Transcription
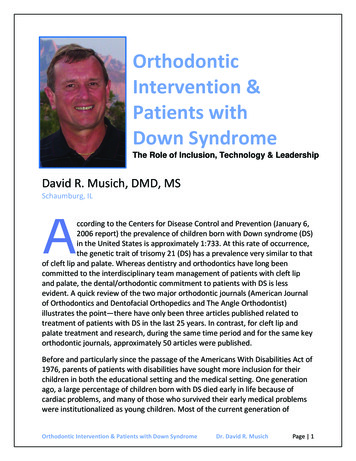
www.cclg.org.ukPosterior fossa syndromeInformation for parents of a child with PFSThis factsheet has been written to help you understandposterior fossa syndrome (PFS), the name given to a collectionof symptoms which may occur together following surgery to theback of the brain. PFS is also sometimes known as cerebellarmutism syndrome.Symptoms are not always present immediately after surgery, but often develop in the followingfew days. Early symptoms include difficulties with speech, movement and swallowing. If your childdevelops PFS they may appear very different. It’s important to remember they are still the same childon the inside.The information in this factsheet explains what PFS is and its impact, and provides information aboutrehabilitation and recovery. If you have any questions, the medical team treating your child will behappy to answer them.When does PFS occur andhow long does it last?PFS has been reported to occur in up to thirty percent ofchildren undergoing surgery to the back of the brain. Theseverity of the condition varies considerably from one childto the next. It is therefore difficult to predict the extent orduration of their recovery.However, the majority of children will make significantimprovements. The extent of any long term difficultiesmay not be evident initially and become apparent lateras the child returns to education and home life.Ongoing rehabilitation and support may be required formonths or even years.CausesThe exact cause of PFS is unknown. It occurs followingoperations to the cerebellum (responsible for balanceand coordination) and brainstem (responsible forbasic functions such as breathing, heart rate and bodytemperature), particularly those to remove a type oftumour called medulloblastoma. Tumours that involve thebrain stem and are located in the brain midline are alsoassociated with PFS.It is currently unclear why it affects some children and notothers, and there is ongoing research into this subject.Current evidence suggests that PFS is caused by aninterruption to a particular pathway in the brain that sendssignals from the cerebellum to the parts of the brain thatprocess information, sensations and body movements.www.cclg.org.uk1
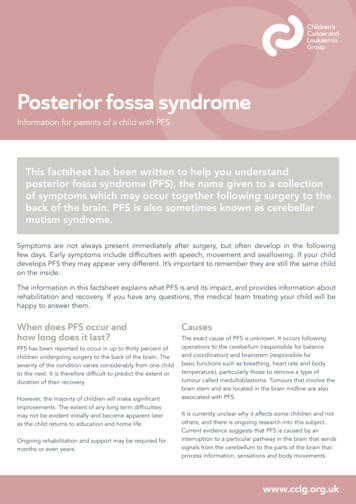
Posterior fossa syndromeAreas of the brainand an approximate guide to their functionsFrontal lobeParietal lobe(Movement, speech,behaviour regulation)(Integrating informationfrom our senses)Occipital lobe(Vision)Temporal lobe(Memory, processing sound,understanding language)Brain stem(Breathing, heartrate, alertness)Cerebellum(Balance, co-ordination)PFS is identified by a collection of symptomsSpeech and communicationReduced or absent speech is often one of the moststriking features, which is why PFS is sometimes called‘cerebellar mutism’. Children may not speak at allor their speech may be slow or slurred and difficultto understand. This usually occurs within the first fewdays after surgery but may not be present immediatelyafter surgery.Body movements (‘motor control’)Children can display low muscle tone (hypotonia),unsteadiness and problems with coordination (ataxia).They may not be able to coordinate voluntarymovements, and can find it difficult to hold theirhead up or sit up.2PFS can affect the movements involved in chewing andswallowing. In severe cases, children may have difficultyswallowing their saliva, making it unsafe for them to haveanything to eat and drink by mouth. Usually, childrenregain the voluntary movements of the lips and tonguefirst before being able to eat and drink, for example,being able to stick out their tongue and move it fromside to side. Children who have been severely affectedmay need tube feeding, especially when radiotherapyand chemotherapy are given at the same time.Emotional difficulties (‘emotional lability’)Many children and young people experience ‘emotionallability’, a term used to describe rapid changes of moodand can include sudden uncontrolled laughter or tears.They may also display angry behaviour such as shoutingor swearing, which may seem out of character.Mood swings and agitation can be very distressing forfamilies to see and can be particularly evident after theinitial stages of recovery following brain surgery. Thiscan be made worse by a child feeling scared, or unableto communicate.Learning and understanding (‘cognition’)Due to the speech and movement problems seenin PFS, it can be difficult to assess the impact onchildren’s learning abilities until they have madea significant recovery.
