Transcription
Peabody Treatment Progress Battery 2007.1Chapter 12Caregiver Strain Questionnaire–Short Form(CGSQ-SF)BackgroundPurposeThe Caregiver Strain Questionnaire-Short Form (CGSQ-SF) assesses the extent to whichcaregivers and families experience additional demands, responsibilities, and difficultiesresulting from caring for a child with emotional or behavioral disorders. The CGSQ-SFalso assesses the psychological impact of the caregiving function. As observable events,the caregiver can respond to objective strain items for the whole family. However, it isgenerally agreed that a respondent can only report on his or her own subjective strain andnot on feelings of other members of the family (Platt, 1985). The terms traditionally usedin the adult mental health literature include burden of care, family burden of care, orcaregiver burden (Schene, Tessler, & Gamache, 1994). The caregiver’s perception ofcaregiving strain is an important outcome of the child or family’s treatment, and alsoinfluences help-seeking and treatment experiences, components of the treatment process.TheoryThe literature supports a two dimensional conceptualization of caregiver strain. Hoenig,and Hamilton (1967) were the first to recognize caregiver strain’s subjective andobjective dimensions. Objective caregiver strain refers to the observable negativeoccurrences and events resulting from the relative's disorder (e.g., loss of personal time,disrupted work life, difficulties with neighbors, disrupted family relationships, financialhardship). Subjective caregiver strain captures to the caregiver's feelings related to thoseoccurrences (e.g., sadness, embarrassment, guilt, anger and worry). Research has shownthat the subjective and objective dimensions of caregiver strain are related, but havedifferent sets of correlates (Montgomery, Gonyea, & Hooyman, 1985; Thompson & Doll,1982).Caregiver strain and psychological distress, although correlated, are different constructs.Moreover, caregiver strain may mediate the relationship between child problems andparental distress. Previous research modeled the relationship among caregiver strainchild clinical symptoms, caregiver psychological distress, functioning, social support,stressful life events, and material resources. Findings indicated that global caregiverstrain and caregiver psychological distress are only weakly related when other familyvariables were controlled (Brannan & Heflinger, 2001; Sales, Greeno, Shear, &Anderson, 2004).Caregiver strain has been found to be strongly related to the severity of the ill relative'ssymptoms (Brannan & Heflinger, 2001; Montgomery et al., 1985; Noh & Turner, 1987).145
Peabody Treatment Progress Battery 2007.1However, several caregiver demographic characteristics appear to influence caregiverstrain including caregiver's educational level and employment status (McDonald, et al.,1997). Racial differences in caregiver strain have long been documented in the adultmental health literature with studies generally finding that African-Americans reportlower caregiver strain than caregivers of other cultural backgrounds (Cook et al., 1994;Guarnaccia & Parra, 1996; Horwitz & Reinhardt, 1995). Similar findings have beenreported among families of children with emotional and behavioral disorders (Kang,Brannan, & Heflinger, 2005; McCabe, Yeh, Lau, Garland, & Hough, 2003).A growing body of evidence indicates that caregiver strain has important implications forhow children use mental health services after controlling for severity of child symptomsand psychosocial functioning (Angold et al., 1998; Brannan & Heflinger, 2005; Brannan,Heflinger, & Foster, 2003; Farmer, Burns, Angold, & Costello, 1997). Caregiver strain isalso associated with parental involvement in their children's treatment (Yatchmenoff etal., 1998), and it is likely that caregiver strain impacts effectiveness in the caregivingrole. Recent evidence indicates that reducing parenting stress can improve theeffectiveness of evidence-based treatments (Kazdin & Whitley, 2003). The sum of theresearch suggests that families respond to the added demands of caring for a child withemotional and behavioral challenges in different ways, and that caregivers experiencestrain at different thresholds.History of DevelopmentThe CGSQ was originally