Transcription
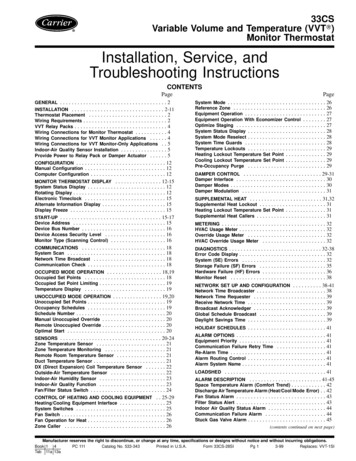
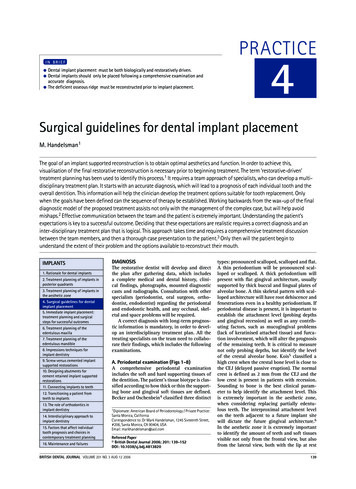
PRACTICEIN BRIEF 3The predictability of aesthetic success depends on tissue loss at the initiation oftreatment.Specific implant systems and designs do no guarantee aesthetic outcomes.Hard and soft tissue deficiencies must be addressed prior to implant placement.Recreating papilla between multiple adjacent implants is not predictable.Treatment planning of implants in theaesthetic zoneS. Jivraj1 and W. Chee2Aesthetic restoration of anterior teeth with implant supported restorations is one of the most difficult procedures to execute.Bone resorption following anterior tooth extraction often compromises gingival tissue levels for the implant restoration.In the last 10 years the focus has shifted from osseointegration, to creation of an implant borne restoration which is inharmony with the surrounding hard and soft tissue. Complete reconstruction of tooth and gingival related aestheticsremains the primary objective and in some instances can be very difficult to achieve.11. Connecting implants to teethThe predictability of aesthetic success dependson the tissue loss present at the initiation oftreatment. The greater the amount of bone andsoft tissue loss, the more difficult it becomesto produce an ideal aesthetic result. Singletooth implants have a high degree of predictability as the adjacent teeth can provide themorphological substructure that is required torestore natural gingival and papillary architecture. Replacement of multiple missing teeth inthe aesthetic zone is challenging particularlywhen the three dimensional architecture of theexisting bone and soft tissue is deficient. Thebony housing in this instance would requireaugmentation to provide a configuration thatpermits placement of implants in optimal positions which in turn would result in pleasingaesthetics. The purpose of this article is to lookat the diagnostic factors that affect the predictability of peri-implant aesthetics. Emphasis isplaced on those parameters which are criticalto overall treatment planning.12. Transitioning a patient fromteeth to implants1*Chairman, Section of Fixed Prosthodontics and Operative Dentistry,IMPLANTS1. Rationale for dental implants2. Treatment planning of implants inposterior quadrants3. Treatment planning of implantsin the aesthetic zone4. Surgical guidelines for dentalimplant placement5. Immediate implant placement:treatment planning and surgicalsteps for successful outcomes6. Treatment planning of theedentulous maxilla7. Treatment planning of theedentulous mandible8. Impressions techniques forimplant dentistry9. Screw versus cemented implantsupported restorations10. Designing abutments forcement retained implant supportedrestorations13. The role of orthodontics inimplant dentistry14. Interdisciplinary approach toimplant dentistry15. Factors that affect individualtooth prognosis and choices incontemporary treatment planning16. Maintenance and failuresUniversity of Southern California School of Dentistry / PrivateProsthodontics Practitioner, Sherman Oaks and Torrance California; 2RalphW. and Jean L. Bleak Professor of Restorative Dentistry, Director of ImplantDentistry at the University of Southern California School of Dentistry /Private Prosthodontics Practitioner, Pasadena, California*Correspondence to: Dr Sajid Jivraj, School of Dentistry, Rm. 4372 UniversityPark, University of Southern California, Los Angeles, CA 90089-0641, USAEmail: jivraj@usc.eduRefereed Paper British Dental Journal 2006; 201: 77-89DOI: 10.1038/sj.bdj.4813820BRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 20062p 77-89.indd 77Marketing enquiries have identified aesthetics as one of the major reasons why dentists usedental implants in their surgeries. If we go bythat premise it is reasonable to speculate that theaesthetic results provided with dental implantsshould be similar to the aesthetics provided withmore conventional modes of therapy such asfixed and removable partial dentures. However,achieving aesthetics with implant restorationsis significantly more challenging than that withconventional restorations. Diagnosis and appropriate treatment planning are critical in obtaining a successful outcome. Many manufacturerswill identify their systems as aesthetic; from anobjective perspective components in themselvesare not aesthetic. There is not a single component available from a manufacturer whichwould be the ideal replacement for a maxillarycentral incisor. Aesthetic outcomes are basedon many variables. It is not the specific implantdesign, surface characteristics or type of abutment that will guarantee an aesthetic result. Itis rather the time spent on data collection inreaching a correct diagnosis that pays dividendsin terms of function and aesthetics.1Root form cylindrical implants placed following surgical techniques described by Branemarket al. have proven to be a predictable methodfor anchoring replacement teeth to the jawbone.2,3 Today clinicians can prescribe the useof implants with the knowledge and confidencethat they will predictably integrate into the jaw7713/7/06 15:46:11
