Transcription
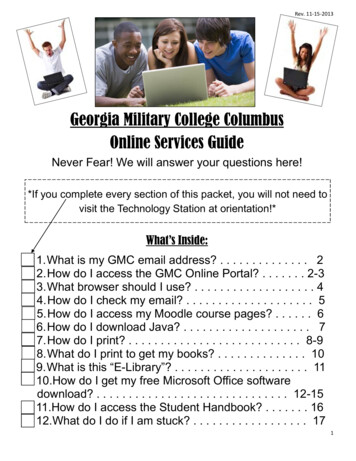
THEME ARTICLENeuro-OptometricRehabilitation AcceleratesPost-Concussion SyndromeRecovery in a ProfessionalAthlete – A Case ReportPresenting a New Paradigmpatient’s overall recovery from acquired braininjury. No system provides more neurosensoryinput to the brain than vision. Therefore,optometry has an obligation to and is bestprepared to provide this area of care referredto as neuro-optometric rehabilitation.Case Report: A professional soccer playerSteven J. Curtis OD, FCOVD, FNORA suffered a head injury during competition.Riverview Eye Associates, OhioHealth He was diagnosed with a mild traumaticRehabilitation Hospital, Columbusbrain injury (concussion) and was unable toCrew SCobtain complete resolution of symptomsdespite current standard return-to-playprotocol administered by the team medicalstaff. Symptoms included intermittent blurredvision during movement, mild photophobia,Abstractand feeling somewhat “not present”. TheBackground:Optometristsareteam medical staff included a sports medicinebecom ing increasingly instrumentalphysician, head athletic trainer/physicalin the care of brain injured patients.therapist, and a neuropsychologist. NeuroWithin the profession of optometry,optometric consultation was requested for thea segment of optometrists hasathlete by the team physician to determinebecome highly trained and skilled inif vision dysfunction was contributing torehabilitation of vision dysfunctionsthe athlete’s persistent symptoms. He wasand therefore is integral in thediagnosed with vision dysfunctions presumablyinterdisciplinary management of aassociated with the concussion and neurooptometric rehabilitation was prescribed.Correspondence regarding this article should beemailed to Steven J. Curtis OD, FCOVD, at curtisten@sbcglobal.net. All state ments are the author’s personalopinions and may not reflect the opinions of theCollege of Optometrists in Vision Development, VisionDevelopment & Rehabili tation or any institu tion ororganization to which the author may be affiliated.Permission to use reprints of this article must beobtained from the editor. Copyright 2017 College ofOptometrists in Vision Development. VDR is indexed inthe Directory of Open Access Journals. Online access isavailable at www.covd.org.Conclusion: The clinical findings and treatmentin a case of post-concussion syndromeinvolv ing associated vision dysfunctions aredescribed. Neuro-optometric rehabilitationuti l izing a unique paradigm remediated thevision dysfunctions of the athlete and elimin ated his post-concussion symptoms. This inturn facilitated his return-to-play process. Theparadigm applied began with passive, inputbased, bottom-up therapy accompanied bygradual introduction of active, output-based,top-down techniques. In recent years, thisauthor has found this paradigm to be moreeffective than a top-down approach whennon-oculomotor based vision dysfunctionsare included in the post-concussion patientclinical findings.Curtis SJ. Neuro-optometric rehabilitation acceleratespost-concussion syndrome recovery in a professionalathlete – a case report presenting a new paradigm.Vision Dev & Rehab 2017;3(3):168-78.Keywords: bottom-up therapy, neurooptometric rehabilitation, non-oculomotorbased vision problems, oculomotor-basedvision problems, optometric phototherapybased multisensory training, post-concussionsyndrome, return-to-play, top-down therapyVision Development & Rehabilitation167Volume 3, Issue 3 September 2017
