Transcription
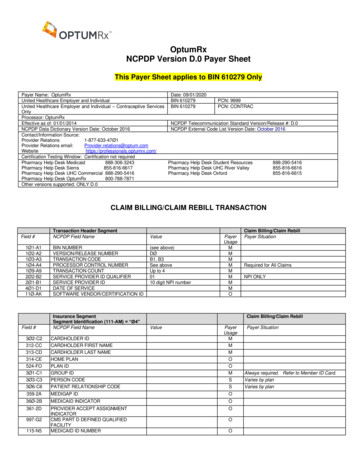
Magellan Rx ManagementNCPDP D.0 Payer SpecificationsJuly 24, 2020**Start of Request Claim Billing/Claim Re-Bill (B1/B3) Payer Sheet**General InformationPayer Name: Magellan Rx ManagementPlan Name/Group Name: Magellan Health EmployeesBIN: 017035PCN: 605Plan Name/Group Name: MRx Commercial – CBA BlueBIN: 017449PCN: CBGPlan Name/Group Name: MRx Commercial – Legacy Partners RxClientsBIN: 015243PCN: PRX1000Plan Name/Group Name: MRx Commercial – Lucent Technologies BIN: 017465PCN: LUCENTPlan Name/Group Name: MRx Commercial – StandardBIN: 017449PCN: 6792000Plan Name/Group Name: MRx Commercial – Employee BenefitManagement ServicesBIN: 017431PCN: EBMSPlan Name/Group Name: FlexScriptsBIN: 017472PCN: FLEXRXPlan Name/Group Name: MRx Commercial – UnionBIN: 017449PCN: UNIONPayer Name: Magellan Rx ManagementDate: July 1, 2017Plan Name/Group Name: MRx Commercial – Cash CardBIN: 018679PCN: 6775000 GRP: 040116Plan Name/Group Name: Yale UniversityBIN: 017449PCN: YALEGRP: PRXYALProcessor: Magellan Rx ManagementEffective as of: 08/01/2014NCPDP Telecommunication Standard Version/Release #: D.0NCPDP Data Dictionary Version Date: In accordancewith NCPDP Version StandardsNCPDP External Code List Version Date: In accordance withNCPDP Version StandardsContact/Information Source: www.magellanrx.comCertification Testing Window: TBDCertification Contact Information: 804-548-0130Provider Relations Help Desk Info: 800-424-3312Other versions supported: No other versions supportedProprietary & Confidential 2014–2020 Magellan Health, Inc. All rights reserved.
Other Transactions SupportedPayer: Please list each transaction supported with the segments, fields, and pertinent informationon each transaction.Transaction CodeE1Transaction NameEligibility TransactionField Legend for ColumnsPayer Usage ColumnValuePayer SituationColumnExplanationMANDATORYMThe Field is mandatory for the Segment in the designatedTransaction.NoREQUIREDRThe Field has been designated with the situation of“Required” for the Segment in the designated Transaction.No“Required when.” The situations designated havequalifications for usage (“Required if x,” “Not required if y”).YesQUALIFIED REQUIREMENTRWFields that are not used in the Claim Billing/Claim Re-bill transactions and those that do not havequalified requirements (i.e., not used) for this payer are excluded from the template.Claim Billing/Claim Re-bill TransactionThe following lists the segments and fields in a Claim Billing or Claim Re-bill Transaction for theNCPDP Telecommunication Standard Implementation Guide Version D.Ø.Transaction Header Segment QuestionsClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentXSource of certification IDs required inSoftware Vendor/Certification ID (11Ø-AK) isPayer IssuedXRequired when vendor certification isrequired by Magellan Rx Management –otherwise submit all zeroesSource of certification IDs required inSoftware Vendor/Certification ID (11Ø-AK) isSwitch/VAN issuedSource of certification IDs required inSoftware Vendor/Certification ID (11Ø-AK) isNot usedTransaction Header SegmentField #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsage1Ø1-A1BIN NUMBERSee aboveM1Ø2-A2VERSION/RELEASE NUMBERDØMPage 2 MRx Payer NCPDP D.0 Payer SpecificationsPayer Situation
