Transcription
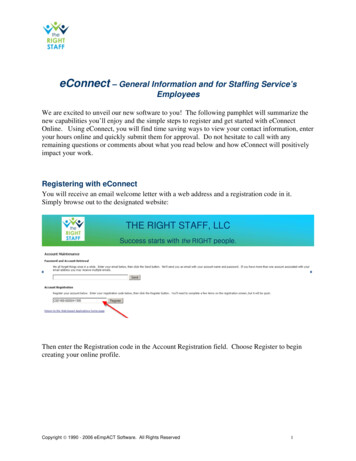
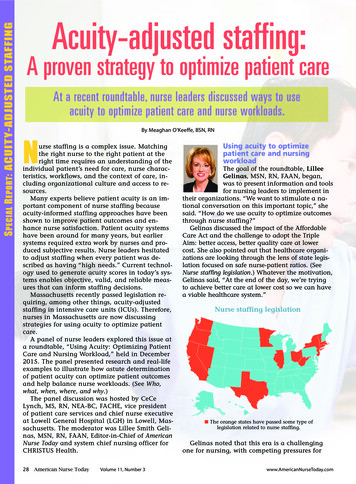
S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGAcuity-adjusted staffing:A proven strategy to optimize patient careNAt a recent roundtable, nurse leaders discussed ways to useacuity to optimize patient care and nurse workloads.By Meaghan O’Keeffe, BSN, RNurse staffing is a complex issue. Matchingthe right nurse to the right patient at theright time requires an understanding of theindividual patient’s need for care, nurse characteristics, workflows, and the context of care, including organizational culture and access to resources.Many experts believe patient acuity is an important component of nurse staffing becauseacuity-informed staffing approaches have beenshown to improve patient outcomes and enhance nurse satisfaction. Patient acuity systemshave been around for many years, but earliersystems required extra work by nurses and produced subjective results. Nurse leaders hesitatedto adjust staffing when every patient was described as having “high needs.” Current technology used to generate acuity scores in today’s systems enables objective, valid, and reliable measures that can inform staffing decisions.Massachusetts recently passed legislation requiring, among other things, acuity-adjustedstaffing in intensive care units (ICUs). Therefore,nurses in Massachusetts are now discussingstrategies for using acuity to optimize patientcare.A panel of nurse leaders explored this issue ata roundtable, “Using Acuity: Optimizing PatientCare and Nursing Workload,” held in December2015. The panel presented research and real-lifeexamples to illustrate how astute determinationof patient acuity can optimize patient outcomesand help balance nurse workloads. (See Who,what, when, where, and why.)The panel discussion was hosted by CeCeLynch, MS, RN, NEA-BC, FACHE, vice presidentof patient care services and chief nurse executiveat Lowell General Hospital (LGH) in Lowell, Massachusetts. The moderator was Lillee Smith Gelinas, MSN, RN, FAAN, Editor-in-Chief of AmericanNurse Today and system chief nursing officer forCHRISTUS Health.28American Nurse TodayVolume 11, Number 3Using acuity to optimizepatient care and nursingworkloadThe goal of the roundtable, LilleeGelinas, MSN, RN, FAAN, began,was to present information and toolsfor nursing leaders to implement intheir organizations. “We want to stimulate a national conversation on this important topic,” shesaid. “How do we use acuity to optimize outcomesthrough nurse staffing?”Gelinas discussed the impact of the AffordableCare Act and the challenge to adopt the TripleAim: better access, better quality care at lowercost. She also pointed out that healthcare organizations are looking through the lens of state legislation focused on safe nurse-patient ratios. (SeeNurse staffing legislation.) Whatever the motivation,Gelinas said, “At the end of the day, we’re tryingto achieve better care at lower cost so we can havea viable healthcare system.”Nurse staffing legislationn The orange states have passed some type oflegislation related to nurse staffing.Gelinas noted that this era is a challengingone for nursing, with competing pressures forwww.AmericanNurseToday.com
Shared governance: The key toimplementing changeAndrea Erickson, MSN, RN, CNML,director of inpatient critical care services at LGH, spoke of the large taskher organization faced as it worked tocomply with the Massachusettsstaffing bill passed in November 2014. Using theshared governance model to guide its journey, LGHbegan to develop and implement an acuity tool tomeet the state’s January 2017 deadline.The shared governance model, Erickson explained, proved vital to LGH as it worked towardimplementing those changes. (See Shared governance model.) “Shared governance gives nursespower in their practice,” she said. “It gives them avoice, which promotes innovation and allowsthem control over their practice. It lets nurses extend their influence beyond their unit walls andpermits staff in the leadership team to share in thedecision making process.”Shared governance modelNursing qualitycouncilNursing leadershipcouncilNursing retentionand recognitioncouncilPatient and familyNursing practicecouncil includingUBCsProfessionaldevelopment councilNursing informaticscouncilNursing EBP andresearch councilThe model illustrates the structure of sharedgovernance at LGH. Note that the patient andfamily appear at the center of the model.The shared governance model at LGH keepsthe patient and family as the central focus, withunit-based councils and evidence-based practiceson the second tier, followed by other councils andcommittees that funnel up through the coordinating council. The acuity-tool advisory committeebegan the process for developing an acuity toolby identifying key stakeholders, including man-Who, what, when, where, and whyAn educational program sponsored by Cerner, “Using Acuity: Optimizing Patient Care and Nursing Workload” was held December4, 2015, at Lowell General Hospital, a large, non-profit, 424-bed community hospital in