PRACTICEbone. The successful integration of an implant,however, is not sufficient to declare success;implants placed in poor restorative positionsresult in unaesthetic restorations that providelittle satisfaction for the clinician or the patient(Figs 1-3). The above illustrations demonstratethe complexity of implant use in aesthetic zonesand the importance of proper treatment planning prior to implant placement.Providing an aesthetic outcome requiresunderstanding of the objective and subjectivecriteria related to hard and soft tissue aesthetics.4Both dental and gingival aesthetics act togetherto provide a smile with harmony and balance.The clinician must be aware of parameters related to gingival morphology, form and dimension,characterisation, surface texture and colour5(Fig. 4). Ceramists can often produce restorations to match adjacent teeth in terms of colour,however if the surrounding tissues are not reconstructed an aesthetic outcome is not likely (Fig.5). The ultimate aim is for the implant restorationto harmonise with the frame of the smile, faceand more importantly the individual.Treatment planning must address hard andsoft tissue deficiencies and combine this withprecision in implant placement. Only with thisapproach can implant restorations be indistinguishable from the adjacent teeth (Fig. 6).Recreating what nature provided can be aformidable challenge. The physiology of woundhealing after tooth extraction creates an unfavourable soft tissue complex. The remainingmucosa often recedes palatally and apically.Often this results in a restoration that appearslong and this is compounded by the absence ofinterdental papilla (Fig. 7).The predictability of the aesthetic outcomeof an implant restoration is dependent on manyvariables including but not limited to the following:1) Patient selection and smile line2) Tooth position3) Root position of the adjacent teeth4) Biotype of the periodontium and tooth shape5) The bony anatomy of the implant site6) The position of the implant.1. Patient selection and smile linePatients who are candidates for replacementof an anterior tooth with an implant supportedrestoration must understand the benefits of animplant restoration. They must also understandthe additional length of time required for treatment and additional costs that will be incurred.The clinician must also understand the patient’sdesires. In most cases the patient’s primarydemand is an aesthetic tooth replacement; withthis in mind it is important to establish soundclinical concepts with clearly defined parameters that lead to successful aesthetics with longterm stability of the peri-implant tissues.The major indication for a single toothimplant restoration is preservation (non preparation) of one or more of the adjacent teeth(Fig. 8), and reduction in the rate of alveolar782p 77-89.indd 78resorption. Additional indications would be restoration of a missing tooth to maintain a diastema and preservation of extensive fixed restorations that are intact.A patient’s aesthetic expectations must alsobe evaluated together with their lip activity andlip length. In an average smile 75-100% of themaxillary incisors and the interproximal gingiva are displayed. In a high smile line additionalgingival tissue is exposed. Less than 75% of theincisors are exposed in a low smile line (Figs9-11).6 The clinician should be aware that thepatient who presents with unacceptable toothhealth, shade or position may not give a fullsmile when asked. Previous photographs mayaid in determining the natural position of thepatient’s lip when smiling.A high smile line poses considerable challenges when planning for implant supportedrestorations in the aesthetic zone because therestoration and gingival tissues are completelydisplayed. In these types of clinical situationsmaximal efforts towards maintaining periimplant tissue support throughout the planning,provisional, surgical and restorative phases willbe required. An article later in the series will discuss soft tissue management with provisionalrestorations.The low smile line is a less critical situationbecause the implant restoration interface whichwill be hidden behind the upper lip. Howeverthis cannot be assumed and the patient’s inputmust be sought to confirm this. ‘The aestheticzone is where the patient thinks it is.’2. Tooth positionThe tooth needs to be evaluated in three planesof space: apicocoronal, faciolingual and mesiodistal. The existing tooth position will significantly influence the presenting gingival architecture. In many instances teeth with a poorprognosis are thoughtlessly extracted. Theseteeth can significantly influence both the hardand soft tissue configuration.Apico-coronal On assessment of the apico-coronal position of the tooth it may be more apical,more coronal or ideal and mimic the level of theadjacent gingival margin (Fig. 12). Numerousauthors have shown that following extractionand insertion of an ovate pontic there is likelyto be up to 2 mm of gingival recession, and onextraction and placement of an implant immediately the migration of the gingival margin islikely to approximate 1 mm.7,8The implications this has from a practicalperspective are that if there is a hopeless toothpositioned ideally or apically and this is extracted, the gingival margin is likely to migrate apically. Restoratively, long clinical crowns, pinkporcelain or visible metal margins will result,compromising the aesthetic outcome. Theseteeth can benefit from orthodontic extrusion(Fig. 13) prior to extraction which will serve toposition the gingival level at a more harmonious level.9,10BRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 200613/7/06 15:47:06