Transaction Header SegmentField #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsage1Ø3-A3TRANSACTION CODEB1, B3M1Ø4-A4PROCESSOR CONTROLNUMBERSee aboveM1Ø9-A9TRANSACTION COUNTUp to 4M2Ø2-B2SERVICE PROVIDER IDQUALIFIER01M2Ø1-B1SERVICE PROVIDER IDM4Ø1-D1DATE OF SERVICEM11Ø-AKSOFTWAREVENDOR/CERTIFICATION IDMInsurance Segment QuestionsThis Segment is always sentNCPDP Field NameRequired for all claimsNPI of submitting pharmacyproviderRequired when vendor certificationis required by Magellan RxManagement – otherwise submit allzeroesClaim Billing/Claim Re-billIf Situational, Payer SituationCheckXInsurance SegmentSegment Identification (111-AM) “Ø4”Field #Payer SituationClaim Billing/Claim Re-billValuePayerUsage3Ø2-C2CARDHOLDER IDM312-CCCARDHOLDER FIRST NAMER313-CDCARDHOLDER LAST NAMER3Ø9-C9ELIGIBILITY CLARIFICATIONCODERWPayer SituationImp Guide: Required if needed forreceiver inquiry validation and/ordetermination, when eligibility isnot maintained at the dependentlevel. Required in special situationsas defined by the code to clarify theeligibility of an individual, whichmay extend coverage.Payer Requirement: Same as ImpGuide3Ø1-C1GROUP ID3Ø3-C3PERSON CODERRWSee ID card.Imp Guide: Required if needed touniquely identify the familymembers within the Cardholder ID.MRx Payer NCPDP D.0 Payer Specifications Page 3
Insurance SegmentSegment Identification (111-AM) “Ø4”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationPayer Requirement: Same as ImpGuide3Ø6-C6PATIENT RELATIONSHIPCODERWImp Guide: Required if needed touniquely identify the relationship ofthe Patient to the Cardholder.Payer Requirement: Same as ImpGuidePatient Segment QuestionsThis Segment is always sentClaim Billing/Claim Re-billIf Situational, Payer SituationCheckXThis Segment is situationalPatient SegmentSegment Identification (111-AM) “Ø1”Field331-CXNCPDP Field NameClaim Billing/Claim Re-billValuePATIENT ID QUALIFIERPayerUsageRWPayer SituationImp Guide: Required if Patient ID(332-CY) is used.Payer Requirement: Same as ImpGuide332-CYPATIENT IDRWImp Guide: Required if necessary forstate/federal/regulatory agencyprograms to validate dual eligibility.Payer Requirement: Same as ImpGuide3Ø4-C4DATE OF BIRTHR3Ø5-C5PATIENT GENDER CODER31Ø-CAPATIENT FIRST NAMER311-CBPATIENT LAST NAMER3Ø7-C7PLACE OF SERVICERWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement: Same as ImpGuide333-CZEMPLOYER IDRWImp Guide: Required if “required bylaw” as defined in the HIPAA finalPrivacy regulations section 164.5Ø1definitions (45 CFR Parts 16Ø andPage 4 MRx Payer NCPDP D.0 Payer Specifications
Patient SegmentSegment Identification (111-AM) “Ø1”FieldNCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer Situation164 Standards for Privacy ofIndividually Identifiable HealthInformation; Final Rule Thursday, December 28, 2000, page82803 and following, andWednesday, August 14, 2002, page53267 and following.)Required if needed for Workers’Compensation billing.Payer Requirement: Same as ImpGuide335-2CPREGNANCY INDICATORRWImp Guide: Required if pregnancycould result in different coverage,pricing, or patient financialresponsibility.Required if “required by law” asdefined in the HIPAA final Privacyregulations section 164.5Ø1definitions (45 CFR Parts 16Ø and164 Standards for Privacy ofIndividuallyIdentifiable Health Information;Final RuleThursday, December 28, 2000, page82803 and following, andWednesday, August 14, 2002, page53267 and following.)Payer Requirement: Same as ImpGuide384-4XPATIENT RESIDENCERWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement: Same as ImpGuideClaim Segment QuestionsCheckThis Segment is always sentXThis payer supports partial fillsXClaim Billing/Claim Re-billIf Situational, Payer SituationThis payer does not support partial fillsMRx Payer NCPDP D.0 Payer Specifications Page 5
