated by subtracting theactual blood glucose level (aBGL) from themetabolic control and decreased glycemictarget blood glucose level (tBGL), divided by123
Diabetes Ther (2013) 4:1–113the correction factor (CF), also referred to as theto transmit data to web databases where theyinsulin sensitivity factor (ISF) in other studiesare interpreted by specialized software systems[19–22]. CF represents how much 1 unit ofinsulin lowers BG and is calculated as:[28].1,960 mg/dL/TDD, according to Walsh et al.[18]. Insulin on board (IOB), the third part ofDo BGMs with Built-In ABCs Help InsulinTreated Patients to Make Appropriatethe equation, corresponds to how much insulinTherapeutic Decisions, While ImprovingTreatment Satisfaction?remains theoretically active in the body fromthe last dose. The IOB amount should be takeninto account and subtracted from the correctiondose. Of note, King recently proposed roundedArecentlypublishedstudyreportedperformances achieved by 205 insulin-treatedformulas for IGR (300/TDD), CF (1,500/TDD),patients (47.6% with type 1 diabetes and 52.4%with type 2 diabetes) who were asked, based onand total basal insulin dosage [TBD 0.2 9weight (kg)], which gives a slightly higherscenarios of high or normal glucose test resultsestimate for bolus insulin and a lower estimatefor TBD [23]. The factors, IGR, CF, tBGL, andprovided by control solutions, to manuallycalculate mealtime doses of short-actingIOB, should be continuously tailored by theinsulin, followed by the same calculationusing a glucose meter with a built-in ABC [29].HCP for each patient.One may easily understand that even well-Two cohorts of patients, either carbohydrateeducated and motivated patients will inevitablyconsider these calculations time consumingcounters (n 101) whosophisticated formula, orwith, on a long-term basis, the risk of mistakeswhen dealing with so many variables clusteredcounters (n 104) who were using a simplifiedformula, were considered for the study. Thein this equation. In reality, a significantresults showed that 63% of doses calculatedmanually by the participants were erroneous,proportion of people with diabetes deal withlow literacy and low numeracy skills, whichwere using anoncarbohydratewhereas only 6% of incorrect responses wereoften results in misinterpretation of therecorded information, wrong therapeuticrecorded when calculations were performedwith an ABC. Eighty-three percent of subjectsdecisions, and low therapeutic compliance,felt confident about using the ABC and 87%preferred the automated method to the manualthereby precluding correct metabolic control[24–27]. Thus, one way diabetes devicecalculation. The study was not designed tomanufacturers sought to facilitate the processof therapeutic decisions was to incorporate anevaluate the direct impact of ABCs onmetabolic control, as the testing was based onABC into insulin pumps and BGMs. BGMs withcontrol solution values, not on actual bloodtests [29].built-in ABCs are mainly designed for MDItreated patients, as insulin pump users alreadyThese results are in line with several previoushave calculators integrated into their pump.These ‘‘smart’’ BGMs are also conceived tostudies that showed only a small proportion ofpeople with diabetes able to adequatelyprovide an electronic log book and to storecalculate insulin doses, while taking intoaccount glucose load and BG levels. This mayinformation regarding insulin intake, foodconsumption, physical activity, and healthinformation. They are sometimes engineeredexplain the low level of treatment complianceand therapeutic inertia over the long duration123
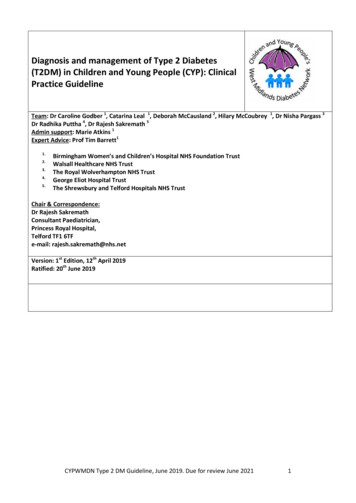