developed for the Fort Bragg Evaluation Project (Bickman etal., 1995; Brannan, Heflinger, & Bickman, 1997) and has since been used in severalmulti-site longitudinal studies. The development of the CGSQ was based on amodification of the Double ABCX model (McCubbin & Patterson, 1982; Heflinger,Northrup, Sonnichsen, & Brannan, 1998) and an extensive review of the caregivingliterature. Original psychometric analyses were conducted with the Fort Bragg sample ofyouth receiving mental health services through three Army posts (Brannan, Heflinger, &Bickman). Additional analyses have been conducted on samples of youth who wereenrolled in Medicaid (Heflinger & Brannan, 2005; Kang, Brannan, & Heflinger, 2005).Examination of the CGSQ’s measurement quality continues with other samples.The development of the CGSQ-SF in the psychometric study (described in Chapter 2)focused on the creation of a brief measure appropriate for frequent administration as partof the overall measurement battery. Findings from these analyses replicated well withtwo additional samples of families (Brannan, manuscript in progress). The short formcontains ten items, which demonstrated good psychometric properties as describedfurther below.StructureThe original CGSQ contains 21 items, which assess strain over the previous six monthperiod. The questions ask the extent to which certain occurrences or events (e.g., missedwork, financial strain, trouble with neighbors) or feelings (e.g., sadness, guilt, worry)have been a problem as a result of the child’s emotional or behavioral problems. Theresponse options range from one (not at all a problem) to five (very much a problem) on a146
Peabody Treatment Progress Battery 2007.1Likert-type scale. Factor analyses with multiple samples have confirmed that the CGSQassesses three related but distinct subscales. Objective strain refers to the observablenegative events that result from the youth's problems (e.g., financial strain, disruptedfamily relations, and difficulty with neighbors or police). Two subjective strain subscalesemerged in factor analyses. Subjective externalized strain involves outwardly directednegative feelings about the child's problems such as anger, resentment, andembarrassment. The subjective internalized strain subscale refers to inwardly directedfeelings experienced by the caregiver such as worry, guilt, and fatigue.The CGSQ-SF contains 10 items derived from the long version, with response options onthe same five-point Likert scale. It measures caregiver strain in the previous month.Factor analysis with the test sample has confirmed that the CGSQ-SF assesses a totalscore of caregiving strain and two related but distinct subscales, Objective Strain (sixitems) and Subjective Internalized Strain (four items). The subjective externalizedsubscale was omitted from the short form because of its relatively poorer internalconsistency and questionable predictive validity. The subscale scores are both means ofitem subsets: objective strain (items one to six) and subjective internalized strain (itemsseven to ten). The CGSQ-SF Total Score is calculated as the sum of the two subscales;the analyses presented in this chapter required 85% of the items to have valid answers.Psychometric information described below is based on the complete sample of thepsychometric study. See Chapter 2 for more detail on the psychometric sample and testdevelopment procedures.AdministrationThe CGSQ-SF is to be administered to parents and other caregivers (e.g., foster parents,relatives) who have primary responsibility for attending to the needs of youth withemotional and behavioral disorders. It may be administered at intake, monthly during thetreatment phase, at discharge, and follow-up as shown in Table 12.1.Table 12.1 Administration of CGSQ-SF by PhaseIntakeYATreatmentCYADischargeCYA Y Youth (age 11-18); A Adult Caregiver; C ClinicianRecommended Frequency: Every four weeksFollow-UpCYAC The suggested administration schedule of all the measures in the Peabody TreatmentProgress Battery is presented in Appendix A. All PTPB measures with self-scoringtables can be found in Appendix B.147