www.cclg.org.ukNevertheless, it is important to consider that thinkingand reasoning could be impaired and processing speedis likely to be slowed. This means that children may beconfused, might find it difficult to make decisions, andcan often take a long time to respond to questions.The aim of rehabilitation is usually to recover skills,but sometimes other ongoing treatment can affect yourchild’s functioning and therefore the aim at that pointcan be to help your child maintain skills.A child may appear uncooperative and be reluctant orunwilling to undertake therapy during their rehabilitationand may need lots of patience and understanding.If your child developsPFS they may appear verydifferent. It’s important toremember they’re still the samechild on the inside.PFS symptomswill improve with timebut recovery is differentfor each child.Your child will need ongoing rehabilitationfrom a team of therapists to help theirrecovery in a range of different areas,depending on their individual difficulties.See page 4 to read about therehabilitation process.3
Posterior fossa syndromeRehabilitationRehabilitation can take place in hospital, at home, and occasionally ata specialist rehabilitation centre depending upon your child’s individualneeds. Children who have more severe symptoms of PFS early on aremore likely to have symptoms that last longer.Your child’s rehabilitation team will includethe following specialists: Speech and language therapists can providesupport for any speech, language and communicationdifficulties. In addition, they help with swallowingdifficulties, supporting the process of eating anddrinking and ensuring it is safe and pleasurable. Physiotherapists can provide assistance withmaximising strength, balance and coordination ofmovements, helping children regain their physical skills.4 Occupational therapists support children toparticipate in everyday life activities, enablingchildren to regain their independence. Clinical psychologists or neuropsychologistscan help to identify and support any difficulties withongoing learning as well as supporting children andtheir families with emotional or behavioural issuesas they adjust to what has happened to them.Other therapists, for example, play therapists, arttherapists and music therapists, may also be involvedin your child’s rehabilitation.
www.cclg.org.ukRecovery and long term prognosisMotor controlFor a few children it will take many months to regaintheir physical abilities. Most but not all will be able towalk independently. However, ongoing difficulties withbalance, coordination and body movement are common.Speech and communicationIn most cases communication comes back very graduallywith more spontaneous sounds first (laughing and crying)followed by individual sounds, slowly developing intosingle words and extending into short phrases. Somechildren may communicate non-verbally using headnods/shakes, gestures or communication boards initially.Emotional difficultiesEmotional difficulties can persist after recovery hasbeen made in many other areas. In addition to suddenemotional distress associated with emotional lability(often crying or appearing agitated), children are atincreased risk of emotional, behavioural and socialproblems following PFS. Children often feel frustrated ifthey are unable to participate in the activities that theyused to enjoy. This may affect their confidence as well associal relationships. If you are concerned about ongoinglow mood or behaviour problems do discuss this witha member of your child’s rehabilitation team.Learning and cognitionThere are many factors that can affect learning andcognition in children with brain tumours, such as thetumour itself, surgery and radiotherapy. It is thereforedifficult to establish how much of an impact PFS has oncognitive function in the long term. Research comparingchildren with the same type of tumour and treatment,with or without PFS, has found that children with PFScan have more difficulties in specific cognitive areas,such as attention and working memory. However,further research is needed in this area.It’s important to remember any learning difficulties will vary for each child.It is helpful for your child to have a neurocognitive assessment by a clinicalpsychologist, educational psychologist or clinical neuropsychologist toidentify your child’s particular strengths and weaknesses.5
