Transcription
How to Use the ADA Type 2 DiabetesTreatment AlgorithmEric L. Johnson, MDJay Shubrook, Jr., DO, FACOFP8ACOFP 55th Annual Convention & Scientific Seminars
ACOFP FULL DISCLOSURE FOR CME ACTIVITIESPlease check where applicable and sign below. Provide additional pages as necessary.Name of CME Activity: ACOFP 55th Annual Convention and Scientific SeminarsDates and Location of CME Activity: March 22-25, 2018 – JW MarriottName of Faculty/Moderator: Eric L. Johnson, MDDISCLOSURE OF FINANCIAL RELATIONSHIPS WITHIN 12 MONTHS OF DATE OF THIS FORMA. Neither I nor any member of my immediate family has a financial relationship or interest with any proprietary entity producinghealth care goods or services.B. I have, or an immediate family member has, a financial relationship or interest with a proprietary entity producing health care goodsor services. Please check the relationship(s) that applies.Research GrantsStock/Bond Holdings (excluding mutual funds)xSpeakers’ Bureaus*EmploymentOwnershipPartnershipxConsultant for FeeOthers, please list:Please indicate the name(s) of the organization(s) with which you have a financial relationship or interest, and the specific clinical area(s) thatcorrespond to the relationship(s). If more than four relationships, please list on separate piece of paper:Organization With Which Relationship ExistsClinical Area Involved1. Medtronic1. Insulin2. Novo2. SpeakersNordiskPumps, CGM Speakers Bureau3. Sanofi3. Advisory4.4.Bureau, Advisory PanelPanel*If you checked “Speakers’ Bureaus” in item B, please continue: Did you participate in company-provided speaker training related to your proposed Topic? Did you travel to participate in this training? Did the company provide you with slides of the presentation in which you were trained as a speaker? Did the company pay the travel/lodging/other expenses? Did you receive an honorarium or consulting fee for participating in this training? Have you received any other type of compensation from the company? Please specify: When serving as faculty for ACOFP, will you use slides provided by a proprietary entity for your presentationand/or lecture handout materials? Will your Topic1 involve information or data obtained from commercial speaker :Yes:Yes:No:No:DISCLOSURE OF UNLABELED/INVESTIGATIONAL USES OF PRODUCTSxA. The content of my material(s)/presentation(s) in this CME activity will not include discussion of unapproved orinvestigational uses of products or devices.B. The content of my material(s)/presentation in this CME activity will include discussion of unapproved or investigationaluses of products or devices as indicated below:I have read the ACOFP policy on full disclosure. If I have indicated a financial relationship or interest, I understand that thisinformation will be reviewed to determine whether a conflict of interest may exist, and I may be asked to provide additionalinformation. I understand that failure or refusal to disclose, false disclosure, or inability to resolve conflicts will requirethe ACOFP to identify a replacement.Signature:Date:Eric L. Johnson, MDPlease email this form to joank@acofp.org or fax to 847-952-5116NO LATER THAN JANUARY 26, 2018
3/15/2018How to Use ADA’s Type 2 DiabetesTreatment AlgorithmJay H. Shubrook DO FACOFPProfessorPrimary Care DepartmentDirector of Clinical Research and Diabetes ServicesTouro University CaliforniaEric L. Johnson, M.D.Associate ProfessorUniversity of North Dakota School of Medicine and Health SciencesAssistant Medical DirectorAltru Diabetes CenterDisclosuresDr. Johnson: Numerous clinical multicenter diabetesstudies at Altru Site since 2003 Novo Nordisk Speakers Bureau Medtronic Speakers Bureau Advisory panels Novo Nordisk, Sanofi I have type 1 diabetes and I use insulinproducts1
3/15/2018Disclosures Jay H. Shubrook– Advisory Board Eli Lilly Novo Nordisk Intarcia– Clinical Trials Eli Lilly Astra Zeneca TheracosManagement of Hyperglycemia in T2DM1.2.3.4.Patient-centered careAnti-hyperglycemic therapyImplementation strategiesOther considerationsAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S852