backgroundConcussion is a mild traumatic brain injurythat can occur with or without the presence ofimpact to the head. It can result in anythingfrom loss of consciousness to impairedcognitive, functional, or physical abilities.Estimated incidence rates for concussion,according to the Centers for Disease Controland Prevention, range from a conservative300,000 per year to a more liberal and recentestimate of 3.8 million cases in the UnitedStates annually.1Post-concussion syndrome (PCS) is a setof symptoms that may continue for weeks,months, a year or more after a concussion.2,3The incidence of PCS varies, but most studiesreport that about 15% of individuals witha history of a single concussion developpersistent symptoms associated with the injury.A history of multiple concussions appearsto increase the risk for post-concussionsyndrome.4It is likely that many of these symptomsof PCS are, in part, a result of compromisedprocessing of sensory inputs, includingvisual.5 Recent research indicates that dueto widespread distribution of brain pathwaysdedicated to vision, vision-based performancetesting enhances sideline concussion assess ment.6 This would therefore promote earlierdetection and treatment of concussion whichin turn decreases the risk for developingPCS. According to Ellis, et al, the findingsof vestibular-ocular dysfunction at initialconsultation is an independent predictor forthe development of PCS in sports relatedconcussions of pediatrics.7A review of the literature reveals that thereis not a well-established, broadly-acceptedtreatment for PCS symptoms. There remainsa lack of evidence-based treatment strategies.However, some individuals benefit from severalinterventions depending on the particularpresenting signs and symptoms. The mostcommon treatment options that are effectiveconsist of medications, physical therapy, earlyVision Development & Rehabilitationeducation,8,9 cognitive behavioral therapy,10and aerobic exercise therapy.11 Research hasshown that optometric vision therapy shouldbe included in the overall treatment as itprovides improvement in post-concussionvision problems.12 Therefore, a neurooptometric rehabilitation evaluation can be aninstrumental component to the return-to-playprocess for an athlete.This paper will propose that optometricrehabilitation providers who treat PCS patientsshould identify whether the patient wouldbe best served utilizing a “top-down” or a“bottom-up” therapeutic approach. To helpmake this decision, a differentiation betweenoculomotor-based vision dysfunctions andnon-oculomotor-based vision dysfunctions ispresented which will help direct the providertoward the appropriate approach in each case.Neuro-optometric rehabilitation is atherapy service provided by specially trainedoptometrists which utilizes therapeutic prisms,lenses, filters, occlusion, and vision therapyto help stimulate visual pathways of the brainwhich are not functioning properly due to braininjury. Return-to-play refers to criteria that anathlete must satisfy before returning to play.The three conditions required are 1) asympto matic status at rest, 2) asymptomatic status withphysical and cognitive exertion, and 3) intactneurocognitive function (either compared tobaseline or normative data). Once the athleteis symptom free under these conditions, he orshe may return to full-contact training, thento competition. If symptoms return during fullparticipation, the athlete should return to aprevious stage of the return-to-play process.13Case ReportA 22-year-old white male professionalsoccer athlete was referred by his teamphysician for a neuro-optometric evaluation33 days post-concussion. The athlete had ahistory of one concussion three years priorfrom which his symptoms resolved completelyin five days. Persistent symptoms from his168Volume 3, Issue 3 September 2017
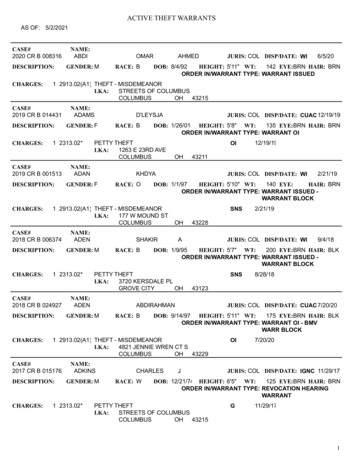
Table 1. Summary of clinical test results before and after treatment.TestUncorrected Visual Acuity atDistancePre-treatmentOD: 20/20OS: 20/25 (PH: 20/20)Presenting Spectacle RxNonePost-treatmentOD: 20/20OS: 20/25 (PH: 20/20)NoneRefractionOD: .25 -1.00 x 096OS: .75 -1.25 x 024Distance: OrthoNear: 3 esophoriaBase Out: x/12/10Base In: x/6/4Base Out: x/25/20Base In: 12 to blur4 BI/Plano: 0 cyc/30”8 BO/Plano: 3 cyc/30”8 BI/Plano: 3 cyc/30”15 BO/Plano: 4 cyc/30”7 cmOD: .25 -1.00 x 096OS: .75 -1.25 x 024Distance: OrthoNear: 2 esophoriaBase Out: x/18/16Base In: x/6/4Base Out: x/25/20Base In: x/12/104 BI/Plano: 2 cyc/30”8 BO/Plano: 6 cyc/30”8 BI/Plano: 6 cyc/30”15 BO/Plano: 6.5 cyc/30”6 cm / 7cmCover TestBar Vergences