Peabody Treatment Progress Battery 2007.1DescriptionBasic DescriptivesAs seen in Table 12.2, the mean of the CGSQ-SF Total Score as well as the mean foreach subscale are slightly below the scale middle of 3.0. However, the overalldistribution is close to a normal distribution with no worrisome skewness or kurtosis andscores across the full range of possible scale scores.The correlation between the two subscales is large (r 0.62, N 466; p 0.0001) but notso large as to indicate they are the same. The confirmatory factor analysis (CFA)reported below provides evidence for two distinct subfactors that together composeglobal caregiver strain.Table 12.2 Descriptive Statistics for CGSQ-SF Summary ScoresNMeanStd DevSkewnessKurtosisMinMaxCGSQ-SF Total Score4932.610.970.29-0.5915Objective StrainSubscale Score4772.341.020.63-0.2415Subjective InternalizedStrain Subscale Score4852.991.160.06-1.0315Note: Data represented in this table reflect the 10-item version of the CGSQ.QuartilesQuartiles for the CGSQ-SF appear in Table 12.3. High scores are those in the topquarter, with low scores in the bottom quarter. For the CGSQ-SF Total Score, a scoregreater than 3.3 is considered high, while a score of less than 1.9 is considered low. Highand low points for the subscales are Objective, 3.0/1.5, and Subjective 4.0/2.0.To aid interpretation, the quartiles were used to create low, medium, and high scores andpercentile ranks based on comparison to the psychometric sample. This information ispresented in the last section of this chapter.Table 12.3 CGSQ-SF QuartilesQuartileCGSQ-SFTotal ScoreObjective StrainSubscaleSubjectiveInternalized StrainSubscale100 % Max75 % Q350 % Median25 % Q100 % 8
Peabody Treatment Progress Battery 2007.1Evidence of ReliabilityReliability CoefficientsThe Cronbach’s alpha internal consistency reliability correlations are presented in Table12.4. These alphas suggest satisfactory internal consistency for the total score and thesubscales.Table 12.4 Cronbach’s Alphas for the CGSQ-SFVersionCGSQ-SF(10 items Total)Objective Strain Subscale(6 items)Subjective InternalizedStrain Subscale (4 0.880.880.820.82Comprehensive Item PsychometricsTable 12.5 presents the comprehensive item psychometrics. Shaded cells indicate that acriterion was out of the range of sought values, as described previously in Table 2.2 inchapter two. Only items with two or more shaded cells are considered problematic. Allitems in the CGSQ-SF showed satisfactory scale characteristics.149
Peabody Treatment Progress Battery 2007.1MeanSt DevKurtosisItem-TotalStd CFALoadingsMeasureInfitOutfitDiscriminationHow worried about child's future4943.791.32-0.560.550.6636.021.231.340.73How tired or strained you feel4952.891.48-1.370.720.8846.690.890.871.21How sad or unhappy you ruption of personal ption of family issing work/neglecting duties4932.441.35-0.950.700.8551.750.860.821.16How guilty about child's isruption of family 1.12Family members doing ancial strain for NTable 12.5 Comprehensive Item Analysis for the CGSQ-SFNote: Items listed in ascending order by item difficulty (Measure).150
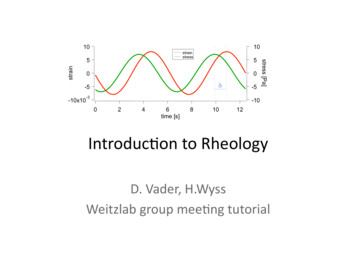
Peabody Treatment Progress Battery 2007.1Standard Errors of MeasurementFor the CGSQ-SF Total Score, the standard error of measurement (SEM) is 0.31 points.With 95% confidence, we can say that the true score is between approximately 2 SEMs,or 0.61 points on a one to five point scale. The SEMs for the CGSQ-SF subscales are0.35 for Objective Strain (95% confidence interval between approximately 2 SEMS or0.69 points) and 0.49 points for Subjective Internalized Strain (95% confidence intervalbetween approximately 2 SEMS, or 0.96 points).Reliable Change IndexThe reliable change threshold is 0.51 points with 75% confidence for the CGSQ-SF TotalScore, and gives us 75% confidence that a difference of more than 0.51 points is not dueto chance. If the change is in a positive direction (i.e., increase in score value) itrepresents an increase in reported strain, while a change in the negative directionindicates a reduction in perceived strain. Reliable change thresholds for the subscalescores are 0.58 for Objective Strain and 0.80 for Subjective Strain.Test-Retest ReliabilityNot available at this time.Evidence of ValidityScree PlotExploratory factor analysis (EFA) was conducted to examine whether the CGSQ-SFitems load on the expected factors. Examination of the scree plot (Figure 12.1) providesclear support for the general primary factor. The eigenvalue of the second factor (1.27) isabove the Kaiser criterion of one and provides some evidence for the separation of the 10items into two factors. The final factor structure was tested using confirmatory factoranalysis (CFA) as presented below.151