3/15/2018Learning Objectives Recognize drug-specific and patient factors ofantihyperglycemic agents to support patientprovider shared decision making Demonstrate when and how to intensify therapy Identify opportunities to refer patients toDiabetes Self-Management EducationOminous Octet3
3/15/2018Patient-Centered Approach“.providing care that is respectful of and responsiveto individual patient preferences, needs, and values ensuring that patient values guide all clinicaldecisions.” Gauge patient’s preferred level of involvementExplore therapeutic choicesConsider using decision aids“Shared decision making”Lifestyle choices ultimately lie with the patientDiabetes Care 2012;35:1364–1379; Diabetologia 2012;55:1577.–1596Glycemic Recommendations: Individualized TreatmentA1C 7.0%*Preprandial capillary plasma glucose 80–130 mg/dL*(4.4–7.2 mmol/L)Peak postprandial capillary plasma glucose† 180 mg/dL*( 10.0 mmol/L)* More or less stringent glycemic goals may be appropriate for individual patients. Goals should be individualized based on duration of diabetes,age/life expectancy, comorbid conditions, known CVD or advanced microvascular complications, hypoglycemia unawareness, and individualpatient considerations.† Postprandial glucose measurements should be made 1–2 h after the beginning of the meal, generally peak levels in patients with diabetesAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S854
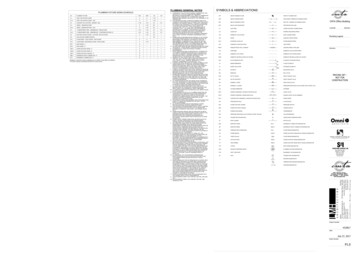
3/15/2018Approach to the Management of HyperglycemiaAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Lifestyle ManagementLifestylemanagement isa fundamentalaspect ofdiabetes careand includes Diabetes self-management education (DSME)Diabetes self-management support (DSMS)Nutrition therapyPhysical activitySmoking cessation counselingPsychosocial careAmerican Diabetes Association Standards of Medical Care in Diabetes.4. Lifestyle Management. Diabetes Care 2018;41(Suppl. 1): S38-S505
3/15/2018Anti-Hyperglycemic Therapy in T2DMTherapeutic options:Oral Agents & Non-Insulin InjectablesMost Popular in U.S. and EuropeLess Commonly UsedMetforminSGLT-2 InhibitorsGLP-1 Receptor AgonistsDPP-4 desA-Glucosidase InhibitorsColesevelamDopamine-2 AgonistsAmylin MimeticsAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85MetforminEfficacyHighHypoglycemiaWeight ChangeNoNeutral (Potential for Modest Loss)CostLowOral/SQOralAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S856
3/15/2018MetforminASCVDPotential BenefitCHFNeutralProgression d witheGRF 30CV EffectsRenal EffectsAdditionalConsiderations Gastrointestinal side effects common (diarrhea, nausea) Potential for B12 deficiencyAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Sulfonylureas (2nd Generation)Compounds: Glyburide; Glipizide; GlimepirideEfficacyHighHypoglycemiaYesWeight ChangeGainCostLowOral/SQOralAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S857
3/15/2018Sulfonylureas (2nd Generation)ASCVDNeutralCHFNeutralCV EffectsProgression of DKD NeutralRenal Effects Dosing/UseConsiderations Glyburide: not recommended Glipizide & glimepiride: initiateconservatively to avoid hypoglycemiaAdditional FDA Special Warning on increased risk of cardiovascular mortalityConsiderations based on studies of an older sulfonylurea (tolbutamide)American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85SGLT-2 InhibitorsCompounds: Canagliflozin; Dapagliflozin; ght ChangeLossCostHighOral/SQOralAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S858
3/15/2018SGLT-2 InhibitorsASCVDBenefit: canagliflozin, empagliflozinCHFBenefit: canagliflozin, empagliflozinProgression of DKDBenefit: canagliflozin, empagliflozinDosing/Use ConsiderationsCanagliflozin: Not recommendedwith eGRF 45Dapagliflozin: Not recommendedwith eGRF 60; contraindicated witheGRF 30Empagliflozin: contraindicated witheGRF 30CV EffectsRenal EffectsAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85SGLT-2 InhibitorsAdditional Considerations FDA Black Box: risk of amputation (canagliflozin) Risk of bone fractures (canagliflozin)DKA risk (all agents, rare in T2DM)Genitourinary infectionsRisk of volume depletion, hypotensionIncrease LDL cholesterolAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S859