Claim SegmentSegment Identification (111-AM) “Ø7”Field #455-EMNCPDP Field NamePRESCRIPTION/SERVICEREFERENCE NUMBERQUALIFIERClaim Billing/Claim Re-billValue1 Rx BillingPayerUsagePayer SituationMImp Guide: For Transaction Code of“B1,” in the Claim Segment, thePrescription/Service ReferenceNumber Qualifier (455-EM) is “1”(Rx Billing).4Ø2-D2PRESCRIPTION/SERVICEREFERENCE NUMBERM436-E1PRODUCT/SERVICE IDQUALIFIERM4Ø7-D7PRODUCT/SERVICE IDM456-ENASSOCIATEDPRESCRIPTION/SERVICEREFERENCE NUMBERRWImp Guide: Required if the“completion” transaction in a partialfill (Dispensing Status (343-HD) “C” (Completed)).Required if the Dispensing Status(343-HD) “P” (Partial Fill) andthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide457-EPASSOCIATEDPRESCRIPTION/SERVICE DATERWImp Guide: Required if the“completion” transaction in a partialfill (Dispensing Status (343-HD) “C” (Completed)).Required if AssociatedPrescription/Service ReferenceNumber (456-EN) is used.Required if the Dispensing Status(343-HD) “P” (Partial Fill) andthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide458-SEPROCEDURE MODIFIER CODE Maximum count of 1Ø.COUNTRWImp Guide: Required if ProcedureModifier Code (459-ER) is used.Payer Requirement: Same as ImpGuidePage 6 MRx Payer NCPDP D.0 Payer Specifications
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field Name459-ERPROCEDURE MODIFIER CODEClaim Billing/Claim Re-billValuePayerUsageRWPayer SituationImp Guide: Required to define afurther level of specificity if theProduct/Service ID (4Ø7-D7)indicated a Procedure Code wassubmitted.Required if this field could result indifferent coverage, pricing, orpatient financial responsibility.Payer Requirement: Same as ImpGuide442-E7QUANTITY DISPENSED460-ETQUANTITY PRESCRIBEDRRWImp Guide: Required when atransmission is for a Scheduled IIdrug as defined in 21 CFR 1308.12and per CMS-0055-F (ComplianceDate 09/21/2020. Refer to theVersion D.0 Editorial Document).4Ø3-D3FILL NUMBERR4Ø5-D5DAYS SUPPLYR4Ø6-D6COMPOUND CODER4Ø8-D8DISPENSE AS WRITTEN(DAW)/PRODUCT SELECTIONCODER414-DEDATE PRESCRIPTIONWRITTENR415-DFNUMBER OF REFILLSAUTHORIZEDR419-DJPRESCRIPTION ORIGIN CODER354-NXSUBMISSION CLARIFICATIONCODE COUNTMaximum count of 3.RWImp Guide: Required if SubmissionClarification Code (42Ø-DK) is used.Payer Requirement: Same as ImpGuide42Ø-DK SUBMISSION CLARIFICATIONCODERWImp Guide: Required if clarificationis needed and value submitted isgreater than zero (Ø). If used forHIV PrEP indicator, enter value of“10” for 0.00 co-pay and SCC of “1”for a non-HIV PrEP indicator forACA Plans only.MRx Payer NCPDP D.0 Payer Specifications Page 7
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationPayer Requirement: Same as ImpGuide3Ø8-C8OTHER COVERAGE CODERWImp Guide: Required if needed byreceiver, to communicate asummation of other coverageinformation that has been collectedfrom other payers.Required for Coordination ofBenefits.Payer Requirement: Values accepted00, 01, 02, 03, 04, and 08. See ECLfor value definitionPayer Requirement: Same as ImpGuide429-DT454-EKSPECIAL PACKAGINGINDICATORRWSCHEDULED PRESCRIPTIONID NUMBERRWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Imp Guide: Required if necessary forstate/federal/regulatory agencyprograms.Payer Requirement: Follow Stateregulatory guidance for productsthat require a scheduled prescriptionID number.6ØØ-28UNIT OF MEASURER418-DILEVEL OF SERVICERWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement: Same as ImpGuide461-EUPRIOR AUTHORIZATION TYPECODERWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement: Same as ImpGuide462-EVPage 8PRIOR AUTHORIZATIONNUMBER SUBMITTED MRx Payer NCPDP D.0 Payer SpecificationsRWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationPayer Requirement: Same as ImpGuide343-HDDISPENSING STATUSRWImp Guide: Required for the partialfill or the completion fill of aprescription.Payer Requirement: Same as ImpGuide344-HFQUANTITY INTENDED TO BEDISPENSEDRWImp Guide: Required for the partialfill or the completion fill of aprescription.Payer Requirement: Same as ImpGuide345-HGDAYS SUPPLY INTENDED TOBE DISPENSEDRWImp Guide: Required for the partialfill or the completion fill of aprescription.Payer Requirement: Same as ImpGuide357-NVDELAY REASON CODERWImp Guide: Required when neededto specify the reason that submissionof the transaction has been delayed.Payer Requirement: Same as ImpGuide391-MTPATIENT ASSIGNMENTINDICATOR (DIRECT MEMBERREIMBURSEMENTINDICATOR)RWImp Guide: Required when theclaims adjudicator does not assumethe patient assigned his/her benefitsto the provider or when the claimsadjudicator supports a patientdetermination of whether he/shewants to assign or retain his/herbenefits.Payer Requirement: Same as ImpGuide995-E2ROUTE OF ADMINISTRATIONRWImp Guide: Required if specified intrading partner agreement.Payer Requirement: REQUIREDWHEN SUBMITTING COMPOUNDCLAIMS996-G1COMPOUND TYPERWImp Guide: Required if specified intrading partner agreement.MRx Payer NCPDP D.0 Payer Specifications Page 9
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationPayer Requirement: REQUIREDWHEN KNOWN FOR COMPOUNDPREPARATION147-U7PHARMACY SERVICE TYPERWImp Guide: Required when thesubmitter must clarify the type ofservices being performed as acondition for proper reimbursementby the payer.Payer Requirement: Same as ImpGuidePricing Segment QuestionsThis Segment is always sentXPricing SegmentSegment Identification (111-AM) “11”Field #NCPDP Field Name4Ø9-D9INGREDIENT COSTSUBMITTED412-DCDISPENSING FEE SUBMITTEDClaim Billing/Claim Re-billIf Situational, Payer SituationCheckClaim Billing/Claim Re-billValuePayerUsagePayer SituationRRWImp Guide: Required if its valuehas an effect on the Gross AmountDue (43Ø-DU) calculation.Payer Requirement: Same as ImpGuide438-E3INCENTIVE AMOUNTSUBMITTEDRWImp Guide: Required if its valuehas an effect on the Gross AmountDue (43Ø-DU) calculation.Payer Requirement: Same as ImpGuide478-H7OTHER AMOUNT CLAIMEDSUBMITTED COUNTMaximum count of 3.RWImp Guide: Required if OtherAmount Claimed SubmittedQualifier (479-H8) is used.Payer Requirement: Same as ImpGuide479-H8OTHER AMOUNT CLAIMEDSUBMITTED QUALIFIERRWImp Guide: Required if OtherAmount Claimed Submitted (48ØH9) is used.Payer Requirement: Same as ImpGuidePage 10 MRx Payer NCPDP D.0 Payer Specifications
Pricing SegmentSegment Identification (111-AM) “11”Field #48Ø-H9NCPDP Field NameOTHER AMOUNT CLAIMEDSUBMITTEDClaim Billing/Claim Re-billValuePayerUsageRWPayer SituationImp Guide: Required if its valuehas an effect on the Gross AmountDue (43Ø-DU) calculation.Payer Requirement: Same as ImpGuide481-HAFLAT SALES TAX AMOUNTSUBMITTEDRWImp Guide: Required if its valuehas an effect on the Gross AmountDue (43Ø-DU) calculation.Payer Requirement: Same as ImpGuide482-GEPERCENTAGE SALES TAXAMOUNT SUBMITTEDRWImp Guide: Required if its valuehas an effect on the Gross AmountDue (43Ø-DU) calculation.Payer Requirement: Same as ImpGuide483-HEPERCENTAGE SALES TAXRATE SUBMITTEDRWImp Guide: Required if PercentageSales Tax Amount Submitted (482GE) and Percentage Sales TaxBasis Submitted (484-JE) are used.Required if this field could result indifferent pricing.Required if needed to calculatePercentage Sales Tax Amount Paid(559-AX).Payer Requirement: Same as ImpGuide484-JEPERCENTAGE SALES TAXBASIS SUBMITTEDRWImp Guide: Required if PercentageSales Tax Amount Submitted (482GE) and Percentage Sales Tax RateSubmitted (483-HE) are used.Required if this field could result indifferent pricing.Required if needed to calculatePercentage Sales Tax Amount Paid(559-AX).Payer Requirement: Same as ImpGuide426-DQUSUAL AND CUSTOMARYCHARGE43Ø-DU GROSS AMOUNT DUERImp Guide: Required if needed pertrading partner agreement.RMRx Payer NCPDP D.0 Payer Specifications Page 11