Diabetes Ther (2013) 4:1–114of diabetes [24, 30, 31]. These data are alsosoftware loaded into a personal data assistant.reminiscent of those from a 2008 study thatIn this group of 123 MDI-treated adult subjectsdemonstrated a benefit of using an ABC in apediatric population of CSII-treated patients,with type 1 diabetes, there was an improvementin glycemic control, but no change in insulinboth in terms of personal satisfaction andimproved preprandial and 2-h postprandial BGdose and no weight gain over a 12-monthperiod [36]. In addition, a higher proportionlevels [32]. In one older study [31], anof ABC users reached HbA1c values\7.5%, whileimprovementintreatmentsatisfaction,adherence, and quality of life was shown in 83remaining within target limit BG levels(70–150 mg/dL). Quite recently, a prospectiveadolescents using MDI or CSII. Another studywith 49 CSII-treated patients [33] reportedstudy performed over a period of 1 year where30 type 1 diabetic patients were asked to use anbetter postprandial BG excursions and goodABC, showed a significant decrease in diurnalconfidence in the doses advised by the device(Table 1 [29, 31–33]).glucose variability (P\0.005), and improvedHbA1c (P 0.007) and postprandial BGDo BGMs with Built-In ABCs Help(P\0.05)values.Thefrequencyhypoglycemia was not increased [37].to Improve Metabolic Controlin Insulin-Treated Patients?ofIn a small study (n 18) published in 2008comparing ABC users to nonusers, improvedmetabolic control did not occur [34]. AlthoughA recent study showed a significantimprovement in HbA1c values after a 6-monthmean postprandial BG levels in the ABC userswere significantly lowered compared tofollow-up in 40 consecutive MDI-treated type 1diabetes patients using an ABC, comparednonusers, HbA1c values were not significantlyimproved [38]. Noteworthy, this was anto standard methods (-0.85% vs. l study, not a randomized study.improvement in metabolic control was furtherFurthermore, the decision whether to use theABC or not was left to the patient’s discretion.confirmed in a recent Danish study thatreported, after 16 weeks, improved metabolicTwo other quite recent studies in CSII-treatedyoung type 1 diabetic patients reached the samecontrol (HbA1c -0.7%) and treatmentsatisfaction in a study group of MDI-treatedconclusion. There was an improvement in 2-hpatients (called the CarbCountABC arm) thatpostprandial BG levels and glucose variability,but no significant improvement of HbA1c valuesreceived a 3-h educational program, flexibleintensive insulin therapy (FIIT) and an ABC as[39, 40]. The discrepancies between thesestudies can be understood consideringcompared to a group that only received FIITeducation (HbA1c -0.1%) [35]. The patients indifferences in study design and duration(Table 2 [34–40]).the CarbCountABC arm also experienced lessglycemic variability than those in the controlgroup and spent more time in the normal BGAre There Other Advantages to UsingBGMs with Built-In ABCs?range. They also needed less insulin due to moreappropriate dosing and less correction ofAnother relevant advantage of using an ABC,hyperglycemia. The results are in line withbesides easier bolus calculation and the likelythose reported in a study of insulin guidanceimprovement in metabolic control, or at least in123
Diabetes Ther (2013) 4:1–115Table 1 Impact of an ABC on patient satisfaction and quality of lifeReferences Study designObjectivesResultsSussmanMulticenter study comparinget al. [29] manual versus ABC-assistedcalculations of insulin dosesEvaluation of error frequencywhen insulin dosagescalculated either manually orwith an ABCSignificant reduction of errors whendoses calculated with an ABC(P\0.001)205 MDI-treated patients47.6% type 1 diabetes; 52.4% type2 diabetes; 104 non-CC; 101 CCImproved confidence and preferenceof using an ABC (P\0.0001)Increased adherence may optimize theuse of meal-time insulinGlaser12-month randomized control trial Impact of an ABC on metabolic Higher rate of calculation errors withet al. [31] comparing an IDC device tocontrolconventional methodsconventional methods for insulindoses83 MDI- or CSII-treated type 1diabetes adolescentsImpact of an ABC ontreatment satisfaction,regimen adherence, andquality of lifeShashaj2-week crossover study comparing Improvement of pre- andet al. [32] an ABC (Bolus Wizard) topostprandial glycemic controlconventional methods for insulindoses36 CSII-treated type 1 diabetesadolescentsTreatment satisfactionGross et al. 7-day crossover study comparing an Improvement of postprandial[33]ABC to conventional methodsBG levelsfor