at DistanceBar Vergences at NearVergence Facility at DistanceVergence Facility at NearNear Point of ConvergencePopulation NormsNot applicableNot applicableNot applicableDistance: 1 exophoriaNear: 3 exophoriaBase Out: 9/19/10Base In:x/7/4Base Out: 17/21/11Base In: 13/21/13Not availableNot availableNear Point of Convergence(red/green)Stereo Fly at Near14.5 cm8 cmLess than 10cm80 seconds60 seconds40”Maddox Rod VerticalOrthoNot testedorthoAccomodative AmplitudeOD: 6 DOS: 5DOD: 11 DOS 10 DAge expected: 10.5 DAccomodative Facility /-1.50 6 cyc/30” OU6 cyc/30” OUNot availableGroffman Line Tracing37 points, age 12 (testmaximum)Reading Rate: 158 #’s/minFixations: R 122/100 #’sL 122/100 #’sSitting: 0-5 degrees leftStanding: 0-5 degrees left20/20 OU, no blur; no HA ornauseaOD: 19.5 degreesOS: 20 degreesExpected: age 12 (max fortest)Not available for # card0 points, age 7VisagraphReading Rate: 100#’s/minFixations: R 200/100 #’sL 198/100 #’sVisual Midline ShiftSitting: 0-5 degrees leftStanding: 10 degrees leftVestibular-Ocular Reflex using 20/25 OU, Slight blur; no HADynamic Visual Acuityor nauseaFunctional Visual Fields Blue OD: 17 degreesOS: 19.3 degreesTest of InformationVisual Modality: 21stProcessing SkillspercentileDelayed Recall: 63rdpercentileVEP amplitudes 32 x 32OD Hc 5.2uV Lc 4.2uVmonocular p100 patternOS Hc 4.2uV Lc 2.5uVreversal; Hc 85% Lc 15%Visual Modality: 50thpercentileDelayed Recall: 99 thpercentileNot applicableOD Hc 6.1uV Lc 3.5uVOS Hc 5.4uV Lc 2.8uVHc / 6uVLc not availablerecent concussion included intermittentblurred vision during movement and mildphotophobia. He further described feelingsomewhat “not present.” He denied difficultieswith reading, concentration, headaches,imbalance, dizziness, memory, hyperacusis,and diplopia.Interventions for the athlete prior tooptometric involvement included physicalVision Development & RehabilitationSitting: 0-5 degreesStanding: 0-5 degreesNo blur beyond static acuitylevel nor symptoms / 20 degreestherapy, aerobic exercise therapy, and chiro practic treatment. Although these interventionsprovided some benefits, his symptoms persist ed. Medical and neuropsychological testingwas essentially negative for pertinent factors.Diagnoses and PlanDiagnoses from the neuro-optometricevaluation (see Table 1 for supportive test data)169Volume 3, Issue 3 September 2017
Table 2. Summary of therapy techniques and order of use throughout the athlete’s vision rehabilitation program.Day1234Bottom-up Passive Therapy (in-office)Optometric phototherapy (OP) using one color,lateral canal vestibular stimulation, auditory trainingOP using three colors, posterior and anterior canalvestibular stimulation, auditory trainingOP using three colors, lateral canal vestibularstimulation, auditory trainingOP using three colors, posterior and anterior canalvestibular stimulation, auditory training5OP using four colors, lateral canal vestibularstimulation, auditory training6OP using four colors, posterior and anterior canalvestibular stimulation, auditory trainingOP using six colors, lateral canal vestibularstimulation, auditory training78OP using six colors, posterior and anterior canalvestibular stimulation, auditory training9OP using six colors, lateral canal vestibularstimulation, auditory training10OP using six colors, posterior and anterior canalvestibular stimulation, auditory training11OP using six colors, lateral canal vestibularstimulation, auditory training12OP using six colors, posterior and anterior canalvestibular stimulation, auditory trainingHOME THERAPY ONLY BEGINS13-30 home OP twice daily using one color; NO furthervestibular or auditory trainingTop-down Active Thearpy (in-office)monocular and binocular horizontal pursuitsmonocular and binocular vertical pursuitsmonocular and binocular horizontal pursuitsmonocular and binocular vertical pursuitsmonocular 4-corner wall saccades, clock dial saccades, Perconmazes level 1monocular and binocular horizontal pursuitsmonocular arrow wall saccades, clock dial saccades, Perconmazes level 1monocular and binocular vertical