Posterior fossa syndromeReturning homePreparation for your child’s discharge from hospital begins as soon as your childis admitted to hospital as it can take some time to arrange the right support.The medical and nursing team will work closely withother professionals to assess your child’s needs and anyadditional support required, both in the short and longterm. This assessment should include considerationof medical needs, physical needs, psychological andpractical needs and returning to school.Medical needsInformation about any ongoing treatment for yourchild’s tumour will be explained to you in detail,and you will receive information on how to care foryour child at home. Referrals will be made to theappropriate community nursing team and otherservices you may need.Physical needsYour child will have an assessment to see how theywill cope at home. If any equipment is needed,this will be ordered by the occupational therapyteam. If required, information about more permanentadaptations to your home will be provided.Psychological and practical needsMembers of the hospital team, including the outreachnurses and CLIC Sargent social worker, will be ableto support you, and also advise on other supportavailable locally.Returning to schoolGoing back to school is an essential part of your child’songoing rehabilitation. It is usually possible for yourchild to return to school on a reduced timetable andslowly build up the time they spend at school. Althoughyour child may tire easily, being back at school will helpyour child get back into a routine and give them theopportunity to see their friends.If you feel that your child has needs which are not beingmet, discuss this with your specialist nurse or consultantwho will be able to liaise with the relevant professional.Leaving hospital can often be a difficult time forfamilies who can feel that they are losing the safetynet of the professionals who understand their child’sunique needs. It may be useful to discuss these concernswith a member of the team, for example, your specialistnurse or CLIC Sargent social worker, who will be ableto signpost you to support groups or other organisationswho are able to help.Getting support in educationEvery mainstream school or nursery has a SpecialEducational Needs Coordinator (SENCo) who isresponsible for ensuring that the needs of children withdisabilities or special educational needs are met. Withincolleges there is also a designated person for this rolebut they may not be called a SENCo.In order to ensure that your child is supported effectively,it is helpful to discuss your child’s needs with the schoolSENCo as early as possible. A member of the hospitalteam may be able to support you with this. It may alsobe possible to invite the SENCo or another seniormember of school staff to the multidisciplinary teammeeting (MDT) or discharge meeting so they can beginto understand your child’s needs and ask questions.Additional support after leaving hospitalAn Education, Health and Care (EHC) plan looks atall of your child’s needs across education, health andsocial care and ensures that the child receives the rightamount of support by engaging everyone involved inthe child’s care. EHC plans are for all children withspecial education needs. An assessment will need tobe requested by the school, hospital or parents andis carried out by the local authority.Whilst your child is attending hospital regularly it islikely that you will be able to access support fromwithin the hospital. Upon discharge the hospital teamshould refer you to appropriate professionals in theWhether or not your child has an EHC plan,their progress and level of support should beregularly reviewed.Make sure the school understands your child’s needs soappropriate support is in place and your child can beincluded in normal school life as much as possible.6community for support. This can include communityphysiotherapy, occupational therapy and speech andlanguage therapists.