insulin doses49 CSII-treated type 1 diabetessubjectsImprovement in treatmentsatisfaction, adherence, and qualityof life among ABC usersNo change in HbA1c among ABCusersSignificant reduction in pre- and 2-hpostprandial BG levels and in thenumber of correction boluses(P\0.05)Higher satisfaction level among ABCusersLess correction boluses to controlpostprandial hyperglycemia whenusing the ABC (P\0.05)Less supplemental glucose to raise lowBG levels when using the ABC(P\0.05)Decreased average deviation of 2-hpostprandial BG levelsABC easy to use and confidence inadvised insulin dosesABC automated bolus calculator, BG blood glucose, CC carbohydrate counters, CSII continuous subcutaneous insulininfusion, HbA1c glycated hemoglobin, IDC insulin dosage calculation, MDI multiple daily injectionglucose variability, is the reduction in fear andrate of hypoglycemia. This was shown in atype 1 diabetes patients, of which 588 respondedpositively [41]. The vast majority of themrecent study that surveyed 1,412 MDI-treated(76.7%) claimed to use the ABC quite often or123
Diabetes Ther (2013) 4:1–116Table 2 Impact of an ABC on HbA1c valuesReferencesStudy designObjectivesResultsMaurizi et al.[34]3- to 6-month randomized trial comparing patientsusing an ABC to a control groupEffect of an ABC onmetabolic control at 3and 6 monthsAt 3 months: nonsignificant improvementin HbA1c levels (-0.61%)40 consecutive adult type 1 diabetes patientsAt 6 months: significant improvement inHbA1c levels (-0.85%; P \ 0.05)Schmidt et al.[35] (TheBolusCalstudy)16-week randomized, controlled, open-label, three-armparallel trialEffect of FIIT and anABC on metaboliccontrolSignificant improvement of HbA1c in thearm of CarbCountABC (P \ 0.0001)51 adult MDI-treated type 1 diabetes patientsEffect of FIIT and anABC on treatmentsatisfactionSignificant improvement in treatmentsatisfaction (DTSQs and DTSQc) inthe arm of CarbCountABC(P \ 0.001)Garg et al. [36]1-year open-label, randomized, controlled trialImprovement of HbA1cvaluesHbA1c improvement by [0.6% at12 months (P \ 0.02)123 adult type 1 diabetes patients randomized on a 1:1basis to either an ABC or control groupHigher proportion of ABC usersachieving HbA1c \7.5% (P \ 0.01)Within-target values higher among ABCusersWithout weight gain or changes in insulindosagesMore severe hypoglycemia among ABCusers (P 0.04)Lepore et al.[37]1-year prospective observation studyImprovement of HbA1cvaluesSignificant improvement in HbA1c(P \ 0.007)Significant improvement of postprandialBG levels (P \ 0.05)30 CSII-treated type 1 diabetes patients already trainedto CH counting and ISF and invited to use aninsulin pump with an ABCSignificant improvement of daily glucosevariability (P \ 0.005)Improved aptitude to calculate properdose of insulin bolusNo increased frequency of hypoglycemiaKlupa et al.[38]Observational study18 CSII-treated type 1 diabetes patientsImprovement of HbA1cvalues when using anABC (in an insulinpump)No significant improvement in HbA1cvaluesSignificant decrease in 2-h postprandialvalues (P \ 0.05)Enander et al.[39]1-year multicenter study involving 40 CSII-treatedtype 1 diabetes patients in three arms: control, CC,CC plus ABC (in an insulin pump)Improvement in HbA1clevels and in mealrelated BG levelsNo difference in HbA1c valuesBłazik andPańkowska[40]3-month randomized, open-label studyChanges in HbA1c,postprandial glucose andglucose variabilityNo change in HbA1c values48 CSII-treated type 1 diabetic children randomlyallocated to a group using diabetics software, and acontrol group using caloric tables and mentalcalculationsDecreased BG levels fluctuations andincrease in postmeal BG levels withintarget (P 0.014)Significant decrease in 2-h postprandialBG levels and in glucose variabilityparameters (P \ 0.05)ABC automated bolus calculator, BG blood glucose, CC carbohydrate counters, CSII continuous subcutaneous insulin infusion, DTSQc and DTSQsdiabetes treatment satisfaction questionnaires (change and status versions, respectively), FIIT flexible intensive insulin therapy, HbA1c glycatedhemoglobin, IDC insulin dosage calculation, ISF insulin sensitivity factor, MDI multiple daily injectionalways. In 52% of respondents, the fear ofhypoglycemia was reduced and most of themdose calculation. In addition, 89.3% reported thatbolus calculation was made easy or very easy(78.8%) reported a high confidence in the insulinwhen the bolus advisor was used. Although123