3/15/2018GPL-1RAsCompounds: Exenatide; Exenatide extended release; lixisenatide,liraglutide; semaglutide; dulaglutideEfficacy HighHypoglycemia NoWeight Change LossCost HighOral/SQ SQAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85GPL-1RAsASCVDNeutral: lixisenatide, exenatideextended releaseBenefit: liraglutideCHFNeutralProgression of DKDBenefit: liraglutideCV EffectsDosing/UseRenal Effects ConsiderationsExenatide: not indicated witheGRF 30Lixisenatide: caution with eGRF 30Increased risk of side effects inpatients with renal impairmentAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8510
3/15/2018GPL-1RAsAdditional Considerations FDA Black Box: Risk of thyroid c-cell tumors(liraglutide, dulaglutide, exenatide extended release) Gastrointestinal side effects common (nausea,vomiting, diarrhea) Injection site reactions Acute pancreatitis riskAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85DPP-4 InhibitorsCompounds: Sitagliptin; Saxagliptin; Linagliptin; AlogliptinEfficacy IntermediateHypoglycemia NoWeight Change NeutralCost HighOral/SQ OralAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8511
3/15/2018DPP-4 InhibitorsASCVDNeutralCHFPotential Risk: saxagliptin, alogliptinProgression of DKDNeutralCV EffectsRenal Effects Dosing/UseConsiderationsRenal dose adjustment required;can be used in renal impairmentAdditional Potential risk of acute pancreatitisConsiderations Joint painAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Thiazolidinediones (TZDs)Compounds: Pioglitazone; RosiglitazoneEfficacy HighHypoglycemia NoWeight Change GainCost LowOral/SQ OralAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8512
3/15/2018Thiazolidinediones (TZDs)ASCVDPotential Benefit: pioglitazoneCHFIncreased RiskProgression of DKDNeutralCV EffectsRenal Effects Dosing/UseConsiderations No dose adjustment required Generally not recommended inrenal impairment due topotential fluid retentionAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Thiazolidinediones (TZDs)Additional Considerations FDA Black Box: Congestive Heart Failure(pioglitazone, rosiglitazone) Fluid retention (edema; heart failure)Benefit in NASHRisk of bone fracturesBladder cancer (pioglitazone)Increase LDL cholesterol (rosiglitazone)American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8513
3/15/2018InsulinEfficacy HighestHypoglycemia YesWeight Change GainCostHuman Insulin: LowAnalogs: HighOral/SQ SQAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85InsulinASCVDNeutralCHFNeutralProgression of DKDNeutralCV EffectsRenal Effects Dosing/UseConsiderationsLower Insulin doses required witha decrease in eGRF; titrate perclinical response Injection site reactionsAdditional Higher risk of hypoglycemia with a human insulin (NPHConsiderationsor premixed formulations) vs. analogsAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8514
3/15/2018Individualizing TreatmentAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes. DiabetesCare 2018; 41 (Suppl. 1): S73-S85Considerations in Designing an OptimalGlucose Lowering Drug Regimen for PatientsAgeWeightSex / racial / ethnic / genetic differencesComorbidities Coronary artery disease Heart Failure Chronic kidney disease Liver dysfunction Hypoglycemia-proneIdentifying and addressing barriers to medication adherence Cost Side effectsAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8515
3/15/2018Antihyperglycemic Therapy in Adults with T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Antihyperglycemic Therapy in Adults with T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8516
