Transcription
2017 ProviderHandbookMagellan Complete Care of FloridaMAGELLAN COMPLETE CARE800-327-8613www.MCCofFL.com
Table of ContentsAbout Magellan Complete Care. . . . . . . . . . . . . . . .Model of Care. . . . . . . . . . . . . . . . . . . . . . . . . . . . .Continuity of Care and Transition of CareRequirements. . . . . . . . . . . . . . . . . . . . . . . . . . . . .Provider Services . . . . . . . . . . . . . . . . . . . . . . . . .Statewide Medicaid Managed Care Program . .Magellan Complete Care ParticipationRequirements . . . . . . . . . . . . . . . . . . . . . . . . . . . .333445Contact Telephone Numbers . . . . . . . . . . . . . . . . . . 6Member Eligibility and ID Card. . . . . . . . . . . . . . . . 7PCP Responsibilities. . . . . . . . . . . . . . . . . . . . . . . . .Coordination of Care . . . . . . . . . . . . . . . . . . . . . .Access and Availability. . . . . . . . . . . . . . . . . . . . .Referrals. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Provision of Assessment and CounselingServices. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .88889Provider Responsibilities (including PCPs). . . . . . 10Pregnancy. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10Access and Availability. . . . . . . . . . . . . . . . . . . . . 10Claims Submission. . . . . . . . . . . . . . . . . . . . . . . . 11Medical Records . . . . . . . . . . . . . . . . . . . . . . . . . . 11Network Development . . . . . . . . . . . . . . . . . . . . 12Credentialing. . . . . . . . . . . . . . . . . . . . . . . . . . . . 12Appealing Decisions That Affect NetworkParticipation Status . . . . . . . . . . . . . . . . . . . . . . 12Quality. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13Retrospective/Post Service Review Process. . . 14Grievances and Appeals. . . . . . . . . . . . . . . . . . . . 14Balance Billing. . . . . . . . . . . . . . . . . . . . . . . . . . . . 14Provision of Assessment and CounselingServices. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14Newborn Hearing Screening. . . . . . . . . . . . . . . 15Identifying and Reporting Abuse, Neglect, orExploitation. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15Marketing/Community Outreach Activities . . . 16Risk Management and Adverse/Critical IncidentReporting. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17Adverse and Critical Incident Reports. . . . . . . . 17 Fraud, Waste and Abuse Responsibilities . . . . . . 19Definitions—Fraud, Waste and Abuse. . . . . . . 19Report Suspected Fraud, Waste or Abuse. . . . 21Presence on Federal and State Exclusions List. . 22Cultural Competency Plan. . . . . . . . . . . . . . . . . . . 24Member Rights and Responsibilities. . . . . . . . . . . 25Provider Complaints . . . . . . . . . . . . . . . . . . . . . . . . 27Provider Complaint Process. . . . . . . . . . . . . . . 29External Claims Dispute Process. . . . . . . . . . . 29Member Grievance and Appeals . . . . . . . . . . . . . . 30Medicaid Fair Hearing . . . . . . . . . . . . . . . . . . . . . 31Subscriber Assistance Program . . . . . . . . . . . . . 31Medical Management. . . . . . . . . . . . . . . . . . . . . . . .Medical Necessity Standards . . . . . . . . . . . . . .Treatment Adherence . . . . . . . . . . . . . . . . . . . .Mental Health and Substance AbuseAssessments. . . . . . . . . . . . . . . . . . . . . . . . . . . . .Continuity of Care. . . . . . . . . . . . . . . . . . . . . . . .Prior Authorization . . . . . . . . . . . . . . . . . . . . . .Covered Services. . . . . . . . . . . . . . . . . . . . . . . . . . .Expanded Services. . . . . . . . . . . . . . . . . . . . . . . . .Additional Notes for Covered Services . . . . . .Subcontractors and Inter-company Partnerswith Magellan Complete Care. . . . . . . . . . . . . .Waived Copayments & Fees. . . . . . . . . . . . . . . .Second Medical Opinion . . . . . . . . . . . . . . . . . .Emergency Services. . . . . . . . . . . . . . . . . . . . . .Emergency Ambulance Services. . . . . . . . . . . .OB Ultrasound Authorizations . . . . . . . . . . . . .Out of Area Emergency Services . . . . . . . . . . .Emergency Room Prudent LaypersonFacility Reviews . . . . . . . . . . . . . . . . . . . . . . . . .Child Health Check-Up/Vaccines . . . . . . . . . . .Telemedicine . . . . . . . . . . . . . . . . . . . . . . . . . . . .Community Referrals. . . . . . . . . . . . . . . . . . . . .32323233333335363840414141424242434445461
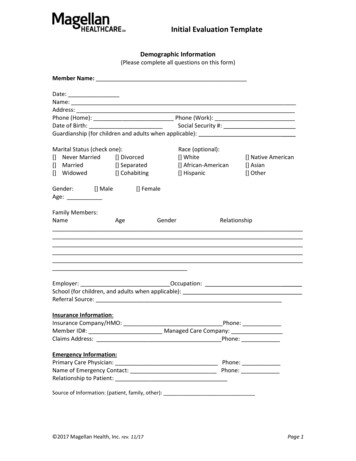