Diabetes Ther (2013) 4:1–117reduced fear of hypoglycemia is not a parameterare also papers reporting worsened quality ofsystematically reported in the literature, most oflife among patients using the SMBG method.the studies point out patient satisfaction and theimproved confidence in insulin dosage whenOf note, these studies were performed with type2 diabetes patients who reported increasedusing an ABC. One may therefore presume thatthe number of patients who skip insulin dosagesanxiety and depression, and even obsessivebehaviour [43–47]. These feelings were oftenor commit calculation errors is likely to be lowerassociated with HCPs lack of interest to activelyamong those using an ABC compared to thosewithout. It is also more likely that ABC users arecheck and use SMBG results that were otherwisecarefully collected by patients. This highlightsmore prone to follow insulin titrationinstructions, which are key in maintainingthe pivotal educational role of HCPs about theimportance they bring to the interpretation ofadequate metabolic control over time.SMBG results. From this view point, there is littleEven though data are contradictory abouthypoglycemic events, with at least one studydoubt that improved quality of life and patientempowerment resulting from an increasedreporting more severe hypoglycemia amongABC users [36], a recent study by Bergenstalcapability to use structured SMBG data andtranslate it into appropriate therapeuticet al. [42], where an insulin support decisiondecisions are two hallmarks of BGMs with built-algorithm was tested both in subjects with type1 and type 2 diabetes, rather supports the ideain ABCs. HCPs in combination with an ABC caneducate patients to interpret SMBG values andthat the frequency of hypoglycemia is loweramong patients using an ABC. Thus, lessmake appropriate therapeutic decisions to meetmetabolic targets. Patients must deal with anhypoglycemic episodes occurred in the groupsusing the algorithm despite the higher rate ofoverload of variables such as BG levels, ICR,glucose intake, target values, IOB, and physicalinsulin adjustment. Another important piece ofactivity before making insulin dose decisions.information brought forward by this paper isrelated to the fact that besides subjects withWhen correctly implemented and tailored toeach patient, the main advantage of an ABC is totype 1 diabetes, two groups of subjects with type2 diabetes (treated either with basal–bolusprovide appropriate means to quickly make dailydecisions, which may contribute to a reductiontherapy or twice-daily biphasic insulin) alsoinappeared to show benefit from the computerdecision system. This indicates that smart BGMsinstability. The literature reveals that BGMswith built-in ABCs are used more often andshould not be reserved only for subjects withtype 1 diabetes, but rather offered to all MDI-with increased confidence by patients, whichcould be viewed as a real advantage, especially fortreated patients, regardless of the type ofthose who are confronted to low numeracy and/diabetes (Table 3 [41, 42]).or low literacy issues. One may reasonablysuppose that, because of improved metabolicDISCUSSIONhypoglycemicincreases awareness of diabetes, as well aspatient’s empowerment and reassurance, thereandmetabolicperformances and quality of life, the increasinguse of BGMs with built-in ABCs may result inreducedAlthough a consensus is emerging that SMBGeventsrisksoflongtermmicro-andmacrovascular complications. This medicalimprovement may of course have positiveeconomic consequences because of long-term123