Lowell, Massachusetts. The aim of theprogram was to stimulate a national conversation on using acuity to optimize patient outcomes and nurse staffing.ModeratorLillee Smith Gelinas, MSN, RN, FAANEditor-in-Chief, American Nurse TodaySystem Vice President and ChiefNursing OfficerClinical Excellence ServicesCHRISTUS HealthIrving, TexasPanelistsAndrea Erickson, MSN, RN, CNMLFormer Director of Inpatient CriticalCare ServicesLowell General HospitalLowell, Massachusettswww.AmericanNurseToday.comAmy L. Garcia, MSN, RNDirector and Chief Nursing OfficerWorkforce and Capacity ManagementCerner CorporationKansas City, MissouriMiriam Halimi, DNP, MBA, RN-BCVice President and Chief NursingInformatics OfficerTrinity HealthLivonia, MichiganEileen T. Lake, PhD, RN, FAANJessie M. Scott Term Chair in Nursingand Health PolicyAssociate Professor of SociologyAssociate Director, Center for HealthOutcomes and Policy ResearchUniversity of Pennsylvania School of NursingPhiladelphiaWilliam Dan Roberts, PhD, ACNPData and Analytics ScientistAssistant Clinical Professor, School ofMedicine, Biomedical InformaticsAssistant Clinical Professor, School of NursingStony Brook MedicineLong Island, New YorkMarch 2016American Nurse Today29S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGboth nursing and healthcare dollars. Becausenursing salaries are the largest operational expense in acute care, many organizations consider cutting nursing positions when they have toreduce costs.At the same time, though, it’s an exciting timefor nursing. One example is the electronic healthrecord (EHR), which makes rich clinical dataavailable; computer analysis of this data offersbetter decisional support for nurses.Panel leaders were asked to share their expertise on patient acuity-adjusted staffing, exploringthe question: How do we ensure patients get thecare they need while creating a safe, effectivework environment for nurses?Before introducing the first speaker, Gelinasdiscussed the problem of variations in definingand implementing acuity-adjusted staffing in themore than 5,600 hospitals across the country. Forthe purpose of this panel discussion, she definedacuity as the individual patient’s need for care.
S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGagement, educators, informatics experts, and staffRNs across both campuses. (See Key stakeholders.)The aim, Erickson said, was to include individualswith varied levels of experience who worked varied shifts.Key stakeholdersErickson explained, “We used the Johari windowconcept to identify stakeholders based on two parameters — interest and power. We focused onthose who fell into the high-interest, high-powersection of the grid.”The committee then conducted a survey to determine which indicators determined high acuityand which warranted 1:1 or 1:2 nursing care. After the survey was completed, the committee developed a task force of nursing administrators,informatics experts, educators, and 6 to 10 staffRNs who met and communicated regularly. Erickson remarked, “We relied heavily on email andone-to-one meetings in both ICUs to identify bestpractices related to patient acuity, whether theywere practices occurring in Massachusetts or other states with mandated safe staffing ratios.” Theorganization maintained quality reporting, including central line–associated bloodstream infection rates, catheter–associated urinary tract infection rates, and pressure ulcer and patient fallsincidence.Erickson stressed the importance of seeking tounderstand how these changes affect work areas,resources, and staff educational needs. “Changetakes hard work and requires engraining the culture,” she pointed out. “This kind of project has tobe nurtured and grown from beginning to end.”She emphasized the necessity of preserving nursing’s voice in the process. “At the end of the day,we want an acuity-tool system that fulfills requirements of the law, but we don’t want to lose nursing judgment along way,” she said. “We muststrike a balance between science and judgment,marked by open dialogue, trust, and teamwork.”30American Nurse TodayVolume 11, Number 3Acuity-adjusted staffing linkedto better outcomesEileen T. Lake, PhD, RN, FAAN, JessieM. Scott Term Chair in Nursing andHealth Policy at the University ofPennsylvania School of Nursing, presented research on acuity-adjustednurse staffing as it relates to preterm infant outcomes. Among the 912 neonatal ICUs (NICUs) in theUnited States, sizable variations in mortality existthat can’t be attributed to infant factors, Lake said.The goal of measuring acuity-adjusted staffingwas threefold, Lake explained, “First, to look at howinfant acuity relates to the assignment a nurse receives. Second, to see how accounting for acuity andstaffing relates to infant outcomes. And third, tolook at how nurse workload relates to infant acuity.”Research shows staffing is significantly associated with infection among very low-birth-weight infants; 15% of these infants develop an infection,which in turn doubles their risk of mortality. Literature findings also reveal staffing influences the rateof breast milk at