3/15/2018Antihyperglycemic Therapy in Adults with T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Case 1 JW is a 42 year old male who presents for a workphysical. He denies any specific symptoms orconcerns. You had mentioned a couple of years agothat he had “pre-diabetes” and he should loseweight and there was a class he could take but hehas not found the time to do this. Med hx/Surg hx: none Meds: omeprazole OTC prn Allergies: none17
3/15/2018Case 1: Physical exam––––Obese male BMI 32Bp 142/88Mild athlete’s footExam otherwise normal Labs––––HbA1c 7.5%Glucose (fasting) 138 mg/dlHigh trigs (258) low HDL 28Labs otherwise normalCase 1: Question 1 What is your A1c goal for this patient?––––A. 6.5%B 7.0%C. 7.5%D 8.0%18
3/15/2018Case 1: Question 2 What is the treatment plan for this patient? We will assume that he will be offered diabeteseducaton––––A. therapeutic lifestyle change (TLC)B. TLC metforminC. TLC other oral medicationD. TLC insulinCase 1: Question 3 Which of the following conditions would makeyou not want to use metformin?–––––A. peripheral neuropathyB. Stage 3 CKDC. Stage 4 CKDD. Stage 3 heart failureE. Cirrhosis19
3/15/2018Case 1: Question 4 What is your next pharmacologic option for thispatient? If A1c not at goal in 3 months?)––––––SulfonylureaDPP-4 inhibitorGLP-1 RASGLT-2 inhibitorTZDAlpha-glucosidase inhibitorWhat About The Patient with EstablishedAtherosclerotic Cardiovascular Disease(ASCVD)?20
3/15/2018Impact of Intensive Therapy for Diabetes:Summary of Major Clinical TrialsStudyUKPDSDCCT / EDIC*ACCORDADVANCEVADTMicrovasc CVDMortality Kendall DM, Bergenstal RM. International Diabetes Center 2009*UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854.Holman RR et al. N Engl J Med. 2008;359:1577. DCCT Research Group. N Engl J Med 1993;329;977.Nathan DM et al. N Engl J Med. 2005;353:2643. Gerstein HC et al. N Engl J Med. 2008;358:2545.Patel A et al. N Engl J Med 2008;358:2560. Duckworth W et al. N Engl J Med 2009;360:129. (erratum:Moritz T. N Engl J Med 2009;361:1024) . Writing Group for the DCCT/EDIC Research Group. JAMA. 2015;313(1):45-53.in T1DMInitial TrialLong Term Follow-upCardiovascular Benefit of Diabetes Medications21
3/15/2018SUSTAIN-6 New GLP-1 agonist just approved December2017, not on algorithm yet 26% risk reduction in the primary outcome, acomposite of nonfatal heart attacks, nonfatalstrokes, and cardiovascular deathN Engl J Med. 2016;375(19):1834-1844LEADERLiraglutideT2DM at higher CVD risk 22% risk reduction of cardiovascular death 22% risk reduction of nephropathy 12% risk reduction of non-fatal heartattacks,11% risk reduction of non-fatal strokesbut neither statistically significant 13% reduction of primary CVD endpointsN Engl J Med 2016; 375:311-32222
3/15/2018EMPA-REGEmpagliflozin T2DM patients with high CVD risk Reduced the primary major adverse cardiac event (MACE) endpoint (CV death, nonfatal myocardial infarction, nonfatal stroke)by 14% 38% reduction in CV mortality No significant decrease in nonfatal myocardial infarction orstroke. 35% reduction in hospitalization for heart failure withoutaffecting hospitalization for unstable anginaN Engl J Med 2015; 373:2117-2128CANVASCanagliflozinT2DM patients with high CV risk 14% reduction in CV endpoints 40% reduction in renal composite endpoints Higher risk of distal amputationsN Engl J Med 2017; 377:644-65723
3/15/2018Pharmacologic Therapy For T2DM:ASCVD RecommendationsIn patients with T2DM and established ASCVD: antihyperglycemic therapy should begin with lifestylemanagement and metformin– subsequently incorporate an agent proven to reduce majoradverse CV events and CV mortality (currently empagliflozinand liraglutide), after considering drug-specific and patientfactors (Table 8.1). A– the antihyperglycemic agent canagliflozin may be consideredto reduce major adverse CV events, based on drug-specificand patient factors (Table 8.1). CAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Case 2 MT is a 58 y/o Hispanic female Type 2 diabetes x 11 years with dyslipidemia, hypertension,albuminuria, non-painful peripheral neuropathy, obesity,NAFLD, history of MI 3 years ago Current medications:–––––––Metformin 1000mg BIDGlipizide 10mg dailyPioglitazone 30mg dailyLisinopril 20mg dailyMetoprolol XL 25mg dailyAtorvastatin 80mg dailyAspirin 81mg daily24