Pricing SegmentSegment Identification (111-AM) “11”Field #423-DNNCPDP Field NameClaim Billing/Claim Re-billValueBASIS OF COSTDETERMINATIONPharmacy Provider Segment QuestionsPayerUsagePayer SituationRClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXPharmacy Provider SegmentSegment Identification (111-AM) “Ø2”Field #465-EYNCPDP Field NameRequired only if law or regulation required.Claim Billing/Claim Re-billValuePROVIDER ID QUALIFIERPayerUsagePayer SituationRWImp Guide: Required if Provider ID(444-E9) is used.444-E9PROVIDER IDRWImp Guide: Required if necessaryfor state/federal/regulatory agencyprograms.Required if necessary to identifythe individual responsible fordispensing of the prescription.Required if needed forreconciliation of encounter-reporteddata or encounter reporting.Payer Requirement: REQUIREDONLY IF LAW OR REGULATIONREQUIREDPrescriber Segment QuestionsThis Segment is always sentClaim Billing/Claim Re-billIf Situational, Payer SituationCheckXThis Segment is situationalPrescriber SegmentSegment Identification (111-AM) “Ø3”Field #466-EZNCPDP Field NameClaim Billing/Claim Re-billValuePRESCRIBER ID QUALIFIERPayerUsageRWPayer SituationImp Guide: Required if PrescriberID (411-DB) is used.Payer Requirement: (any uniquepayer requirement(s))Page 12 MRx Payer NCPDP D.0 Payer Specifications
Prescriber SegmentSegment Identification (111-AM) “Ø3”Field #411-DBNCPDP Field NameClaim Billing/Claim Re-billValuePRESCRIBER IDPayerUsageRWPayer SituationImp Guide: Required if this fieldcould result in different coverage orpatient financial responsibility.Required if necessary forstate/federal/regulatory agencyprograms.Payer Requirement: (any uniquepayer requirement(s))427-DRPRESCRIBER LAST NAMERWImp Guide: Required when thePrescriber ID (411-DB) is notknown.Required if needed for PrescriberID (411-DB)validation/clarification.Coordination of Benefits/Other PaymentsSegment QuestionsCheckClaim Billing/Claim Re-billIf Situational, Payer SituationThis Segment is always sentThis Segment is situationalXRequired only for secondary, tertiary, etcclaims.Scenario 1 – Other Payer Amount PaidRepetitions OnlyXOCC codes 00, 01, 02, 03, 04 Supported.Scenario 2 – Other Payer-PatientResponsibility Amount Repetitions andBenefit Stage Repetitions OnlyXOCC codes 08 Supported.Scenario 3 – Other Payer Amount Paid, OtherPayer-Patient Responsibility Amount, andBenefit Stage Repetitions Present(Government Programs)If the Payer supports the Coordination of Benefits/Other Payments Segment, only one scenariomethod shown above may be supported per template. The template shows the Coordination ofBenefits/Other Payments Segment that must be used for each scenario method. The Payer mustchoose the appropriate scenario method with the segment chart, and delete the other scenariomethods with their segment charts. See section Coordination of Benefits (COB) Processing formore information.MRx Payer NCPDP D.0 Payer Specifications Page 13