discharge. Across hospitals, aracial disparity in breast milk at discharge exists,linked to poorer staffing in hospitals with predominantly African-American patients. Of particularnote, hospitals with a largely minority populationhad higher rates of infection and discharge withoutbreast milk. They also had a higher degree of nurseunderstaffing and poorer practice environments.Lake said that across the acuity spectrum, all ofthe infants had similar parent needs, includingteaching, emotional support, and developmentalsupport. “We observed that when nurses care formultiple low-acuity infants, if you add events andparent needs together, their workloads are actuallyhigher than those of nurses who care for one ortwo high-acuity infants,” she noted. “This shows usthat acuity has a significant relationship withstaffing and outcomes but doesn’t account completely for workload.”Lake went on to discuss the need for adequatedecisional support in the NICU setting, includingacuity assessment systems that apply to that setting, as well as the need to ensure that these systems are evidence based.Acuity calculation driven bynursing documentationMiriam Halimi, DNP, MBA, RN-BC,vice president and chief nursing informatics officer at Trinity Health inLivonia, Michigan, discussed the importance of using an electronic healthsystem that’s integrated with nursing documentation. According to Halimi, this helps ensure thatacuity-level calculation doesn’t come at the cost ofdirect nursing time. “We hypothesized that an acuwww.AmericanNurseToday.com
cal critical-care evaluation depicting how an acuityscore is generated based on the nursing interventions classification and nursing outcomes classification (NOC). “For instance, in the respiratory domain, a patient on room air would be considereduncompromised and receive a score of 5. But a patient on a ventilator would be considered severelycompromised, with a score of 1,” she explained.“The lower the score, the more severely deviatedthe patient is and the more nursing care he or sheneeds. Therefore, the level of acuity is higher.” Thesystem calculates acuity scores every 4 hours, withscores generated 2 hours before shift change, to ensure the most updated scores. This helps identifyappropriate staffing for the next shift. (See Nursingdocumentation and acuity levels.)How does an integrated acuity system work? Byentering and saving clinical documentation inthe EHR, which is sent automatically to the acuitysolution. The acuity solution maps the observations and values using the NOC and indicatorvalues. Mapping of the clinical documentation isassigned to a domain (each domain has multipledata elements), which identifies the patient’s acuity assessment within that domain.As Trinity leaders evaluate implementation ofthe acuity tool, Halimi said, they’re looking atNursing documentation and acuity levelsReprinted with permission from Cerner Clairvia www.AmericanNurseToday.comMarch 2016American Nurse Today31S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGity system that’s electronic and integrated withnursing documentation will create better and timelier information, leading to better decisions thatoptimize both the process and practice of nursingcare,” she said. “We’re looking to leverage an acuity solution that will allow for flexibility and provide the information needed in real time to supportnursing down to the unit level.”Trinity Health, new to using an integrated acuitysolution, successfully implemented a solution within a 6-month period at one of its hospitals in fall2015; a second hospital is scheduled to go live withits solution this spring. While nursing leadershipdebated whether all nurses should have access tothe tools, ultimately they decided that was the bestway to go. Halimi said this approach providesgreater transparency.The Trinity Health planning team focused onkeeping staff nurses engaged throughout theprocess by: using scheduling and acuity solutions togetherto provide powerful tools that empower nurses giving staff nurses access to acuity tools, as wellas education on how to use them leveraging the role of a patient-outcomes expert toensure partnership in the use of acuity tools daily.Halimi showed a screenshot of a medical-surgi-
S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGStaffing: Financial to operationalmeasuring such outcomes as staffing expenses,staff and patient satisfaction, and productivity.“Acuity matters with or without the [nursestaffing] law,” Halimi concluded, pointing outthat acuity-adjusted nurse staffing holds importance whether or not it’s mandated by legislation.