pursuits, monocular 4-cornerwall saccades, clock dial saccades, Percon mazes level 1binocular horizontal pursuitsbinocular arrow wall saccades, clock dial saccades andperipheral awareness, Percon mazes level 1binocular vertical pursuitsbinocular 4-corner wall saccades, clock dial saccades andperipheral awareness, Percon mazes level 2 /-.25 lens flipper at near2 BO and BI loose prism fusion at 15 ftbinocular horizontal pursuitsbinocular arrow wall saccades with tandem stance, clock dialsaccades and peripheral awareness, Percon mazes level 2 /-.50 lens flipper at near4 BO and 2 BI loose prism fusion at 15 ftbinocular vertical pursuitsbinocular 4-corner wall saccades with tandem stance, clockdial saccades and peripheral awareness, Percon mazes level 2 /-.50 lens flipper6 BO and 2 BI loose prism fusion at 15 ftbinocular horizontal pursuitsbinocular arrow wall saccades balancing on one foot, clockdial saccades and peripheral awareness, Percon mazes level 2 /-1.00 lens flipper8 BO and 4 BI loose prism fusionbinocular vertical pursuitsbinocular 4-corner wall saccades balancing on one foot, clockdial saccades and peripheral awareness, Percon mazes level 2 /-1.00 lens flipper8 BO and 4 BI loose prism fusionhead rotation pursuits and 4-corner saccades at trainingfacility while team trainer guided return-to-play exercise andgradual training advancementincluded convergence and accommodativedysfunctions which likely provided thesymptom of intermittent blurred vision;14,15pursuit eye movement dysfunction, saccadiceye movement dysfunction, visual midlineVision Development & Rehabilitationshift, and vestibular-ocular reflex (VOR)dysfunction contributed to the symptoms ofintermittent blurred vision and “not feelingpresent”;16,17,18 and constricted functional visualfields (green, red, blue) which contributed170Volume 3, Issue 3 September 2017
to both the “not feeling present” symptomand photophobia.19 Neuro-optometric rehab ilitation was ordered with the intent of theathlete regaining visual efficiency and sensorimotor skills for functional performanceimprovement applicable to his safety duringsoccer and daily life activities. Goals includedage-normed binocular vergence ranges,accommodative efficiency and flexibility, ageappropriate oculomotor skills, midline shiftto 5 degrees or less while standing, and nonconstricted functional visual field each eye.All members of the team medical staff (headphysician, neuropsychologist, and athletictrainer/physical therapist) and this authorwould then convene at the training facility tore-establish a plan of care appropriate for theathlete’s return-to-play process. The athletictrainer would execute this return-to-playworkout protocol while in collaboration withhis continued vision rehabilitation program.Treatment and OutcomesThe athlete’s vision rehabilitation tookplace daily for 34 days and was comprisedof saccade and pursuit oculomotor activities,vergence therapy, optometric phototherapy(syntonics), vestibular stimulation, and multisensory integration training. It consisted of 12days of in-office therapy followed by 22 daysof home therapy. Initial emphasis of therapywas passive utilizing optometric phototherapy,auditory training, and vestibular stimulation.Active therapy was minimal initially consistingof 5-10 minutes of monocular saccadic andpursuit oculomotor activities. Convergencetherapy was gradually introduced as toleratedwithout aggravating symptoms. The saccadic,pursuit, and vergence activities increasedin difficulty during the in-office phase oftreatment, see Table 2. Balance activitieswere gradually added to further rehabilitateintegration of sensorimotor pathways.On day number seven, the athlete was seenfor a progress evaluation. Although he reportedthat he had been experiencing symptoms ofVision Development & RehabilitationFigurecolorfieldfieldresults(blue, (blue,red, green)Figure1:1: FunctionalFunctionalcolorresultsred,one day prior to initiation of therapy.green) one day prior to initiation of therapy.headache and fatigue during the first