Transcription
STANDARD NURSEPROTOCOL FORDIABETES MELLITUSIN ADULTSFunding Source for Development of this Nurse Protocol: CDC CooperativeAgreement DP13-1305 State Public Health Actions.
THIS PAGE INTENTIONALLY LEFT BLANK
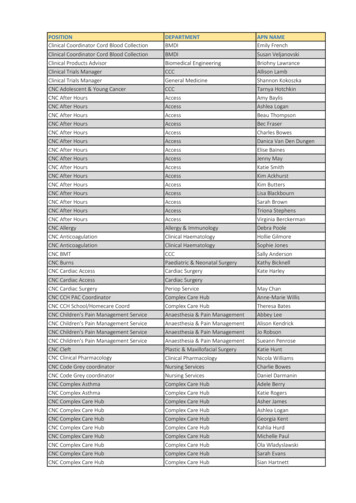
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20162015 DIABETES MELLITUS CLINICAL REVIEW TEAMPatricia Jones, RNChronic Disease Prevention SectionGeorgia Department of Public HealthJean O’Connor, JD, DrPHChronic Disease Prevention DirectorGeorgia Department of Public HealthStephen Goggans, MD, MPHDistrict Health DirectorEast Central Health DistrictMedical ConsultantAllison Smith, MPH, CHESPolicy, Program, and Planning Analyst:Diabetes and VisionGeorgia Department of Public Health,Chronic Disease Prevention SectionWilliam R. Grow, MD, FACPDistrict Health DirectorSouth Health DistrictMedical ConsultantTammy Burdeaux, RN, BSN, CRNIDistrict Nursing and Clinical CoordinatorEast Central Health DistrictKelly Knight, RN, BSNClinical Nursing CoordinatorSouth Central Health DistrictKimberley Hazelwood, Pharm DDirector of PharmacyGeorgia Department of Public HealthRejani T. Rajan, PharmDPharmacy Disaster ResponseCoordinatorGeorgia Department of Public HealthDivision of Health ProtectionGreg French, RD, LD, CPTDeKalb County Board of HealthPenny H. Conner RN, BSNState Immunization Nurse ConsultantGeorgia Department of Public HealthTonia Parrott, Ph.D, MT (ASCP)Clinical Microbiology Services DirectorGeorgia Public Health LaboratoryGeorgia Department of Public Health
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016Atlanta, GATHIS PAGE INTENTIONALLY LEFT BLANK
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016TABLE OF CONTENTSDIABETESDiabetes Mellitus in AdultsAppendix A:Clinical Tasks in Care of Patient with DiabetesAppendix B:Clinical Tasks in Follow-up Care of Patient with DiabetesAppendix C:Treatment Algorithm for Type 2 DiabetesAppendix D:Summary of RecommendationsAppendix E:Correlation between A1C and Plasma Glucose LevelsAppendic F:Management of Lipids in Patients with DiabetesAppendix G:Educational Resources1717.117.2917.3117.3317.3517.3717.3917.43
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016THIS PAGE INTENTIONALLY LEFT BLANK
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016STANDARD NURSE PROTOCOL FORDIABETES MELLITUS IN ADULTSDEFINITIONDiabetes mellitus is a group of metabolic diseases characterized byhyperglycemia resulting from defects in insulin secretion, insulin action orboth. Diabetes is characterized by fasting plasma glucose (FPG) equalto or greater than126 mg/dL or random plasma glucose equal to orgreater than 200 mg/dL (with testing on two separate days)accompanied by symptoms. Symptoms of diabetes mellitus arefrequently due to the osmotic diuresis associated with hyperglycemia.Complications of diabetes may be acute and/or chronic. Acutecomplications include: hyperglycemia, hypoglycemia, diabeticketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome(HHS). The chronic complications of diabetes are most often the result ofsustained hyperglycemia and include damage, dysfunction and failure ofvarious organs, such as eyes, kidneys, nerves, heart and vascularsystem.ETIOLOGYType 1 Diabetes Mellitus1.Cause: inadequate or absolute lack of insulin productionsecondary to destruction of the pancreatic Beta cells. Individualsare dependent on exogenous insulin for survival. Type 1comprises less than 10% of all cases of diabetes.2.Contributing factors:a.b.Autoimmune mediated response.Idiopathic (No evidence of autoimmunity is present).Type 2 Diabetes Mellitus1.Cause: combination of insulin resistance and/or inadequateinsulin production. Increased hepatic glucose productioncontributes to elevated fasting blood glucose levels. Insulinresistance in the liver and muscle and impaired insulinsecretion also contribute to hyperglycemia.2.Risk factors:a.b.c.d.Overweight - BMI equal to or greater than 25 kg/m2 andBMI equal to or greater than 23 kg/m² for AsianAmericans.Waist circumference greater than 102cm (40 inches) formen and greater than 88cm (35 inches) for women.Sedentary lifestyle, such as sitting for more than 90minutes at a time or little to no moderate to vigorousactivity in the past 30 days.Age equal to or greater than 45 years old.Diabetes17.1