Peabody Treatment Progress Battery erFigure 12.1 Scree Plot of Eigenvalues for CGSQ-SFConfirmatory Factor AnalysisA confirmatory factor analysis (CFA) was run using SAS CALIS in a mode emulatingBentler & Wu’s (1995) EQS. Results are results presented in Table 12.6. The two factormodel that emerged from the EFA was reasonably supported in the CFA. The CFI andGFI fit indices just met the generally accepted thresholds. However, the RMSEAindicator was larger than would be considered ideal (i.e., 0.05-0.08). We also ran asimple one-factor model to see if the items of the CGSQ-SF were capturing a singleconstruct. The fit for the one-factor model was considerably worse than for the twofactor conceptualization of caregiver strain. The χ2 difference test indicated that the twofactor model provided a significantly better fit than did the one-factor model (χ2diff 282, df 1, p .001). In addition, when these tests were replicated with two additionalsamples, the two-factor model fit the data very well (i.e., RMSEA 0.08) (Brannan,manuscript in progress).Table 12.6 Evaluation of the CGSQ-SF Factor Structureχ2dfCGSQ One Factor Model514.035CGSQ Two Pre-statedFactorsObjective & Subjective232.434Sampleχ2 diff281.6**df 1For the CFI and GFI, values greater than 0.90 indicate good fit between a model and the data. For theRMSEA, a value of 0.05 indicates close fit, 0.08 fair fit, and 0.10 marginal fit (Browne & Cudeck, 1993).** p .001152
Peabody Treatment Progress Battery 2007.1Factor loadings for Objective Strain and Subjective Strain appear in Table 12.7. They arelarge and fairly uniform as they should be. The correlation between scores for the twofactors (r 0.69) suggests that the two forms of strain share roughly half their variance.Clinicians using the CGSQ-SQ may use the total score for simplicity and higherreliability, or the two factor scores then the distinction between objective and subjectivestrain is important.Table 12.7 CGSQ-SF Standardized Factor LoadingsItemFactor 1Objective StrainPersonal time0.85Missing Work0.83Disrupt routines0.89Family members0.68Financial Strain0.51Disrupt relationships0.70Factor 2Subjective StrainTired or strained0.80Sad or unhappy0.64Worried about futureGuilty0.650.83Note: Correlation r (Objective, Subjective) 0.69Using the CGSQ-SFScoringUse the Self-Scoring Form (Table 12.8) to calculate the CGSQ-SF subscale and totalscores. The total score is calculated as the sum of the two subscale scores and should notbe calculated if either subscale score is missing. There are no reverse coded items in theCGSQ-SF. The self-scoring form is also available in Appendix B: Measures and SelfScoring Forms.Use the scoring form in the case where measures are fully completed (100% responserate). Otherwise, in cases with missing data, scoring can be done by computing the meanof completed items. Determining when too much missing data occurs for computingsummary scores is at the discretion of the user. The analyses presented in this chapterrequired 85% of the items to have valid answers.153
Peabody Treatment Progress Battery 2007.1Table 12.8 CGSQ-SF Self-Scoring FormValues for ResponsesNot at allA littleSomewhatQuite a bitVery muchEnter value for selectedresponses here and calculatescores as 33333333444444444555555555BCDEFGHIJKSum of A-F:K / 6:MSum of G-J:M / 4:Sum of L and N:O / 2:LNOPCGSQ-SF Total Score PInterpretationThe CGSQ-SF assesses the extent to which families of children with emotional andbehavioral problems experience additional demands, difficulties, and psychologicalconsequences as a result of their caregiving role. Both objective strain (i.e., observabledisruptions, negative events and occurrences) and subjective internalized strain (i.e.,negative inwardly directed feelings such as worry, sadness, and guilt) are assessed.Subscale scores can range from one to five and the total score ranges from two to ten.The tables presented below help to judge whether a score should be considered relativelylow, medium, or high. The higher the score, the more strain the caregiver and family areexperiencing.Scores from the CGSQ-SF can be used for several purposes. First, practitioners can usethe scores to identify families who need support services and the type of services thatwould be helpful. Second, the CGSQ-SF is a useful measure of child clinical and familyoutcomes. Previous research has shown that strain scores decrease as child symptomsdecline. In addition, many programs are interested in improving the overall family154