Coordination of Benefits/Other PaymentsSegmentSegment Identification (111-AM) “Ø5”Field #NCPDP Field Name337-4CCOORDINATION OFBENEFITS/OTHER PAYMENTSCOUNT338-5COTHER PAYER COVERAGETYPE339-6COTHER PAYER ID QUALIFIERClaim Billing/Claim Re-billScenario 1 – Other Payer Amount Paid Repetitions OnlyValueMaximum count of 9.PayerUsagePayer SituationMMRWImp Guide: Required if Other PayerID (34Ø-7C) is used.Payer Requirement: Same as ImpGuide34Ø-7COTHER PAYER IDRWImp Guide: Required ifidentification of the Other Payer isnecessary for claim/encounteradjudication.Payer Requirement: Same as ImpGuide443-E8OTHER PAYER DATERWImp Guide: Required ifidentification of the Other PayerDate is necessary forclaim/encounter adjudication.Payer Requirement: Same as ImpGuide341-HBOTHER PAYER AMOUNT PAIDCOUNTMaximum count of 9.RWImp Guide: Required if Other PayerAmount Paid Qualifier (342-HC) isused.Payer Requirement: Same as ImpGuide342-HCOTHER PAYER AMOUNT PAIDQUALIFIERRWImp Guide: Required if Other PayerAmount Paid (431-DV) is used.Payer Requirement: Same as ImpGuide. See program providerrequirements.Page 14 MRx Payer NCPDP D.0 Payer Specifications
Coordination of Benefits/Other PaymentsSegmentSegment Identification (111-AM) “Ø5”Field #431-DVNCPDP Field NameClaim Billing/Claim Re-billScenario 1 – Other Payer Amount Paid Repetitions OnlyValueOTHER PAYER AMOUNT PAIDPayerUsagePayer SituationRWImp Guide: Required if other payerhas approved payment for some/allof the billing.Not used for patient financialresponsibility only billing.Not used for non-governmentalagency programs if Other PayerPatient Responsibility Amount(352-NQ) is submitted.Payer Requirement: Same as ImpGuide471-5EOTHER PAYER REJECT COUNT Maximum count of 5.RWImp Guide: Required if Other PayerReject Code (472-6E) is used.Payer Requirement: Same as ImpGuide472-6EOTHER PAYER REJECT CODERWImp Guide: Required when theother payer has denied thepayment for the billing.Payer Requirement: Same as ImpGuideCoordination of Benefits/Other PaymentsSegmentSegment Identification (111-AM) “Ø5”Field #NCPDP Field Name337-4C COORDINATION OFBENEFITS/OTHER PAYMENTSCOUNT338-5C OTHER PAYER COVERAGE TYPEClaim BillingScenario 2 – Other Payer – Patient Responsibility Amount (OPPRA)Repetitions OnlyValueMaximum count of 9Payer UsagePayer SituationMM339-6C OTHER PAYER ID QUALIFIERRWRequired if Other Payer ID(34Ø-7C) is used.34Ø-7C OTHER PAYER IDRWRequired if identification of theOther Payer is necessary forclaim/encounter adjudication.443-E8 OTHER PAYER DATERWRequired if identification of theOther Payer Date is necessaryfor claim/encounteradjudication.MRx Payer NCPDP D.0 Payer Specifications Page 15
Coordination of Benefits/Other PaymentsSegmentSegment Identification (111-AM) “Ø5”Field #Claim BillingScenario 2 – Other Payer – Patient Responsibility Amount (OPPRA)Repetitions OnlyNCPDP Field NameValuePayer UsagePayer Situation353-NR OTHER PAYER – PATIENTRESPONSIBILITY AMOUNTCOUNTMaximum count of 25.RRequired if Other Payer –Patient Responsibility AmountQualifier (351-NP) is used.351-NP OTHER PAYER – PATIENTRESPONSIBILITY QUALIFIERØ1 - 13RCode qualifying the “OtherPayer-Patient ResponsibilityAmount (352-NQ)352-NQ OTHER PAYER-PATIENTRESPONSIBILITY AMOUNTDUR/PPS Segment QuestionsRClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXDUR/PPS SegmentSegment Identification (111-AM) “Ø8”Field #473-7ENCPDP Field NameDUR/PPS CODE COUNTERSubmitted if required to affect outcome ofclaim related to DUR intervention.Claim Billing/Claim Re-billValueMaximum of 9occurrences.PayerUsageRWPayer SituationImp Guide: Required if DUR/PPSSegment is used.Payer Requirement: Same as ImpGuide439-E4REASON FOR SERVICE CODERWImp Guide: Required if this fieldcould result in different coverage,pricing, patient financialresponsibility, and/or drugutilization review outcome.Required if this field affectspayment for or documentation ofprofessional pharmacy service.Payer Requirement: Same as ImpGuide44Ø-E5PROFESSIONAL SERVICECODERWImp Guide: Required if this fieldcould result in different coverage,pricing, patient financialresponsibility, and/or drugutilization review outcome.Required if this field affectspayment for or documentation ofprofessional pharmacy service.Page 16 MRx Payer NCPDP D.0 Payer Specifications