Covered Pharmacy Services. . . . . . . . . . . . . . . . . .Pharmacy Policy. . . . . . . . . . . . . . . . . . . . . . . . .Prior Authorization. . . . . . . . . . . . . . . . . . . . . . .Over-the-Counter Items. . . . . . . . . . . . . . . . . . .72-hour Emergency Supply Policy. . . . . . . . . . .Newly Approved Products. . . . . . . . . . . . . . . . .474747484848Healthcare Advance Directives. . . . . . . . . . . . . . . 56The Patient’s Right to Decide. . . . . . . . . . . . . . . 56Questions About Healthcare AdvanceDirectives. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56More Information On Healthcare AdvanceDirectives. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58Care and Disease Management Programs. . . . . . 49Helpful Forms. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60Adult Health Assessment. . . . . . . . . . . . . . . . . . . 61Child Health Assessment. . . . . . . . . . . . . . . . . . 65Grievance Form. . . . . . . . . . . . . . . . . . . . . . . . . . 69Appeals Form. . . . . . . . . . . . . . . . . . . . . . . . . . . . 71Florida WIC Program Medical Referral. . . . . . 73Florida Department of Health WICProgram Medical Documentation forFormula and Food. . . . . . . . . . . . . . . . . . . . . . . . 75Living Will . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 77Designation of Healthcare Surrogate. . . . . . . . 79Uniform Donor Form . . . . . . . . . . . . . . . . . . . . . . 81Healthcare Advance Directives. . . . . . . . . . . . . 83Quality Benefit Enhancement Programs . . . . . . . 49Member Rewards Program. . . . . . . . . . . . . . . . . . . 50Continuity of Care Procedures Upon ProviderTermination. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50Medical Records Standards. . . . . . . . . . . . . . . . . . . 51Medical Record Retrieval. . . . . . . . . . . . . . . . . . 52Medical Record Confidentiality. . . . . . . . . . . . . 52Medical Record Review . . . . . . . . . . . . . . . . . . . 52Claims and Encounter Submission Protocols(clean claims). . . . . . . . . . . . . . . . . . . . . . . . . . . . 52Other Insurance. . . . . . . . . . . . . . . . . . . . . . . . . . . .Filing claims and payment. . . . . . . . . . . . . . . . .Encounter Data. . . . . . . . . . . . . . . . . . . . . . . . . .Provider Portal . . . . . . . . . . . . . . . . . . . . . . . . . .Protocols for Submitting Claims andEncounters. . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Preferred Drug List . . . . . . . . . . . . . . . . . . . . . .Supporting Efforts to Connect withMembers. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2 54545455555555
About Magellan Complete CareMagellan Complete Care is an integratedwhole health plan designed for the total care ofindividuals including medical and behavioralhealth needs. Our clinical and operational modelof care allows us to offer our members access tohigh-quality, clinically appropriate, affordablehealthcare, tailored to each individual’s needs toultimately improve healthcare outcomes and theoverall quality of life for our members and theirfamilies.with a Serious Mental Illness (SMI). Our membersare both eligible for Medicaid and have beendiagnosed with a Serious Mental Illness.Magellan Complete Care is a division of MagellanHealth Services, a healthcare managementcompany that focuses on fast-growing, complexand high-cost areas of healthcare, with anemphasis on special population management.Continuity of Careand Transition of CareRequirementsModel of CareOur providers are the key to our success inmeeting the needs of our members. Our modelis built to meet the medical and behavioralhealthcare needs of our members. The levelof support and coordination is dependent onthe needs of the individual members. Our CareCoordination Team (CCT) deploys a broad setof tools, resources and reports. The CCT iscomprised of the member and/or designatedrepresentative, primary and specialist treatingproviders, an Magellan Complete Care IntegratedCare Case Manager with both behavioral andphysical health clinical expertise, peer supportspecialists, and a Health Guide. The Health Guidehelps the member navigate through the physicaland behavioral health delivery systems andensures that the member receives all necessarybehavioral and physical health services in order tolive independently in the community.Magellan Complete Care is a Medicaid specialtyplan as part of the Statewide Medicaid ManagedCare program specializing in the care of those Magellan Complete Care brings the samecommitment to the provider community thatwe have for the last 25-years. Together, we canleverage our strength, experience and expertise toimprove outcomes for Medicaid recipients in ourcommunity.Magellan Complete Care and the other approvedhealth plans will be following special proceduresduring the transition period. The transition periodis defined as the first sixty (60) calendar days fromthe date of the member’s enrollment. Magellanworks with in and out of network providers toassure the following: If the new member is receiving care which wasprior authorized by the last health plan, or themember has ongoing treatment or medications,MCC will pay for those services without anyform of authorization even if the providers orthe pharmacy are not in our network. Members can continue to see their PCP andbehavioral health provider until the new PCPand BH providers have reviewed and updatedthe member’s treatment plan (which should bewithin 60 days). An outreach program for all members using anyhistorical claims and service authorization dataprovided by the State or previous health plans.We will use the data to identify and prioritizemembers who are at high risk if their behavioralor physical care is disrupted.3