PRACTICEFacio-lingual In this dimension the tooth position may present with different concerns. Thetooth may be positioned too far facially; thisoften results in very thin or non existent labialbone. These teeth are not good candidates fororthodontic extrusion because of inadequateunderlying bone. Extraction of these teethresults in significant vertical bone loss andcollapse of the gingival architecture. This typeof situation would benefit from bone augmentation procedures prior to implant placement. A tooth positioned more lingually wouldbenefit from the presence of an increasedamount of facial bone. This situation is morefavourable prior to extraction since the resultant discrepancy in the facial free gingival margin may be minimal.9Mesio-distal The proximity of the adjacentteeth necessary to provide proximal support andvolume of interdental papillae should be evaluated. Ideally the mesiodistal tooth width shouldbe equal to that of the contra lateral toothso that an aesthetic outcome can be achieved(Figs 14-15). Excess or deficiencies in thisdimension should be addressed through the useof orthodontics, enameloplasty or restorations.For patients with diastemas it is imperative thatthe decision to maintain or close the space bemade prior to implant placement. If the patientrefuses the above options to close the space andinsists on closing the space with the implantrestoration there is a likelihood that a black triangle may ensue. This results from inadequatesupport from the adjacent tooth to maintain thepapilla. It is important that the clinician discusses this with the patient ahead of time so disappointment with the final outcome is avoided(Figs 16-17).3. Root position of the adjacent teethPart of the diagnostic work up for patientswho need implants is a peri-apical radiograph,as often root position will preclude placing ofimplants. Many of these patients can benefitfrom orthodontics to reposition malposed teeth.If the patient illustrated in Figures 18 and 19desired implant restorations to replace congenitally missing maxillary lateral incisors, orthodontic therapy would be necessary to move theroots of the cuspid and central incisor to allowroom for ideal implant placement.Teeth with root proximity also possess verylittle interproximal bone; this thin bone createsa greater risk of lateral resorption which willdecrease the vertical bone height after extraction or implant placement. When teeth arepresent the use of orthodontics serves as a valuable adjunct to create space. This can be advantageous for support of proximal gingival architecture.11,124. Biotype of periodontium and tooth shapeThe position of the gingival tissue around atooth is determined by the connective tissueattachment and by the bone level. Two differBRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 20062p 77-89.indd 79ent periodontal biotypes have been describedin relation to the morphology of the interdental papilla and the osseous architecture: the thinscalloped periodontium and the thick flat periodontium.13The thin scalloped periodontium found inless than 15% of cases is characterised by a delicate soft tissue curtain, a scalloped underlyingosseous form and often has dehiscence and fenestrations and a reduced quantity and qualityof keratinised mucosa. Generally interproximaltissue does not completely fill the space betweenadjacent teeth. This form of gingiva reacts toinsults by receding facially and interproximally. As recession occurs and the inter-root boneresorbs, the subsequent soft tissue loss compromises the overall aesthetic result (Fig. 20).The tooth form in this type exhibits a contactpoint towards the incisal third essentially triangular anatomic crowns and contact areas ofteeth that are small facio-lingually and apicocoronally. Due to extreme taper of the roots thebone interproximally tends to be thicker.Characteristics of the soft tissue biotype willplay a prominent role in final planning for theshoulder position of the implant. A thin biotypewith highly scalloped tissue will require theimplant body and shoulder to be placed morepalatal to mask any titanium show through.When implants are placed toward the palate aslightly deeper placement is required to allowfor proper emergence profile.Combining previous factors in a patient witha high lip line and a thin biotype is extremely difficult to treat. Patients