3/15/2018Case 2: Question 1 In this patient with established ASCVD, whatshould we consider beyond initial metformintherapy? A. TZD B. DPP-IV inhibitor C. GLP-1 RA (liraglutide) D. SGLT-2 inhibitor (canagliflozin, empagliflozin) E. either C or DCase 2: Question 2 In this patient with established ASCVD, what shouldwe consider beyond initial metformin therapy? A. TZD B. DPP-IV inhibitor C. GLP-1 RA (liraglutide) D. SGLT-2 inhibitor (canagliflozin, empagliflozin) E. either C or DAnswer: E25
3/15/2018Case 2 Physical exam– Nonproliferative retinopathy, normal heart and lung sounds, obese,decreased vibratory and filament sensation in otherwise healthyappearing feet Concerns– Many blood sugars in 200’s-300’s, but occasional less than 70 mg/dl– Fatigue– Difficulty losing weight Labs– A1C 10.2%– Lipids target (on moderate statin dose), serum creatinine 0.9, GFR 54,hepatic function minor transaminase elevation, urine albumin 110(normal 30)What next?Case 2 Recall current standards of care recommendSGLT-2 inhibitor (empagliflozin, canagliflozin) orGLP-1 agonist (liraglutide) in the setting ofestablished cardiovascular disease Empagliflozin and liraglutide have FDAindication One of patients main complaints is difficultylosing weight, both of these drug classes aremore weight-neutral or -loss26
3/15/2018Case 2 Could do any of the following in the setting of establishedCVD– Add liraglutide (GLP-1 RA)– Add empagliflozin (or canagliflozin) (SGLT-2 inhibitor)– Both GLP-1 RA or SGLT-2 inhibitor for maximal weight loss Would definitely– Continue metformin (renal function is OK)– Refer to diabetes educator and dietician– Review activity level/exercise prescription Could consider– Stop glipizide– Stop pioglitazoneInsulin Therapy in T2DM The progressive nature of T2DM should beregularly and objectively explained to T2DMpatients. Avoid using insulin as a threat, describing it as afailure or punishment. Give patients a self-titration algorithm.American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8527
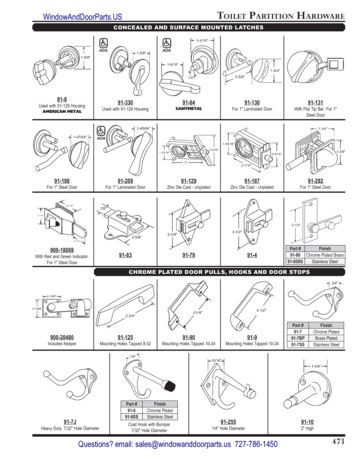
3/15/2018Combination Injectable Therapy in T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Therapeutic Options: InsulinsHumanInsulins analogues(glargine,detemir,degludec)Regularhuman insulinRapidanalogues(lispro, mulationsBiosimilarInsulinBasaglar(a biosimilarversion ofinsulinglargine);long-actingDiabetes Care 2012;35:1364–1379; Diabetologia 2012;55:1577–1596Diabetes Care 2015;38:140-149; Diabetologia ly.com/releasedetail.cfm?ReleaseID 1004325https://www.basaglar.com/en/28
3/15/2018Anti-Hyperglycemic Therapy: InsulinsInsulin levelRapid (Lispro, Aspart, Glulisine)Short (Regular)Long (Detemir)(Degludec)Long (Glargine)0246810121416Hours After Injection18202224Approach to Starting and Adjusting Insulin in T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8529
3/15/2018Approach to Starting and Adjusting Insulin in T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S85Approach to Starting and Adjusting Insulin in T2DMAmerican Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: Standards ofMedical Care in Diabetes. Diabetes Care 2018; 41 (Suppl. 1): S73-S8530
3/15/2018Case 3 GM is a 64 y/o white male Diagnosed with type 2 diabetes after 2 fasting bloodsugars of 154 mg/dl and 142 mg/dl and A1C of 6.8% Saw Diabetes Educator and Dietician at diagnosis Pre-existing– HTN (on Lisinopril 10mg)– Dyslipidemia(on atorvastatin 40mg)– no history of ASCVD ASA 81 mg daily (over 50 DM)Case 3 Physical Exam BP 132/78, pulse 80, BMI 34 Fundi normal Obese Feet healthy appearing other than benign calluses Lipids in target (measure of compliance), hepatic andrenal chemistries all normal31