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016e.f.g.h.i.j.k.l.m.First degree relative with diabetes.Race – African-American, Latino, Native American, Asianand Pacific Islander at greater risk.History of large birth-weight babies – greater than 9pounds or history of diagnosed with gestational diabetes.History of A1C equal to or greater than 5.7%, impairedglucose tolerance- 2 hour plasma glucose in 75 –g OralGlucose Tolerance Test of 140 mg/dL to 199 mg/dL orfasting plasma glucose of 100 mg/dL to125 mg/dL.Hypertensive -blood pressure equal to or greater than140/90 mmHg or on therapy for hypertension.HDL cholesterol level less than 35mg/dL and/ortriglyceride level greater than 250mg/dL.Women with polycystic ovary syndrome.Clinical conditions associated with insulin resistance,such as severe obesity and acanthosis nigricans.History of cardiovascular disease.Prediabetes1.2.3.4.5.6.7.Patient’s blood glucose levels do not meet criteria fordiagnosis of diabetes but blood glucose levels are higherthan what is considered normal glucose levels.Patients who should be screened are those at any age whoare overweight or obese (BMI equal to or greater than 25kg/m² or equal to or greater than 23 kg/m² in AsianAmericans) or present with the same risk factors for Type 2diabetes as listed in the preceding section.Patients are asymptomatic but at high risk for developingcardiovascular disease and diabetes.A1C is 5.7-6.4%Impaired fasting glucose is 100-125 mg/dL.Plasma glucose at 2 hour oral glucose tolerance test (75-gram)between 140-199 mg/dL is considered Impaired GlucoseTolerance (IGT).Impaired fasting glucose and IGT are not clinical entities butare risk factors for diabetes and cardiovascular disease andare associated with obesity, especially abdominal or visceralobesity, dyslipidemia, high triglyceride levels and/or lowdensity lipoprotein cholesterol, and hypertension.Gestational Diabetes (GDM)1.Patients who are pregnant, planning to become pregnant, orbreast-feeding must be referred to an obstetrician formanagement of diabetes.Diabetes17.2
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20162.3.4.5.SUBJECTIVE1.In the past, Gestational Diabetes was defined as any degreeof glucose intolerance that was first recognized duringpregnancy. It did not matter if the condition may havepredated the pregnancy or persisted after the pregnancy. If itpersisted post-pregnancy, it was re-classified according tothe diagnostic criteria.The epidemic of obesity and more type 2 diabetes in womenof child-bearing age has resulted in an increase number ofpregnant women with undiagnosed type 2 diabetes.It is now recommended that women with risk factors forType 2 diabetes be tested on the initial prenatal visit usingstandard diagnostic criteria.Women with diabetes in the first trimester are classified ashaving type 2 diabetes. GDM remains as diabetes diagnosedduring the second or third trimester when it is clear that it isnot overt diabetes.Patient history may or may not reveal the following:a.b.c.d.Symptoms of hyperglycemia-polyuria, polydipsia,polyphagia, blurry vision, extreme fatigue, slow healing,and or tingling, and pain or numbness in feet and hands(primarily type 2)Unexplained weight loss or gain.Previously diagnosed with “borderline diabetes” or prediabetes, gestational diabetes or impaired glucosetolerance.Past or current symptoms of coronary heart disease, heartfailure, cerebrovascular disease, peripheral vasculardisease, renal disease, gout or sexual dysfunction.2.The patient, primarily those with type 2 diabetes, may beasymptomatic. Elevated glucose levels are often foundin routine lab work, during evaluations for surgery or work-up forother conditions. Patients suspected to have type 1 diabetes mayreport rapid onset of symptoms.3.There may or may not be a family history or obvious risk factors.4.The following should be assessed and documented in chart:a.Current diabetes self-management routine, if previouslydiagnosed, to include:1)2)Duration of diabetes, including age andcharacteristics of onset, such as diabeticketoacidosis (DKA) or asymptomatic.Current and prior medications for diabetes.Diabetes17.3