If our member experiences a problem findingproviders or getting an appointment, our careworkers, health guides, and other staff willtrouble-shoot in real time.Provider ServicesOur Provider Support Representatives arecommitted to our providers and work to establisha positive experience with Magellan CompleteCare including: Provide orientation to Magellan Complete Care Provide education and support to facilitate bestpractices and cultural competency Assist with strategies related to thedevelopment and management of the MagellanComplete Care provider network Support the processes that lead to resolutionof operational short-falls (e.g. claims paymentissues) Implement provider practice-based qualityinitiatives—(e.g. patient registries, P4Pprograms, provider scorecards) Distribute and review various MagellanComplete Care reportsStatewide Medicaid ManagedCare ProgramMedicaid is the medical assistance program thatprovides access to healthcare for low-incomefamilies and individuals. Medicaid also assistsaged, blind and disabled people with the costs ofnursing facility care and other medical expenses.Eligibility for Medicaid is usually based on thefamily’s or individual’s income and assets.Florida has offered Medicaid services since 1970.Medicaid provides healthcare coverage for eligiblechildren, seniors, disabled adults and pregnantwomen. It is funded by both the state and federalgovernments. The 2011 Florida Legislature passedHouse Bill 7107 (creating part IV of Chapter 409,F.S.) to establish the Florida Medicaid programas a statewide, integrated managed care programfor all covered services, including long-term careservices. This program is referred to as statewideMedicaid managed care (SMMC) and includes twoprograms: one for medical assistance (MMA) andone for long-term care (LTC).The Agency for Healthcare Administration (AHCA)is responsible for administering the StatewideMedicaid Managed Care program. MagellanComplete Care is a participating specialty plan inthe Statewide Medicaid Managed Care program.Additional information regarding coverageand reimbursement can be found in the AHCAMedicaid handbooks and fee schedules. Thisinformation is available at www.fdhc.state.fl.us/medicaid/index.shtml.4
Magellan Complete CareParticipation RequirementsAll participating providers with MagellanComplete Care must have a unique FloridaMedicaid Identification Number, along with aNational Provider Identification Number (NPI)and be credentialed by Magellan Complete Care.Magellan Complete Care does not employ orcontract with individuals on the state or federalexclusions list.Magellan Complete Care’s Network Developmentdepartment ensures that all services and tasksrelated to the provider contract are performedin compliance with the terms of the ProviderAgreement. The provider contract identifies anyaspect of service that may be subcontracted by theprovider.In this event, the background screen will bea Level II screen in accordance with Agencypolicies for providers not currently enrolled inthe Medicaid fee-for-service program. This screenwill require providers to submit fingerprintselectronically through the Agency’s system, allowMagellan to exclude from contracting any providerwho has a record of illegal conduct, and permitMagellan to receive verification of Medicaideligibility through the background screeningwebsite. Providers who have completed abackground screen through the Medicaid programor, within the last 12 months, by another Floridadepartment are exempt from this requirement.In general, Magellan Complete Care only contractswith participating providers in the Medicaid feefor-service program. Thus, a Level II backgroundscreening is performed through this program.Background screening is conducted by MagellanComplete Care in the event that other providersare contracted. 5