DUR/PPS SegmentSegment Identification (111-AM) “Ø8”Field #NCPDP Field NameClaim Billing/Claim Re-billPayerUsageValuePayer SituationPayer Requirement: Same as ImpGuide441-E6RESULT OF SERVICE CODERWImp Guide: Required if this fieldcould result in different coverage,pricing, patient financialresponsibility, and/or drugutilization review outcome.Required if this field affectspayment for or documentation ofprofessional pharmacy service.Payer Requirement: Same as ImpGuide474-8EDUR/PPS LEVEL OF EFFORTRWImp Guide: Required if this fieldcould result in different coverage,pricing, patient financialresponsibility, and/or drugutilization review outcome.Required if this field affectspayment for or documentation ofprofessional pharmacy service.Payer Requirement: Same as ImpGuideCompound Segment QuestionsClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXCompound SegmentSegment Identification (111-AM) “1Ø”Field #NCPDP Field NameSubmitted if the claim dispensed is acompound.Claim Billing/Claim Re-billValuePayerUsage45Ø-EFCOMPOUND DOSAGE FORMDESCRIPTION CODEM451-EGCOMPOUND DISPENSINGUNIT FORM INDICATORM447-ECCOMPOUND INGREDIENTCOMPONENT COUNT488-RECOMPOUND PRODUCT IDQUALIFIERMaximum 25 ingredientsPayer SituationMMMRx Payer NCPDP D.0 Payer Specifications Page 17
Compound SegmentSegment Identification (111-AM) “1Ø”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsage489-TECOMPOUND PRODUCT IDM448-EDCOMPOUND INGREDIENTQUANTITYM449-EECOMPOUND INGREDIENTDRUG COSTRCOMPOUND INGREDIENTBASIS OF COSTDETERMINATIONR49Ø-UEClinical Segment QuestionsPayer SituationImp Guide: Required if needed forreceiver claim determination whenmultiple products are billed.Imp Guide: Required if needed forreceiver claim determination whenmultiple products are billed.Claim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXClinical SegmentSegment Identification (111-AM) “13”Field #491-VENCPDP Field NameDIAGNOSIS CODE COUNTSubmitted if the clinical detail will affect theoutcome of claims processing.Claim Billing/Claim Re-billValueMaximum count of 5.PayerUsageRWPayer SituationImp Guide: Required if DiagnosisCode Qualifier (492-WE) andDiagnosis Code (424-DO) are used.Payer Requirement: Same as ImpGuide492-WEDIAGNOSIS CODE QUALIFIERRWImp Guide: Required if DiagnosisCode (424-DO) is used.Payer Requirement: Same as ImpGuide424-DODIAGNOSIS CODERWImp Guide: Required if this fieldcould result in different coverage,pricing, patient financialresponsibility, and/or drugutilization review outcome.Required if this field affectspayment for professional pharmacyservice.Required if this information can beused in place of prior authorization.Page 18 MRx Payer NCPDP D.0 Payer Specifications
Clinical SegmentSegment Identification (111-AM) “13”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationRequired if necessary forstate/federal/regulatory agencyprograms.Payer Requirement: Same as ImpGuide**End of Request Claim Billing/Claim Re-bill (B1/B3) Payer Sheet**MRx Payer NCPDP D.0 Payer Specifications Page 19