www.cclg.org.ukFurther informationabout returning homeafter treatment for a braintumour can be found in theCCLG booklet ‘Brain andspinal tumours’.CCLG also produces a booklet entitled‘Welcome back!’, which offers adviceand support for teachers helping childrenand young people return to schoolafter a diagnosis of cancer.It’s importantyou plan time foryourself and ensureyou have the supportyou need.Supporting your childTaking care of yourselfYour child will need ongoing support and parentsunderstandably find it very stressful to see their childupset. It is natural to try to find out what your child isupset about to make things easier for them. However,as biological changes in the brain can be associatedwith strong emotional reactions without any apparenttrigger, your child may not know why they are upset.Whilst it is important to encourage your child to talkabout their feelings, it is also important to knowthat at times, they will have no answer.Seeing your child suffer from the symptoms of PFS canbe very distressing. It is very normal to feel overwhelmedat times, especially as you already have to deal with yourchild’s diagnosis and treatment. Being there for yourchild, providing reassurance and familiarity will helpthem begin their gradual process of recovery.On those occasions it is helpful to have a plan in placeof how your child can manage their distress until itpasses. They may simply benefit from a hug, somequiet time, an object that is special to them, anactivity that distracts them, or some rest.Whilst your natural instinct as a parent may be to give upeverything to support your child, you also need to lookafter yourself to allow you to best support your child.Try to eat regularly (even if you don’t feel like it) and restwhen possible. The recovery process from PFS may takea long time. It is important that you plan time for yourselfand ensure that you have the support you need in orderto be able to be there for your child throughout theirjourney of recovery.7
Posterior fossa syndromeSources of information and supportUseful organisationsUseful resourcesChildren’s Cancer and Leukaemia GroupThere’s a comprehensive range of free publicationsavailable for children and young people with cancerand their families from a number of InformationStandard accredited organisations, includingCCLG and CLIC Sargent.www.cclg.org.ukCCLG is the UK and Ireland’s professional association for those involvedin the treatment and care of children with cancer, and is dedicated toimproving best practice and outcomes. We support research and alsoprovide accredited information for patients and families.Children’s Cancer and Leukaemia Group(CCLG)The Child Brain Injury Trustwww.childbraininjurytrust.org.ukHelpline: 0303 303 2248Provides information on children’s acquired brain injury and offerstraining and support for professionals including school staff.The Children’s Trust Brain Injury Hubwww.braininjuryhub.co.ukProvides information on acquired brain injury. Also providesa discussion forum for parents and families.CLIC Sargentwww.clicsargent.org.ukHelpline: 0300 330 0803Children and young people with cancer:A Parent’s Guide (2014)Welcome back! A guide for teachers helping childrenand young people returning to school after a diagnosisof cancer (2015)Brain and spinal tumours (2016)For schoolsProvides practical support and advice for children and young peopleaffected by cancer and their families and offers accredited information.The Brain Tumour Charitywww.thebraintumourcharity.orgProvides information about brain tumours and their treatment.The Danny Green Fundwww.thedannygreenfund.org.ukCancer and school life pack (CLIC Sargent, 2014)Welcome back! A guide for teachers helping children andyoung people returning to school after a diagnosis ofcancer (CCLG, 2015)Returning to school: A teacher’s guide for pupils withbrain tumours (Second edition, The Royal Marsdenand Cerebra, 2015)A charity set up by the family of a child who experienced PFS.Provides information and funding for equipment and therapy.This factsheet was written by Louise Robinson, CLIC Sargent Neurooncology Nurse Keyworker (Nottingham), Dr Susanna Waern, ClinicalPsychologist (The Royal Marsden), and Dr Sophie Thomas, ConsultantPaediatric Neuropsychologist (Nottingham) in conjunction with theCCLG Publications Committee, comprising multiprofessional expertsin the field of children’s cancer.Children’s Cancer and Leukaemia Group is a leading children’s cancercharity and the UK and Ireland’s professional association for thoseinvolved in the treatment and care of children with cancer. Each weekin the UK and Ireland, more than 30 children are diagnosed. Two outof ten children will not survive their disease.We bring together childhood cancer professionals to ensure all childrenreceive the best possible treatment and care. We fund and supportresearch into childhood cancers, and we help young patients andtheir families with our expert, high quality and award-winninginformation resources.Children’s Cancer and Leukaemia GroupUniversity of LeicesterClinical Sciences BuildingLeicester Royal InfirmaryLeicester LE2 7LX8Registered charity number 2866690116 252 G UKWith thanks to the Brainbow brain tumour rehabilitation serviceteam at Addenbrooke’s Hospital for their contributions and forreviewing the text.CCLG makes every effort to ensure that information provided isaccurate and up-to-date at the time of printing. We do not acceptresponsibility for information provided by third parties, includingthose referred to or signposted to in this publication. Informationin the publication should be used to supplement appropriateprofessional or other advice specific to your circumstances.For information about the sources used to put this publication together,please contact us.Publication of this factsheet was funded by CCLG. CCLG 2016Published: May 2016Next review due: May 2019
The medical and nursing team will work closely with . psychological and practical needs and returning to school. Medical needs Information about any ongoing treatment for your child's tumour will be explained to you in detail, . (MDT) or discharge meeting so they can begin to understand your child's needs and ask questions.