who fit into thesetreatment categories should be made aware ofthe challenges involved in obtaining an aesthetic result before treatment begins.The thick flat periodontal biotype is characterised by a denser more fibrotic soft tissue curtain, a flat thicker underlying osseous form andan increased quantity and quality of attachedkeratinised gingiva. This tissue often reactsto insults by pocket formation. Flat gingiva isassociated with a tooth form that is more bulbous. Contact areas are located more toward themiddle third of the tooth; primarily square anatomic crowns and contact areas that are widefacio-lingually and apico-coronally (Fig. 21).The tooth morphology appears to be correlated with the soft tissue quality. The triangular tooth shape is associated with the scalloped and thin periodontium. The contact areais located in the coronal third of the crownunderlining a long and thin papilla. The squareanatomic crown shape combines with a thickand flat periodontium. The contact area islocated at the middle third supporting a shortand wide papilla.Loss of interproximal tissue in the presenceof a triangular tooth form will display a widerblack triangle than in a situation when a squaretooth is present (Fig. 21). In some cases when theadjacent teeth are to be restored the crown formcan be modified prosthetically to compensatefor partial interproximal tooth loss. The contact7913/7/06 15:47:47
PRACTICEFig. 1 (left) Intra oral photographof implant in poor position angledlabially and exiting the ridge toocoronallyFig. 2 (right) Restoration fabricatedfor implant in Figure 1; note lengthof restoration compared to adjacentteethFig. 3 (left) Labial view of restorationfor implant on Figure 1 note poorshape and form of the tooth dictatedby poor implant positionFig. 4 (right) Restoration of implantsmust satisfy objective and subjectiveaesthetic criteria. There should besufficient inter-radicular space forplacement of the implant and sufficientinter-tooth distance for fabrication ofan aesthetically pleasing restorationFig. 5 (left) Note ceramics of rightcentral incisor matches that ofthe left central incisor, howeverreconstruction of the deficienthard tissue has not been achieved,resulting in a restoration that doesnot satisfy objective criteria ofaestheticsFig. 6 (right) Implant restoration onleft lateral incisor in harmony withthe existing hard and soft tissueFig. 7 (left) Wound healingfollowing extraction of a tooth canresult in apical and palatal migrationof the inter-dental papillaFig. 8 (right) A perfect indicationfor a dental implant is nonpreparation of the adjacent teethFig. 9 (left) Low smile lineFig. 10 (right) Average smile lineFig. 11 (left) High smile line.The colour and contour of therestorations and associated hard andsoft tissues becomes very visible tothe observerFig. 12 (right) The right lateralincisor has been treatment plannedfor an implant restoration. The levelof the soft tissues mimic that of thecontra lateral tooth802p 77-89.indd 80BRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 200613/7/06 15:48:12
PRACTICEFig. 13 (left) Immediate extractionof the right lateral incisor wouldresult in apical migration of thesoft tissue. Orthodontic extrusionwill allow the clinician to positionthe tissue more coronally so that onextraction there is a margin of errorFig. 14 (right) The mesio-distalwidth of the tooth requiringreplacement must equal that of thecontra lateral toothFig. 15 (left) Implant restorationreplacing the right central incisorFig. 16 (right) Excessive mesiodistalspace in the region of the toothrequiring an implant restorationFig. 17 (left) Implant restoration inthe region of the right central incisor.Note absence of interdental papilla asa result of inadequate support of thesoft tissue by the restorationFig. 18 (right) Clinical presentationof patient with congenitally missingmaxillary lateral incisors postorthodontic treatmentFig. 19 (left) Radiograph of patientin Figure 18 revealing that there isinsufficient inter radicular space forimplantsFig. 20 (right) Biotype 1periodontium; note thin andscalloped tissueFig. 21 (left) Biotype 2periodontium, not thick and flattissuesFig. 22 (right) Loss of interproximalsoft tissue in the presence of atriangular tooth form can result inunsightly black trianglesFig. 23 (left) Overcontour of theimplant provisional restoration asit emerges from the free gingivalmargin can result in apical migrationof the soft tissuesFig. 24 (right) A diagnostic waxup can highlight the deficiency ofthe hard and soft tissue and canindicate to the surgeon how muchaugmentation is requiredBRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 20062p 77-89.indd 818114/7/06 11:43:39