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20163)b.c.d.f.g.h.i.j.k.l.OBJECTIVE 1.Eating patterns, weight history, and nutritionalstatus.4)Prior self-management education/training.5)Self-monitoring of blood glucose (SMBG) patternand results and A1C results if available.6)Current physical activity-type, frequency,duration.7)Frequency of usage and indications for OTCmedications, prescriptions, and alternativemedications, home remedies, nutritionalsupplements.Acute complications-severe hyperglycemia, DKA,severe hypoglycemia requiring assistance of another,hypoglycemia unawareness. Prior emergency roomvisits and hospitalizations related to diabetes.History of infections-type, treatment, resolution time.Family history of diabetes, chronic kidney disease, prematurecardiovascular disease.CHD risk factors-hypertension, abnormal lipids, highsodium intake, tobacco use, prior myocardialinfarction, coronary revascularization, heart failure,stroke, transient ischemic attacks, peripheral arterialdisease, sleep apnea.History of target organ damage: retinopathy (visualdisturbances/changes- loss or fluctuation of visualacuity, blurry vision, floaters or history of cataracts,macular degeneration, or ophthalmic procedures);nephropathy (history of renal disease, ankle edema,fatigue, hypertension); peripheral (stocking and glovepattern of numbness, tingling, pain or weakness)and/or autonomic neuropathy (resting tachycardia,fixed heart rate, postural hypotension, syncope,urinary frequency, urgency, incontinence, male orfemale sexual dysfunction, gastrointestinal complaintssuch as nausea, vomiting, early satiety, abdominalbloating, and weight loss.).History of foot ulcers and deformities.Psychosocial and social situation, including economicfactors.Smoking or other tobacco use including e-cigarettes,alcohol and recreational drug use.Female reproductive history: menstrual history, method ofcontraception, pregnancies and outcomes.Current immunization status.Physical examinationa.AppearanceDiabetes17.4
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20161)2)b.c.d.e.f.g.h.i.j.k.l.m.2.Type 1 Thin, ill appearance, dehydrated, may havehad significant weight loss.Type 2 Frequently overweight or obese.Height, weight and BMI.Routine assessment of blood pressure (standing andsitting or sitting and lying) to assess for dehydration andautonomic neuropathy. Blood pressure may be greaterthan 140/90 mmHg.Extremities - assess patient extremities for changes incolor, deformity, injury, sensation, temperature changes,muscle strength and deep tendon reflexes (use a 128-Hztuning fork and a monofilament).Mouth - assess for gum problems, tooth decay and oralcandidiasis.Visual acuity-assess using Snellen Chart.Arterial Pulses – Palpate and auscultate pulses.Neurological and foot examination includinginspection, palpation of dorsalis pedis and posteriortibial pulses, nails for thickening, signs of fungal orbacterial infections, and signs of compromised bloodflow. Assess for decreased or absent deep tendonreflexes, numbness or burning sensation or sensoryloss may be present.Neck - Palpate the thyroid for an enlarged thyroid. Assessfor hoarseness and difficulty swallowing.Skin - Inspect for sites of previous insulin injections, shinyspots over tibial bones, loss of hair over lower legs andtoes, ulcerations of feet/legs, carbuncles and ulcers,lipohypertrophy or lipoatrophy at insulin injection sites. Intype 2 diabetes early hyperinsulinemia may beevidenced by Acanthosis Nigricans around the neck,waist, inguinal and axillary skin folds (dark velvetyhyperpigmentation).Cardiovascular – Auscultate the heart for heart rate, rhythmand sounds. Assess for orthostatic hypotension,hypertension, decreased capillary refill, absent pedalpulses, impaired circulation.Abdomen - Perform abdominal exam. Palpate for anenlarged liver.Inspect the hands for mobility and deformities.Diagnostic laboratory findings (Non-Pregnant Adults)a.b.Confirmed A1C equal to or greater than 6.5%ORConfirmed fasting plasma glucose level equal to orgreater than 126 mg/dL on at least two different occasions(on subsequent days).Diabetes17.5
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016c.ORConfirmed random plasma glucose level equal to orgreater than 200 mg/dL (with classic symptoms ofdiabetes), on two different occasions.ASSESSMENTDiabetes Mellitus (Type 1 or Type 2)PLANDIAGNOSTIC AND FOLLOW-UP STUDIESInform the patient of the importance of abnormal results and follow-upand referrals. If a service is not available in the clinic, the patient shouldbe given resource/referral information that must be appropriatelydocumented in the patient’s record. The patient’s follow-through on therecommendations should be documented at the next visit.1.2.3.4.5.6.7.8.9.10.11.12.13.A1C – Initially and every six months for well