Contact Telephone NumbersIn order to assist you with your day-to-day operations, Magellan Complete Care has a team of experiencedCustomer Service, Provider Relations, Health Services and Pharmacy professionals to assist you with ourplan. Please contact us whenever you need assistance.DepartmentHours (M – F unless noted)TelephoneProvider ServicesPharmacy BenefitsClaimsNetwork Development (Contracting)CredentialingComplaints8 a.m. to 7 p.m. ET800-327-8613800-424-1694 TTY onlyCheck Member Eligibility24 hours a day800-327-8613800-424-1694 TTY onlyPrior Authorizations and ReferralsHealth Services (Utilization Management)24 hours a day800-327-8613800-424-1694 TTY onlyNurse Line24 hours a day800-327-8613800-424-1694 TTY only8 a.m. to 7 p.m. ET800-327-8613800-424-1694 TTY onlyReservation line: 8 a.m. to 5 p.m. ETTransportation assistance for triprecovery and after hour dischargesis available 24/7/365800-424-8268Provider ContactsMember ContactsCustomer ServiceBehavioral Health ServicesCondition Care ProgramsGrievances and AppealsVendor ContactsNon-Emergent Transportation (Veyo)Dental Services (DentaQuest)800-964-7811Routine and preventive vision (Florida Eye Care)9 a.m. to 5 p.m. EST877-481-3322Routine and preventive vision (Premiere Eye)24 hours a day800-738-1889Hearing Evaluations (HearUSA)8 a.m. to 8 p.m., voice mail afterhours800-528-32778:00am to 5:00pm ET866-762-2237State ContactsFL Department of Children and Families6
Member Eligibility and ID CardMagellan Complete Care requires that ourmembers keep their ID card with them at all times.If a member loses their ID card, please have themcontact Customer Service toll free at 800-327-8613.If they’re hearing impaired, call toll free at800-424-1694 TTY. Magellan Complete Care willsend them a replacement ID card within 5business days.Please remember that a member ID card is nota guarantee of payment for services rendered.The provider’s office is responsible for verifyingeligibility at the time of each office visit. Theprovider can access the following methods toverify eligibility: Call 24-hour Eligibility Line at 800-327-8613 Online at MCCofFL.comID Card front:7600 Corporate Drive, Suite 600Miami FL, 33126MagellanCompleteCareofFL.comback:Customer Service, Claims/Billing, and Transportation:1-800-327-8613 (Monday – Friday 8 a.m. – 7 p.m. EST)If you are hearing impaired, call our TTY number at 1-800-424-1694Emergency Services: Seek treatment at the nearest emergency room orurgent care center or call 911. Notify your doctor and the health planwithin 48 hours or as soon as possible if you are admitted to the hospital.Member Name: xxxMEMBERNAMExxxMember #:xxMEMBERNBR-xxGroup:xxxxxEnrollment Date:xx/xx/xxxxAuthorizations/Eligibility (Participating and Non-Participating Providers):1-800-327-8613Mail Claims to:Magellan Complete CarePO Box 2097Maryland Heights, MO 63043Payor ID#: 01260Utilize Medicaid Participating PharmaciesBIN #: 016523 PCN #: 622 RxGroup: XXXXXXX Possession of an ID card does not guarantee eligibility orpayment for services provided.7
PCP ResponsibilitiesWith the support of the Magellan Complete Care’sCore Care team, the primary care provider (PCP)is responsible for the overall care of the member.This includes providing direct care, referringmembers for behavioral health, specialty orancillary care and coordinating care with thehealth plan and these providers for greater clinicaloutcomes.Coordination of Care Coordinator of Care: The PCP is thecoordinator of care. Therefore, the PCP agreesto ensure continuity of care for MagellanComplete Care’s members and arranges for theprovision of services when the PCP’s office isnot open. The PCP integrated medical recordshould include documentation of the member’scare, and the treatment plan, includingdocumentation of ER visits, lab results, hospitaldischarge summaries or operative reports. Sharing of Information: The PCP agrees tofacilitate adequate and timely communicationamong providers and the transfer ofinformation when members are transferred toother healthcare providers. Agency Communication: The PCP agrees tomaintain communication with the appropriateagencies such as local police, social servicesagencies and poison control centers to providequality care. OB/GYN as PCP: Each female member mayselect as her primary physician an obstetrician/gynecologist who has agreed to serve as aprimary physician and is in the MagellanComplete Care network. Please call MagellanComplete Care at 800-327-8613 if a membermakes this request.8 Access and Availability Member Panel: The PCP agrees to maintain aratio of members to full time equivalent (FTE)physicians as follows: One physician shall not exceed a MagellanComplete Care member panel of 1,500;each physician extender (ARNP or PA) mayincrease panel size by 750 patients. The PCP must certify to Magellan CompleteCare whether or not their active memberpanel exceeds 3,000 across all plansduring the application and re-credentialingprocess.ReferralsConsistent with our model of care, MagellanComplete Care has established a referral policywhich promotes care coordination, integration,and access. We do not require in-network referralsto be approved by the health plan; however,provider’s records are expected to includeevidence that care has been coordinated amongthe member’s treating providers.Specifically, primary care providers should referthe member for specialty care and send theirNPI number, clinical records and other relevantinformation to the specialist at the time of thereferral, in advance of the appointment. Specialistsare expected to provide a written report to theprimary care provider after seeing the member. AllMagellan Complete Care providers are expectedto maintain medical records which reflect thiscoordination. If coordination is oral, the providers’records should include documentation of thecommunication.