PRACTICEarea of the prosthetic tooth is positioned morecervically reducing the volume of the interdental space.The presenting tooth shape will also influence the implant restoration shape. The implantrestoration should mimic its contra lateral natural tooth coronal to the free gingival margin.However, apical to the free gingival margin, theimplant restoration will not be an anatomic replica. A delicate balance must be developed thatprovides adequate support of the gingival architecture yet does not provide excessive pressure.Ideally the facial contour should be slightlyflatter than the contra lateral natural tooth tominimise apical displacement of the free gingival margin after insertion (Fig. 23).145. Bony anatomy of the implant siteFor successful aesthetic restoration of implants,the bony housing must have a three dimensional configuration that permits placement ofan implant in a restoratively ideal position.15 Ifthe bony anatomy is inadequate, a bone grafting procedure may be required to enhance thesite. When these situations are encountered thepatient must be made to understand that a successful outcome will involve replacing morethan just a ‘missing tooth’. The patient must alsounderstand that the missing hard and soft tissuearchitecture will need to be rebuilt so that optimum aesthetics can be achieved.The definitive implant restoration needs to besurrounded by a hard and soft tissue environmentwhich is in harmony with the surrounding dentition. It is not only the amount of bone and soft tissue present prior to implant surgery but the precision of surgical execution which leads to an overallfavorable outcome. Several key analyses need tobe performed prior to commencing with implantplacement. A diagnostic wax up highlighting tissue deficiencies and final tooth positioning canassist in the planning process (Fig. 24).Facio-lingual ridge anatomy should be evaluated to determine if there is sufficient crestwidth to house the implant. Deficient alveolarcrest width will require a bone augmentationprocedure to allow the implant to be placedin the ideal position (Fig. 25). Clinical sounding techniques or sophisticated radiographictechniques such as tomograms or CT scans canassist in diagnosing deficiencies in this dimension (Figs 26 and 28).Mesio-distal space should be equal to that ofthe contra lateral tooth; excess or deficienciesin this dimension need to be addressed throughorthodontics, enameloplasty or restorationeither prior to or after implant placement.The most critical dimension remains theapicocoronal dimension; deficiencies in thisdimension can result from periodontal disease,trauma, atrophy and infection. Vertical graftingis complex and the site may require several surgeries to achieve an optimal configuration. Themost efficient method to evaluate this dimension is through the use of a diagnostic templatehighlighting the proposed gingival margin of822p 77-89.indd 82the implant restoration.Two anatomic structures are important indetermining predictability of soft tissues afterimplant placement. The first is the height andthickness of the facial bony wall and the secondis the bone height of the alveolar crest in theinterproximal areas.Height and thickness of facial bony wallThe position of the osseous crest is an importantpredictor for gingival levels. Kois,16 in a surveyof 100 patients, classified patients as havinghigh, normal or low crests. This was based on thevertical distance of the osseous crest to the freegingival margin. The greater the distance fromthe osseous crest to the free gingival margin thegreater the risk of tissue loss after an invasiveprocedure. Kois proposed that if the total verticaldistance of the total dentogingival complex onthe mid facial aspect is 3 mm, a slight apical lossof tissue up to 1 mm is anticipated after extraction and immediate implant placement. Greateror lesser than 3 mm indicates the change will berelatively negligible to more than 1 mm. Measuring the distance from the free gingival margin tothe osseous crest prior to extraction is an important diagnostic predictor of the anticipated finalposition of the free gingival margin.Height of bony crest in the interproximal areaThe interproximal bony crest plays a criticalrole in the presence or absence of peri-implantpapillae. A clinical study around teeth12 measured the distance from the interproximal contact to the vertical height of bone and observedhow frequently the interproximal space wouldbe filled completely by soft tissue. When thecontact point to the bone was 3-5 mm, papillaalways filled the space. When the distance was6 mm papilla was absent 45% of the time andwith a distance of 7 mm, papilla did not fill thespace 75% of the time. A difference of 1-2 mmis significant in obtaining soft tissue aesthetics.This has been confirmed with implant supported restorations.17 Kan et al.18 have also shownthat the height of peri-implant papillae in singletooth gaps is independent of the proximal bonelevel next to the implant but is dependent onthe interproximal bone height of the adjacentteeth. From a diagnostic perspective soundingfrom the tip of the papilla to the interproximalbone crest of the adjacent tooth would be animportant predictor (Figs 29-30). If this distanceis 5 mm or less there is an increased likelihoodthat the interproximal tissues will be predictably maintained following implant placementand restoration. If the distance is greater than5 mm the papilla cannot be predictably maintained after surgical intervention (Figs 30, 31).6. Implant positionAesthetic implant placement is driven by both arestorative and biological philosophy. Aesthetically the implant should be placed to satisfythe parameters of contour so that the restoration is pleasing. Biologically it should be placedBRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 200613/7/06 15:49:23