Peabody Treatment Progress Battery 2007.1environment in order to support a healthy context for children that can maximize clinicaloutcomes. Many observers also believe that supporting caregivers and reducing strainallows them to be more effective in their caregiving role. Hence, CGSQ-SF can be usedto assess the impact of programs on child, family and caregiver outcomes.Finally, the CGSQ-SF can also be used as a predictor or mediating variable. Forexample, previous research indicates that, after controlling for severity of child problems,children of caregivers who are experiencing greater strain are more likely to useexpensive residential services (Brannan & Heflinger, 2005; Brannan, Heflinger, & Foster,2003). Some research has shown that providing support services to caregivers canimprove the effectiveness of evidence-based treatments (Kazdin & Whitley, 2003).CGSQ data can be used to help understand children’s treatment experiences and canpoint to service changes that can be made that would help meet system goals such asreduction of service costs and improvement intervention outcomes.Low, Medium, High ScoresBased on the psychometric sample, a total score greater than 3.3 is considered high,which indicates that the caregiver reports high strain. If the total score is less than 1.9, itis considered low, indicating that the caregiver’s perception of caregiving strain is low.All scores in between represent a medium level of caregiving strain. Low, medium, andhigh scores for the CGSQ-SF are presented in Table 12.9.Table 12.9 CGSQ-SF Low, Medium, and High ScoresScaleLowMediumHighCGSQ-SF Total Score 1.91.9 – 3.3 3.3Objective Strain 1.51.5 – 3.0 3.0Subjective Internalized Strain 2.02.0 – 4.0 4.0155
Peabody Treatment Progress Battery 2007.1Percentile RanksPercentile ranks appear in Table 12.10. For example, a score of 1.5 is in the 14thpercentile. This means that in the psychometric sample, 14% of caregivers scored 1.5 orlower and 86% scored higher.Table 12.10 CGSQ-SF Percentile Ranks for Total ScoresScore 8ReferencesAngold, A., Messer, S. C., Stangl, D., Farmer, E. M. Z., Costello, E. J., & Burns, B. J.(1998). Perceived parental burden and service use for child and adolescentpsychiatric disorders. American Journal of Public Health, 88, 75-80.Bentler, P. M. & Wu, E. J. C. (1995). EQS for Windows user’s guide. Encino, CA:Multivariate Software, Inc.Brannnan, A. M. (manuscript in progress). Short form of the Caregiver StrainQuestionnaire.Brannan, A. M., & Heflinger, C. A. (2005). Child behavioral health service use:Comparison of managed care and fee-for-service Medicaid systems. MentalHealth Services Research, 7, 197-211.156
Peabody Treatment Progress Battery 2007.1Brannan, A. M., & Heflinger, C. A. (2001). Distinguishing caregiver strain frompsychological distress: Modeling the relationship between child, family, andcaregiver variables. Journal of Child and Family Studies, 10, 405-418.Brannan, A. M., Heflinger, C. A., & Bickman, L. (1997). The Caregiver StrainQuestionnaire: Measuring the impact on the family of living with a child withserious emotional disturbance. Journal of Emotional and Behavioral Disorders, 5,212-222.Brannan, A. M., Heflinger, C. A., & Foster, E. M. (2003). The role of caregiver strain andother family variables in determining children’s use of mental health services.Journal of Emotional and Behavioral Disorders, 11, 77-91.Browne, M. W. & Cudeck, R. (1993). Alternative ways of accessing model fit. In K. A.Bollen & J. S. Long (Eds.), Testing structural equation models (pp. 136-162).Newbury Park: Sage.Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155-159.Cook, J. A., Lefley, H. P., Pickett, S. A., & Cohler, B.J. (1994). Age and family burdenamong parents of offspring with severe mental illness. American Journal ofOrthopsychiatry, 64, 435-447.Farmer, E. M. Z., Burns, B. J., Angold, A., & Costello, E. J. (1997). Impact of children’smental health problems on families: Relationship with service use. Journal ofEmotional and Behavioral Disorders, 5, 230-238.Guarnaccia, P. J. & Parra, P. (1996). Ethnicity, social status, and families’ experiences ofcaring for a mentally ill family member. Community Mental Health Journal, 32,243-260.Heflinger, C. A., & Brannan, A. M. (2005). Differences in the experience of caregiverstrain between families caring for youth with substance use disorders and familiesof youth with mental health problems. Journal of Child and Adolescent SubstanceAbuse, 15, 83-104.Heflinger, C. A., Northrup, D. A., Sonnichsen, S. E., & Brannan, A. M.(1998). Includinga family focus in research on community-based services for children with seriousemotional disturbance: Experiences from the Fort Bragg Evaluation Project. InM.H. Epstein, K. Kutash, & A. Duchnowski (Eds.), Outcomes for children andyouth with behavioral and emotional disorders and their families: Programs andevaluation best practices (pp.261-293). Austin, TX: Pro-Ed.Hoenig, J. & Hamilton, M. W. (1967). The schizophrenic patient in the community andhis effect on the household. International Journal of Social Psychiatry, 12, 165-157
Peabody Treatment Progress Battery 2007.1176.Horwitz, A. V. & Reinhard, S. C. (1995). Ethnic differences in caregiving duties andburdens among parents and siblings of persons with severe mental illnesses.Journal of Health and Social Behavior 36, 138-150.Kang, E. J., Brannan, A. M., & Heflinger, C. A. (2005). Racial differences in reports ofcaregiver strain among caregivers of children with emotional and behavioralproblems. Journal of Child and Family Studies, 14, 43-56.Kazdin, A. E., & Whitley, M. K. (2003). Treatment of parental stress to enhancetherapeutic change among children referred for aggressive and antisocialbehavior. Journal of Consulting and Clinical Psychology, 71, 504-515.McCabe, K., Yeh, M., Lau, A., Garland, A., & Hough, R. (2003). Racial/ethnicdifferences in caregiver strain and perceived social support among parents ofyouth with emotional and behavioral disorders. Mental Health Service Research,5, 137-148.McCubbin, H. I., & Patterson, J. M. (1982). Family adaptation to crisis. In H. I.McCubbin, A. E. Cauble, & J. M. Patterson (Eds.), Family stress, coping andsocial support (pp. 26-47). Springfield, IL: Charles C. Thomas.McDonald, T. P., Poertner, J., & Pierpont, J. (1999). Predicting caregiver stress: Anecological perspective. American Journal of Orthopsychiatry, 69, 100-109.McDonald, T. P., Gregoire, T. K., Poertner, J., and Early, T. (1997). Building a model offamily caregiving for children with emotional disorders. Journal of Emotional andBehavioral Disorders, 5, 138-148.Montgomery, R. J. V., Gonyea, J. G., & Hooyman, N. R. (1985). Caregiving and theexperience of subjective and objective burden. Family Relations, 34, 19-26.Noh, S., & Turner, R. J. (1987). Living with psychiatric patients: Implications for themental health of family members. Social Science Medicine, 25, 263-271.Platt, S. (1985). Measuring the burden of psychiatric illness on the family: An evaluationof some rating scales. Psychological Medicine, 15, 383-393.Sales, E., Greeno, C., Shear, M. K., & Anderson, C. (2004). Maternal caregiving strain asa mediator in the relationship between child and mother mental health problems.Social Work Research, 28, 211-223.Schene, A. H., Tessler, R. C., & Gamache, G. M. (1994). Instruments measuring family orcaregiver burden in severe mental illness. Social Psychiatry and PsychiatryEpidemiology, 29, 228-240.158
Peabody Treatment Progress Battery 2007.1Stommel, M., Given, C. W., and Given, B. (1990). Depression as an overriding variableexplaining caregiver burden. Journal of Aging and Health, 2, 81-102.Thompson, Jr., E. H., & Doll, W. (1982). The burden of families coping with the mentallyill: An invisible crisis. Family Relations, 31, 379-388.Yatchmenoff, D. K., Koren, P. E., Friesen, B. J., Gordon, L. J., and Kinney, R. F. (1998).Enrichment and stress in families caring for a child with a serious emotionaldisorder. Journal of Child and Family Studies, 7, 129-145.159
Chapter 12 Caregiver Strain Questionnaire–Short Form (CGSQ-SF) Background Purpose The Caregiver Strain Questi