3/15/2018Case 3 Current Diabetes Medications:– Metformin 1000mg BID– Glimepiride 4mg daily– Basal insulin 40 units daily A1C 8.2% Fasting blood glucose values 110’s-130’s 2 hour post-prandial glucose values 220’s-250’s What next?Case 3 What would be an appropriate choice for thispatient? A. DPP-IV inhibitorB. Higher dose of sulfonylureaC. GLP-1 RAD. Rapid acting insulin32
3/15/2018Case 3 What would be an appropriate choice for thispatient? A. DPP-IV inhibitorB. Higher dose of sulfonylureaC. GLP-1 RAD. Rapid acting insulinAnswer: C or DCase 3 Options– Add rapid acting insulin to largest meal of the day33
3/15/2018Case 3– Add GLP-1 RA (or switch to combination GLP-1 RA basal insulin) (lirglutide degludec or lixisenatide glargine)– Switch to premixCase 3 Patient should see Diabetes Educator (again)and Dietician for regimen change/instruction andlifestyle evaluation If not reaching targets, consider multiple dailyinjections of insulin per algorithm Could consider stopping sulfonylurea may notbe adding a lot of benefit, or could contribute tohypoglycemia34
3/15/2018Key PointsIndividualize glycemic targets & BG-lowering therapiesLifestyle foundation of any T2DM therapy programUnless contraindicated, metformin is optimal first-line drug In patients with ASCVD and T2D, subsequent treatmentshould incorporate agent proven to CV events and/or CVmortality Ultimately, many patients will require insulin therapy aloneor in combination with other agents to maintain BG control Shared decision making (focus on his/her preferences,needs & values)Comprehensive CV risk reduction - a major focus of therapyDiabetes Care 2012;35:1364–1379; Diabetologia 2012;55:1577–1596Diabetes Care 2015;38:140-149; American Diabetes Association Standards of Medical Care in Diabetes.Diabetes Care 2018; 41 (Suppl. 1): S73-S85Inzucchi SE et al. Diabetologia 2015;58(3):429–442.Case 4 TG, a 58-year-old African American, has had T2D for8 years Currently being treated for hypertension (12 years)and dyslipidemia (10 years) Concerned about uncontrolled blood glucose level, arecent increase in weight (5 lbs) Non-smoker and only occasionally consumes alcohol Walks 15-20 minutes, three times a week Diet has improved over last 5 years after consult withRD, but she admits to having a “sweet tooth”(Continued )35
3/15/2018Case 4 Physical exam:– General examination normal, No pallor, cyanosis, clubbing orlymphadenopathy– Height, 5’2” (157 cm); weight, 152 lbs (69 kg)– BMI, 27.8 kg/m²– BP, 132/86 mmHg– Pulse 80/min, regular, peripheral pulses well felt– Systemic examination- normal– Foot examination is normal– Fundus examination :Grade I non proliferative diabetic retinopathy Medication history: Glimepiride 2 mg daily BID Metformin sustainedrelease preparations 1000 mg daily Telmisartan 40 mg daily Atorvastatin 10 mg at night Aspirin 81 mg at night(Continued )Case 4 Labs:– A1C 8.3 %– Lipids TC 190, TG’s 210, HDL 35, LDL 101– Fasting blood glucose values 130’s-160’s– Post-prandial blood glucose values 190’s-220’s– GFR 65, serum creatinine 1.2, hepatic chemistriesnormal– Urine normal (no albuminuria)36
3/15/2018Case 4From the lab results, which plasma glucose patternsof hyperglycemia are cturnalB and C aboveCase 4A drug from which of the following drug classes couldyou suggest to intensify Mrs. G’s treatment to manageher hyperglycemia?A. GLP-1 receptor agonistB. DPP-4 inhibitorC. SGLT2 inhibitorD. Basal insulinE. A, B, C, or D above37
3/15/2018Case 4: Think-Pair-Share What option you would have tried first? Would you discontinue the sulfonylurea or add theGLP-1 receptor agonist to themetformin/sulfonylurea? What if this patient had chronic kidney disease(GFR 40)? What if this patient had ASCVD?Thank You!38
Diabetes self-management support (DSMS) Nutrition therapy Physical activity Smoking cessation counseling Psychosocial care Lifestyle management is a fundamental aspect of diabetes care and includes American Diabetes Association Standards of Medical Care in Diabetes. 4. Lifestyle Management.