“An integrated acuity solution creates accuracyand precision in staffing, ultimately moving toward positive patient outcomes.”Balanced staffing: Wherefinance and operationsconvergeWilliam Dan Roberts, PhD, ACNP,data and analytics scientist at StonyBrook Medicine in Long Island, NewYork, moved the discussion in anotherdirection. He addressed how patient acuity affectsnurse staffing from both a financial and an operational perspective. He stressed the dynamic natureof patient acuity, stating, “It changes by the minute,by the hour, by the shift, so you want to make sureyou’re able to be flexible with your staffing.”Staffing is more than just allocating full-timeequivalents (FTEs) during a budgeting process,Roberts said. Considering the FTE allocation thathas been allotted is important. This includesachieving a balanced schedule based on how nurs32American Nurse TodayVolume 11, Number 3es and unlicensed assistant personnel are scheduled. From this, the allocated skill mix for the dayis available for assigning to patient needs.Roberts posed a pertinent question: How can apatient’s needs be best matched with the nurse’sskills to allow for the best nursing care, while stillmeeting the expected care processes and outcomes necessary for efficient and cost-effectivehealthcare delivery? To view his formula forachieving this, see Staffing: Financial to operational.The forms above show the usual financial allocation of staff during the budgeting process. Theyincorporate Roberts’ staffing formula, which includes assignment, RN competency, and patientacuity. The staffing formula relies on operationaland financial flexibility.Roberts showed a screenshot of a nurse-staffingdocument depicting a breakdown of the nursingworkload on a general medicine unit during theday shift, illustrating the effect of patient acuity onnursing care hours. “Predictably, we can ask, whatis the nursing work going to be for that patient?Does the nurse have a balanced workload? Howdo we achieve that? We would reallocate resourcesso that nurse is able to carry the load,” he said.Roberts went on to explore differences in demand between the medical ICU (MICU) and themedical intermediate care (MICR) unit, with awww.AmericanNurseToday.com
Patient acuity: Realizing theclinical potentialAmy L. Garcia, MSN, RN, directorand chief nursing officer for workforceand capacity management withCerner Corporation, spoke about theexciting potential for patient acuitydata to promote efficient, cost-effective care withbetter patient outcomes. She discussed the use ofacuity to inform the assignment of nurses to patients, as well as levels of care. She highlighted thiswith an example of a patient who was beingtreated for a myocardial infarction. Garcia explained that a patient who follows the typical re-covery trajectory might be ready for transfer fromthe ICU to a step-down unit after about 50 hours,then discharged home after about 30 hours of careon a telemetry or step-down unit.Taking patient variance into account, Garciapointed out, a patient who recovers more quicklythan expected may be a low-acuity outlier on anICU. Likewise, a patient who recovers more slowlythan expected may be transferred to a lower levelof care, resulting in the nurse having a largerworkload than he or she can manage in a settingmeant for lower-acuity patients.Garcia discussed the positive effect of aligningacuity with adjusted nursing hours per patient day,which promotes budget neutrality and optimizesnurse-to-patient assignments. Garcia noted thatnurse-to-patient assignments are often made by dividing the available nursing hours by the numberof patients and assigning the nurse to a number ofbeds or a geographic area. However, this practiceignores fundamental questions: How many hoursof care does an individual patient need to progresstoward optimal outcomes? Can that care be delivered on this unit? And which nurse is best suited toprovide that care? Garcia showed an illustration ofa system that provides visibility to the nursingworkload, adjusted for acuity, census, and activityon the unit (See Balancing workloads).Balancing workloadsReprinted with permission from Cerner Clairvia www.AmericanNurseToday.comMarch 2016American Nurse Today33S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGslide illustrating a higher workload demand in theMICR unit. Data aggregated from acuity calculating tools created visibility that allowed more staffcoverage for the MICR unit by adding anothernurse to each shift. It also enabled leaders to advocate for additional unlicensed assistant personnelas well as support staff, such as physical therapyand respiratory therapy, for the MICR unit.Roberts closed with an encouraging message:Nursing and finance departments can work together to use the data effectively. He stressed the needfor objective measures and standard terminologyto ensure congruency among organizations.
S PECIAL R EPORT : ACUITY-ADJUSTED STAFFINGOne East Coast hospital she works with implemented acuity considerations to help balance nurses’caseloads. “The rate of staff who called out of theirshifts on med surg units dropped 42%,” Garcia said.“Nurses were able to see that their caseloads werebalanced and that when they came to work, theyhad a good opportunity to actually make a difference. That’s what we
Workforce and Capacity Management Cerner Corporation Kansas City, Missouri Miriam Halimi, DNP, MBA, RN-BC Vice President and Chief Nursing Informatics Officer Trinity Health Livonia, Michigan Eileen T. Lake, PhD, RN, FAAN Jessie M. Scott Term Chair in Nursing and Health Policy Associate Pro