controlled patientson diet therapy or oral medication. Every three months for patientspoorly controlled or when medications have been changed. A1Ctarget goals should be individualized based on patientdesires, values, and willingness to participate inmanagement, potential risks of hypoglycemia and otheradverse events, patient’s age and duration of diabetes,comorbidities and established vascular complications.Treatment goal is generally 7%, however, any lowering ofA1C levels has benefit.Initial lipid profile. Lipid management is an integral part ofdiabetes management. Lipid management is addressed inappendix F.Metabolic profile initially and annually.Serum creatinine, potassium, and sodium or more frequentlybased on medication profile.ECG annually (or as indicated).Annual dilated eye exam.Spot urine for albumin to creatinine ratio.TSH as indicated by findings on physical examination orsuggestive history.Annual dental examination.Weight and calculation of BMI on each visit; height annually.Referral to other specialties and services as needed.Urine cultures as indicated. Urinalysis for ketones, protein andsediment.Refer women of reproductive age to Women’s Health.THERAPEUTICNON-PHARMACOLOGIC1.A patient-centered approach is highly recommended in thecare of patients with diabetes. It is defined in articles by theDiabetes17.6
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016American Diabetes Association (see references) as“providing care that is respectful of and responsive toindividual patient preferences, needs, and values andensuring that patient values guide all clinical decisions.”2.Diabetes Self-Management Education/T raining (DSME/DSMT)is considered an essential element for persons withdiagnosed diabetes. DSME/T provides the knowledge, skillsand support necessary for diabetes self-care. Refer to thePatient Education Counseling Section for specificcomponents of DSME and DSMT. For Medicarereimbursement, DSMT coding must be used.3.For patients with prediabetes, the goals are to decrease therisk of diabetes and cardiovascular disease through intensivelifestyle interventions through participation in lifestylechange programs to promote and maintain moderate weightloss (7%of body weight).a.b.c.4.Promote healthy food choices with consistency in dayto-day carbohydrate intake and the limitation ofsucrose-containing and high glycemic index foods.The Dietary Approaches to Stop Hypertension (DASH)Eating Plan can be used as a basis for meal planning tohelp manage blood glucose, blood pressure andcholesterol.Increase physical activity to at least 150 minutes perweek of moderate-intensity aerobic activity such aswalking.Patients with prediabetes should be referred to lifestylechange programs or Diabetes Prevention Programs.Nutrition Therapy-Evidence suggests that there is no idealpercentage of calories from carbohydrate, protein and fat forall persons with diabetes. More emphasis is placed on apattern approach rather than specific macronutrient andmicronutrient recommendations. Macronutrient distributionshould be based on individualized assessment of currenteating patterns, preferences and metabolic goals. The goalsof nutrient therapy are:a.b.c.d.e.Promote and support healthful eating patterns.Attain glycemic, blood pressure and lipid goals.Achieve and maintain body weight goals.Delay or prevent complications of diabetes.Address individual nutrition needs based on personaland cultural preference, access to healthy foodchoices, willingness and ability to make behaviorchanges, and barriers to change.Diabetes17.7
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016f.g.5.Physical activity has been shown to improve blood glucosecontrol by decreasing insulin resistance and increasingmetabolism, reducing cardiovascular risk factors, contributingto weight loss and improved sense of well-being.a.b.c.d.e.6.Maintain pleasure of eating by providing positivemessages about food choices while limiting foodchoices only when indicated by scientific evidence.Provide patients with practical tools for day-to-daymeal planning. A variety of meal planning tools, DASHEating Plan, Therapeutic Lifestyle Changes Diet, USDAChoose My Plate, Mediterranean style, and vegetarianand vegan eating plans may be used.Patients should reduce sedentary time by breaking upextended amounts of time (greater than 90 minutes)sitting.Adults should be advised to perform at least 150minutes per week of