threedays, now he was tolerating the therapy well.Clinically, he demonstrated improved vergenceamplitudes at distance (BO x/15/12, and BIx/6/4), vergence facility at distance (8 BO/pl: 3cyc/30”), near point of convergence (red/green:10.5cm), and amplitude of accommodation(OD 9D, OS 8D). Additionally, his functional(color) visual fields expanded (see Figures 1and 2). General consensus amongst optometricphototherapy providers is that when a smalltarget is used (e.g. 1-2mm diameter), theexpected color field sizes are a minimum of20, 15 and 10 degrees for blue, red and green,respectively.20 However, these should onlybe considered general guidelines by visionrehabilitation clinicians. There are severalvariables that impact performance on color171Volume 3, Issue 3 September 2017
Figure 2:colorfield fieldresultsresults(blue, ed,onday number 13 of therapy.green) on day number 13 of therapy.field testing, such as, patient fatigue, sensitivity,time of day, test environment, stimulus sizeand speed of presentation, and more.21 Thisis likely the reason that the literature lacksestablishment of definitive norms for functionalvisual fields. Moreover, therapy goals shouldinclude an expansion of color fields relative topre-therapy. This provides the clinician a toolto monitor the effectiveness of the prescribedlight and to make modifications if indicated. Asshown in Figures 1 and 2, the athlete’s blue colorfields (average of eight meridians) improved42% in right eye and 28% left eye indicatingthe current light sequence was appropriate tothis point.Home therapy activities were added and hecontinued coming for daily in-office sessions.Vision Development & Rehabilitation172Home therapy consisted of BI and BO prismfusion at 15 ft. progressing from 2BI/2BO to4BI/8BO over several days. Additional hometherapy included /- .25 and then /-.50 lensflippers at a 20/30 near point target.On day number 13, the athlete was seenagain for a brief progress evaluation. Hestated that his blurred vision had completelyresolved. He was very pleased with improvedperception of his location in space andretrospectively realized this was what causedhim problems when trying to play duringinitial return-to-play protocol prior to beingreferred for neuro-optometric management.Clinically, he had been gradually advancingin performance of therapeutic vergence andaccommodation activities without increasedsymptoms. Treatment was transitionedfrom in-office to home-based optometricphototherapy combined with oculomotoractivities at the team training facility assistedby the athletic trainer, under this author’sdirection. All providers of the team medicalstaff, including this author, convened theday after this appointment to collaborativelydetermine his continued plan of care.Communication continued by phone or textnearly every day over the next three weeksregarding his progress. During this period,minor adjustments were made to his homevision rehabilitation activities to graduallyincrease therapy complexity.Thirty-four days after initiation of therapy,the athlete was seen for an extensive visionrehabilitation progress evaluation. He statedhis “vision is fantastic” and he felt “fullypresent”. His photophobia had resolved. Allclinical testing revealed findings either at ornear goals as shown in the post-treatmentcolumn of Table 1. These findings wereshared by phone consultation with the teamphysician and resulted in a decision that theathlete would resume return-to-play protocol.Goals included partial game participation in11 days and full game participation in 18 daysif symptoms remained absent. The athlete’sVolume 3, Issue 3 September 2017
vision rehabilitation was discontinued andhe was advised to return for monitoring infour weeks. At that evaluation he remaine
Rehabilitation Hospital, Columbus Crew SC Correspondence regarding this article should be . with reading, concentration, headaches, imbalance, dizziness, memory, hyperacusis, . table 2. summary of therapy techniques and order of use throughout the athlete’s vision rehabilitation progra