PRACTICEto allow maintenance of both hard and softtissue architecture. If the tooth to be replacedhas not yet been removed, several determinations should be made prior to the extraction.9,10Immediately placing the implant after extraction helps to shorten the treatment time andmay reduce the amount of ridge width reduction that accompanies tooth extraction. In addition, if bone deficiencies are present, orthodontic eruption of the tooth prior to extraction canhelp to increase the amount of hard and soft tissue in the future implant site.19-21The need for precision in implant placementvaries according to each individual case. Forexample, in the edentulous mandible there is needfor precision only in the facio-lingual direction.The need for precision increases in the partiallyedentulous jaws according to the teeth treatedand the positions of the neighbouring and opposing teeth. The most challenging is the anteriormaxilla where a malposition of less than a 1 mmcan jeopardise the overall treatment outcome.In most situations involving a single anteriorimplant restoration, the aesthetic considerationsare more important than functional considerations. As such axial loading is not as critical asit is with posterior implant restorations. Implantposition is critical to the final aesthetic outcomeand needs to be considered in all three dimensions and in relation to the adjacent teeth. Misalignment of the implant in the prosthetic spacecan have adverse aesthetic consequences.Apico-coronal placementApicocoronal positioning appears to be the mostcritical aspect. Deficient tissue in this dimension can result from several factors. This typeof tissue needs to be addressed during treatmentplanning. Because of the complexity of verticalhard and soft tissue grafting these patients areplaced in a high risk group.Most often tooth loss is followed by bone lossof minor or major importance. It is necessary toevaluate the discrepancy between the bone level atthe proposed implant site and the level at the adjacent teeth. Too large a difference represents a riskto both periodontal and peri-implant tissue health.Facing this, the surgeon should consider reconstructing the ridge prior to implant placement.The apico-coronal positioning of the implantis the vertical discrepancy between the occlusalsurface of the implant and the peaks of the bonysepta proximal to the adjacent teeth, the mostpleasing aesthetic result occurs when this discrepancy is minimal.To obtain appropriate apicocoronal positioning of the implant, a diagnostic wax up needs tobe completed and from this a surgical guide ismade. The emergence profile and the shape ofthe restoration are reproduced on the guide toverify the implant positioning on placement.A maxillary central incisor measures onaverage 7-8 mm mesiodistally and 6 mm faciolingually at the emergence from the soft tissue.A 4.0 mm the implant needs to be placed 3-4mm apical to the gingival margin of the contraBRITISH DENTAL JOURNAL VOLUME 201 NO. 2 JUL 22 20062p 77-89.indd 83lateral tooth to allow the restoration to emergewith a natural profile. A vertical distance of 3-4mm is needed for gradual transition from the 4mm diameter of the implant platform to the 7-8mm dimension at the gingival margin. If a lateral incisor is being replaced the implant wouldnot have to be placed so apically since the average diameter of the crown at the gingival margin is 5 mm and less room is required for transition (Figs 33-37).There are also situations in which there isexcess tissue height and these require attentionas well. In these types of patients a bone scalloping procedure is required to allow placement ofthe implant shoulder in a subgingival position,once again the most efficient way to examinethis is through a surgical guide highlighting theproposed gingival margin.Errors in apico-coronal implant placementcan have serious aesthetic and biomechanicalimplications. An implant placed too coronallywill not allow adequate transition from the headof the implant to the point where the restorationexits from the free gingival margin. The restoration will look short in comparison to the contra lateral tooth. The only prosthetic ‘bailout’for this type of situation is to provide a ridgelapped restoration with contours that are pleasing to the observer’s eye (Figs 38-39).Problems can also
3. Treatment planning of implants in the aesthetic zone 4. Surgical guidelines for dental implant placement 5. Immediate implant placement: treatment planning and surgical steps for successful outcomes 6. Treatment planning of the edentulous maxilla 7. Treatment planning of the edentulous mandible 8. Impress