We require specialists to include the primarycare provider’s NPI number in field 17b on claimsfor office-based services. Exceptions to thisrequirement include: Provider is in the same provider group, or hasthe same tax ID or type II NPI as the referringphysician. Services were provided after hours (99050) Emergency services (services performed inplace of service 23) Obstetrics/gynecology claims Billing or referring physician is from any of thefollowing: Federally Qualified Health Center Urgent Care Center County Health DepartmentsProvision of Assessment andCounseling Services Initial Assessment: The PCP must conduct ahealth assessment of all new members within90 days of the effective date of enrollment.The PCP is responsible for notifying MagellanComplete Care if unable to contact the memberto arrange the initial assessment with 90 days. Members Entering Protective Custody: ThePCP agrees to physically screen members takeninto the Protective Custody, Emergency Shelteror Foster Care programs by the Department ofChildren and Families (DCF) within 72 hours orimmediately, if required. Self-referrals—Members may self-refer forcertain services, including: Family planning services Annual eye exams by optometrist Some chiropractic, podiatric, anddermatologic services Well-woman examinations Behavioral health servicesFor these excluded services, Magellan CompleteCare requests your assistance in communicatingand coordinating the care of members. However,we pay for direct-access services withoutcompletion of field 17b.If medically necessary care cannot be providedby in-network providers, care can be provided byan out-of-network provider. In these exceptionalcases, Magellan Complete Care requires priorauthorization by the health plan. 9
Provider Responsibilities(including PCPs)Pregnancy Pregnancy Identification: The provider isresponsible for notifying Magellan CompleteCare’s Health Services team when they identifya pregnant member at 800-327-8613. If faxed,the notification should include the member’sname, ID number, and due date. Referrals to Healthy Start and WIC: Theprovider agrees to refer pregnant women orinfants to Healthy Start and WIC programs. HIV Counseling for Pregnant Women: Theprovider agrees to provide counseling and offerthe recommended anti-retroviral regimen toall pregnant women who are HIV-positive andto refer them and their infants to Healthy Startprograms, regardless of their screening scores. Hepatitis B Screening for Pregnant Women:The provider agrees to offer screening forHepatitis B surface antigen to all womenreceiving prenatal care. If they test positive,the provider agrees to refer them to HealthyStart regardless of their screening score and toprovide Hepatitis B Immune Globulin and theHepatitis B vaccine series to children born tosuch mothers.Access and Availability 24-Hour Coverage: All providers must provide24 hours a day/seven days a week coverageand regular hours of operation must be clearlydefined and communicated to the members,including arranging for on-call and after-hourscoverage. Such coverage must consist of ananswering service, call forwarding, providercall coverage or other customary meansapproved by Magellan Complete Care per AHCA10 guidelines. The after-hours coverage must beaccessible using the medical office’s daytimetelephone number and the call must be returnedwithin 30 minutes of the initial contact. Coverage During Absence: The providermust arrange for coverage of services duringabsences due to vacation, illness, or othersituations that require the provider to be unableto provide services. A Magellan Complete Careparticipating provider must provide coverage. Appointment Wait Time Requirement: Theprovider offers appointments to our memberswithin the timeframes outlined below. Pleaseensure office staff is aware of and follows thesestandards. Magellan Complete Care audits itsproviders on a routine basis to ensure that youroffices are compliant with this policy. Urgent Care—within one day Routine Sick Patient Care—within one week Well Care Visit—within one month Timely Medical Evaluation: The provider willensure that all patients have a professionalevaluation within one hour of their scheduledappointment time. If a delay is unavoidable,the patient will be informed and provided analternative. Americans with Disability Act: The provideragrees to establish appropriate policies andprocedures to fulfill obligations under theAmericans with Disabilities Act (ADA).