Diabetes Ther (2013) 4:1–118Table 3 Impact of an ABC on hypoglycemiaReferences Study designObjectivesResultsBarnardSurvey of 588 MDI-treated type 1et al. [41] diabetic patients using an ABCReduced fear ofhypoglycemiaMild or significant reduction in fear ofhypoglycemia in 52% of respondentsPrognosis of patients toachieve improvedglycemic controlImprovement or significantimprovement in the confidence inthe insulin dose calculation in 78.8%of respondentsBolus calculation made easy or veryeasy by the ABC in 89.3% ofrespondentsBergenstal 12-week intervention period (testing the Primary: fraction ofImprovement in average BG levelset al. [42] Diabetes Insulin Guidance systemsoftware dosage(P\0.03)following a 4-week baseline run-inadjustment approved byperiodthe study team20 MDI-treated CC type 1 diabetesSecondary: improvedpatients, 20 MDI-treated non-CC type glycemic control2 diabetes patients, and six twice-dailybiphasic-treated type 2 diabetespatientsImprovement in mean HbA1c(P\0.03)Reduction by 25.2% of hypoglycemicevents (P 0.02)ABC automated bolus calculator, CC carbohydrate counters, BG blood glucose, HbA1c glycated hemoglobin, MDI multipledaily injectionimproved HbA1c and a reduced rate of diabetescomplications [13].treated patients who already have strong skillsto calculate bolus manually. This is the price toTo be efficacious, smart BGMs that arepay for them to really understand and criticallyexpected to increase patient adherence to BGmonitoring, should be used by patients whoreview dosage recommendations proposed bythe software. According to the principle thatform a cohesive team with caregivers. It is ofcourse important that all patients understandnothing is definitively fixed in the life ofpatients and that everything may changethe relevance of SMBG and how to use it.overtime, the customization of the deviceNoteworthy, this should be done while alwaysquestioning the suggestions delivered by themustbesupervisedmachine. For instance, a BGM cannot exemptthe patient to always predict changes in theexplaining to patients what to do withrecorded data. Thus, the key aspect for aphysical activity or diet habits in the hourssuccessful use of a smart BGM is education.that follow the injection of insulin. Otherparameters, such as concurrent illnesses andRegular assessments must be foreseen to makesure that recommendations provided by thespecial medications (e.g., corticoids), must alsobe taken into account. For all of these reasons,system are done in a safe way and always inclose connection with the patient needs. AsABC devices should be proposed to insulin-long as the principle of ongoing education is123continuouslyproposedby HCPs who shouldandkeep
Diabetes Ther (2013) 4:1–11kept in mind, one may expect that using an9CONCLUSIONautomated decision support algorithm willbring a great relief to patients, especially tothose who are carbohydrate counters, becausethey must deal with more difficult math thanthose treated with fixed doses of insulineventually corrected by CF.The reduced risk of hypoglycemia iscertainly another relevant advantage of BGMswith built-in ABCs. The fear of hypoglycemia,just as a low level of education, often precludesBGMs with an embarked ABC are effectivemotivational tools that should be consideredmore than just gadgets. They do bring a realvalue in patient empowerment that is nowconsidered essential in diabetes management.But this statement remains pertinent as long asthe principle of ongoing education and thetight cohesion with the HCPs team arepreserved.the ability of patients to make changes and is asource of therapeutic inertia. Hypoglycemia isone of the main causes of alteration of thepatient’s quality of life. The ongoing technicalimprovements and, for instance, the recentprogresses in telemedicine should make usmore confident in the ability of supportdecision software to alert patients in real timeabout hypoglycemia [48]. This is of coursecrucial as, most of the time, actual systems donot warn enough patients about hypoglycemiaand about the importance of managing itACKNOWLEDGMENTSThis article was reviewed by Abbott for scientificaccuracy before submission. Dr. Colin is theguarantorforthisarticle,andtakesresponsibility for the integrity of the work as awhole.Conflict of interest. Allnothing to disclose.authorshavebefore injecting the next dose