Response Claim Billing/Claim Re-bill Payer SheetClaim Billing/Claim Re-bill Accepted/Paid (or Duplicate of Paid) Response**Start of Response Claim Billing/Claim Re-bill (B1/B3) Payer Sheet**General InformationPayer Name: Magellan Rx ManagementPlan Name/Group Name:Magellan Health EmployeesBIN:PCN:017035605Plan Name/Group Name:MRx Commercial-CBA BlueBIN:PCN:017449CBGPlan Name/Group Name:MRx Commercial-Legacy Partners Rx ClientsBIN:015243PCN:PRX1000Plan Name/Group Name:MRx Commercial-Lucent TechnologiesBIN:017465PCN:LUCENTPlan Name/Group Name:MRx-Commercial StandardBIN:017449PCN:6792000Plan Name/Group NameBINPCNMRx Commercial-Employee Benefit ManagementServices017431EBMSPlan Name/Group NameBINPCNFlexScripts017472FLEXRXClaim Billing/Claim Re-bill PAID (or Duplicate of PAID) ResponseThe following lists the segments and fields in a Claim Billing or Claim Re-bill response (Paid orDuplicate of Paid) Transaction for the NCPDP Telecommunication Standard ImplementationGuide Version D.Ø.Response Transaction Header SegmentQuestionsCheckThis Segment is always sentXClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)Response Transaction Header SegmentField #Claim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationNCPDP Field NameValuePayerUsage1Ø2-A2VERSION/RELEASE NUMBERDØM1Ø3-A3TRANSACTION CODEB1, B3M1Ø9-A9TRANSACTION COUNTSame value as in requestM5Ø1-F1HEADER RESPONSE STATUSA AcceptedMPage 20 MRx Payer NCPDP D.0 Payer SpecificationsPayer Situation
Claim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)Response Transaction Header SegmentField #NCPDP Field NameValuePayerUsage2Ø2-B2SERVICE PROVIDER IDQUALIFIERSame value as in requestM2Ø1-B1SERVICE PROVIDER IDSame value as in requestM4Ø1-D1DATE OF SERVICESame value as in requestMResponse Message Segment QuestionsCheckPayer SituationClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentThis Segment is situationalXResponse Message SegmentSegment Identification (111-AM) “2Ø”Field #5Ø4-F4NCPDP Field NameSent if additional information is availablefrom the payer/processor.Claim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)ValueMESSAGEPayerUsageRWPayer SituationImp Guide: Required if text isneeded for clarification or detail.Payer Requirement: Same as ImpGuideResponse Insurance Segment QuestionsThis Segment is always sentCheckClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationXThis Segment is situationalMRx Payer NCPDP D.0 Payer Specifications Page 21
Response Insurance SegmentSegment Identification (111-AM) “25”Field #3Ø1-C1NCPDP Field NameClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)ValueGROUP IDPayerUsageRWPayer SituationImp Guide: Required if needed toidentify the actual cardholder oremployer group, to identifyappropriate group number, whenavailable.Required to identify the actualgroup that was used when multiplegroup coverages exist.Payer Requirement: Same as ImpGuideResponse Patient Segment QuestionsThis Segment is always sentCheckClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationXThis Segment is situationalResponse Patient SegmentSegment Identification (111-AM) “29”Field #31Ø-CANCPDP Field NameClaim Billing/Claim Re-billAccepted/Paid (or Duplicate of Paid)ValuePATIENT FIRST NAMEPayerUsageRWPayer SituationImp Guide: Required if known.Payer Requirement: Same as ImpGuide311-CBPATIENT LAST NAMERWImp Guide: Required if known.Payer Requirement: Same as ImpGuide3Ø4-C4DATE OF BIRTHRWImp Guide: Required if known.Payer Requirement: Same as ImpGuideResponse Status Segmen
Plan Name/Group Name: Yale University BIN: 017449 PCN: YALE GRP: PRXYAL Processor: Magellan Rx Management . 804-548-0130 Provider Relations Help Desk Info: 800-424-3312 Other versions supported: No other versions supported. Page 2 MRx Payer NCPDP D.0 Payer Specifications