Claims Submission To ensure timely payment, participatingproviders must submit clean claims and/orencounters using the methodology establishedby AHCA for that provider and service except asoutlined in this manual. This also ensures thatthe required Magellan Complete Care encounterdata will be accepted by the Florida MMIS and/or the State’s encounter data warehouse. The provider agrees to submit a claim orencounter using the correct codes for eachpreventative visit. These claims provide thedocumentation needed for gaps in care for ourmembers and for HEDIS (Health Plan EmployerData and Information Set) service.Medical Records Participation in Medical Record Sharing:The provider must adhere to MagellanComplete Care release of medical recordspolicy to facilitate the sharing of medicalrecords (subject to applicable confidentialityrequirements in accordance with 42 CFR, Part431, Subpart F, including a minor’s consultation,examination and drugs for STDs in accordancewith Section 384.30 (2), F.S.). Confidentiality of Member Records: Theprovider must comply with all applicable federaland state laws regarding the confidentiality ofmember records. Release of Information on SensitiveConditions: Release of information aboutprotected and sensitive conditions and services,including psychotherapeutic services, requiresspecific release from the member prior tosharing with other providers. The MagellanComplete Care Authorization to Use andDisclose Protected Health Information (AUD)form is used to indicate the conditions forwhich release is permitted. This form can befound at MagellanCompleteCareofFL.com. Notations for Clinical Research: The provideragrees that any notation in a member’s clinicalrecord indicating diagnostic or therapeuticintervention as part of clinical research will beclearly contrasted with entries regarding theprovision of non-research related care. Sharing of Immunization Information: Theprovider agrees to provide immunizationinformation to the DCF upon receipt ofmember’s written permission and DCF’srequest for members requesting temporary cashassistance from the DCF. Obtaining Records from Out-of-NetworkProviders: The provider agrees to attemptto obtain medical records on any member(s)receiving services from a non-network providerusing the proper release signed by the member. See Medical Records section for additionalinformation. Release of Medical Records: The provideragrees to obtain a signed and dated releaseallowing for the release of information toMagellan Complete Care and other providersinvolved in the member’s care. 11
Network Development New Provider in Group Practice: If a newprovider is added to a group, MagellanComplete Care must approve and credential theprovider before the provider may treat membersunless a prior authorization has been approved.Notification of changes in the provider staff isthe responsibility of the provider’s office andmust be communicated to Magellan CompleteCare Network Development in writing to thefollowing address:Network Management Contract AdministrationFlorida MHS, Inc.14100 Magellan PlazaMaryland Heights, MO 63043 Malpractice Insurance: The provider isrequired to maintain malpractice insuranceacceptable to Magellan Complete Care. Thisinformation is verified by obtaining a copyof the malpractice insurance fact sheetfrom the provider or from the malpracticeinsurance carrier. If the provider does notcarry malpractice insurance (“going bare”),the provider must conform to the notificationrequirements contained in Section 458.320, F.S.CredentialingProviders are required to successfully completethe Mage
Medicaid Identification Number, along with a National Provider Identification Number (NPI) and be credentialed by Magellan Complete Care . . Dental Services (DentaQuest) 800-964-7811 Routine and preventive vision (Florida Eye Care) 9 a.m. to 5 p.m. EST 877-481-3322