of insulin. Inaddition, they should also encourage patientsto inject insulin as soon as BG levels are gettingback to normal, a requirement that is oftenneglected by patients when recovering fromhypoglycemia.Decision softwares were initially designed tohelp patients dealing with doses of short- orrapid-acting insulin. Unfortunately, fastingvalues, that are also known to influence HbA1cvalues [49], are not yet included enough in thecalculation process. It should be easy formanufacturers to propose ABC devices able toOpen Access. This article is distributedunder the terms of the Creative CommonsAttribution Noncommercial License whichpermits any noncommercial use, distribution,and reproduction in any medium, provided theoriginal author(s) and the source are credited.REFERENCES1.UK Prospective Diabetes Study (UKPDS) eas or insulin compared withconventional treatment and risk of complicationsin patients with type 2 diabetes (UKPDS 33). Lancet.1998;352:837–53 (Erratum in: Lancet. 1999;354:602).2.Diabetes Control and Complications Trial (DCCT)Research Group. The effect of intensive treatmentof diabetes on the development and progression ofcounsel doses of long-acting insulin based onfew days of fasting BG levels. Positive ornegative trends in relation with chosen targetvalues would then be recorded and translatedinto suggestions to increase or decrease thedosages of basal insulin.123
Diabetes Ther (2013) 4:1–1110long-term complications in insulin-dependentdiabetes mellitus. N Engl J Med. 1993;329:977–86.3.4.5.Diabetes Control and Complications Trial (DCCT)Research Group. The relationship of glycemicexposure (HbA1c) to the risk of development andprogression of retinopathy in the diabetes controland complications trial. Diabetes. 1995;44:968–83.Nathan DM, Cleary PA, Backlund JY, et al. DiabetesControl and Complications Trial/Epidemiology ofDiabetes Interventions and Complications (DCCT/EDIC) Study Research Group: intensive diabetestreatment and cardiovascular disease in patientswith type 1 diabetes. N Engl J Med. 2005;353:2643–53.14. Goldstein DE, Little RR, Lorenz RA, Malone JI,Nathan DM, American Diabetes Association. Testsof glycemia in diabetes. Diabetes Care. 2004;27(Suppl 1):S91–3.15. Blonde L. SMBG and glycemic control: examining theevidence. Medscape website. http://www.medscape.org/viewarticle/532933 2. Accessed 4 Oct 2012.16. American Diabetes Association. Standards formedical care in diabetes. Diabetes Care.2011;35(Suppl 1):S11–63.17. Demidowich AP, Lu K, Tamler R, Bloomgarden Z.An evaluation of diabetes self-managementapplications for Android smartphones. J TelemedTelecare. 2012;18:235–8.Gaede P, Lund-Andersen H, Parving HH, PedersenO. Effect of a multifactorial intervention onmortality in type 2 diabetes. N Engl J Med.2008;358:580–91.18. Walsh J, Roberts R, Bailey T. Guidelines for optimalbolus calculator settings in adults. J Diabetes SciTechnol. 2011;5:129–35.6.Holman RR, Paul SK, Bethel MA, Matthews DR, NeilHA. 10-year follow-up of intensive glucose controlin type 2 diabetes. N Engl J Med. 2008;359:1577–89.19. Bloomgarden ZT. Inpatient diabetes control:approaches to treatment. Diabetes Care. 2004;27:2272–7.7.Saydah SH, Fradkin J, Cowie CC. Poor control ofrisk factors for vascular disease among adults withpreviously diagnosed diabetes. JAMA. 2004;291:335–42.20. Kawamura T. The importance of carbohydratecounting in the treatment of children withdiabetes. Pediatr Diabetes. 2007;8(Suppl 6):57–62.8.Strowig SM, Raskin P. Improved glycemic control inintensively treated type 1 diabetic patients usingblood glucose meters with storage capability andcomputer-assisted analyses. Diabetes Care. 1998;21:1694–8.9.Levine BS, Anderson BJ, Butler DA, Antisdel JE,Brackett J, Laffel LMB. Predictors of glycemiccontrol and
short-acting insulin dose, at least three-times daily. Patients are supposed to calculate their insulin dose based on the following formula: Insulin dosage ðU) ¼ glucose load ðgÞ IGR þ ðaBGLÞð tBGLÞ CF ½ IOB Insulin dosage is expressed in units (U). The first part of the equation corresponds to a division between the glucose load and the