moderate-intensity aerobicphysical activity spread over at least 3 days per weekwith no more than 2 consecutive days withoutexercise.Adults should do muscle strengthening activities thatinvolve all major muscle groups 2 or more days perweek.Patients over the age of 65 or those with disabilitiesshould follow the above guidelines to the extentpossible, and if not possible, they should be asphysically active as possible.Consideration of existing diabetes related healthissues identified during the patient’s assessment, suchas cardiovascular disease, hypertension, peripheraland/or autonomic neuropathy, and microvascularchanges, should be considered when recommending aphysical activity program.Monitoringa.Self-Monitoring of Blood Glucose (SMBG):1)2)Used to assess effectiveness of meal plan,exercise and medication.Patients with Type 2 diabetes being treated withmedication should perform SMBG on a regular,consistent basis until blood glucose targets arereached. One example of a testing schedule isperforming a fasting and one other test duringthe day on an alternating routine, such as preDiabetes17.8
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20163)4)5)meal testing on alternate days (pre-lunch oneday, pre-evening one day and at bedtime on thethird day). If fasting and pre-meal values arewithin target values but A1C values do notcorrelate, post-prandial blood glucose valuesmay provide guidance in reviewing compositionand portion sizes of meals. Once 50% of bloodglucose values are within target blood glucoserange, SMBG frequency can be modified totreatment (e.g., meal planning only, 2-3 times perweek; oral medications once per day onalternating fasting and pre-meal schedule).Frequency of monitoring may depend onpatient’s willingness and physical ability toperform SMBG, financial resources, comorbidconditions and ability to take action whenabnormal values occur.Individualized target blood glucose ranges arebased on treatment regimen, age, and presenceof complications such as hypoglycemiaunawareness. The recommended target goals formost patients: pre-meal glucose between 80-130mg/dL and peak post-prandial glucose less than180mg/dL. Discuss target glucose levels with thepatients and have them write down their targetglucose levels in their logbook.The patient’s SMBG records should be reviewedon each visit to identify patterns of bloodglucose levels to consider adjustments in themanagement plan. Provide the patient withfeedback to support and encourage continuedmonitoring as well as behavior and lifestylechanges.Additional testing may be indicated during timesof stress, especially infection/illness.b.A1C testing, which reflects average blood glucoseconcentration over the past 90-120 days, should beperformed at least two times per year in patientsmeeting target treatment goals and quarterly inpatients whose therapy is changed or who are notmeeting treatment goals. Reduction of A1C to 7% orless has been shown to reduce microvascularcomplications and long-term reduction inmacrovascular disease.cWeight monitoring-Weight loss has been shownbeneficial for persons with diabetes, particularly type 2diabetes, to reduce insulin resistance. NutritionalDiabetes17.9
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016inventions and increase physical activity can promotecontrolled weight loss. Unintentional weight loss mayoccur as a result of uncontrolled hyperglycemia orother underlying causes. Weight gain should bemonitored and possible reasons explored, such asmedications and need for additional nutritionalcounseling.d.Regularly assess for cardiovascular risk factors andthe presence of macrovascular disease.1)2)See Appendix F for lipid management guidelines.Monitor blood pressure and insure thathypertension is being treated to target goal ofsystolic blood pressure less than 140 mmHg anddiastolic blood pressure less than 90 mmHg.3)Assess for symptoms of macrovascular disease:a)chest painb)decreased tolerance for physical activityc)chronic fatigued)shortness of breathe)swelling of feet and anklesf)sudden numbness or weakness on oneside of the bodyg)inability to walk or weakness, paralysis onone side of the bodyh)pain in the calves when walking or pain infeet when at resti)coolness of lower extremitiese.Smokers, e-cigarette users, or other nicotine usersUtilize Ask, Advise and Refer (AAR) model and providecessation counseling and referral to the Georgia QuitLine 1-877-270-STOP (7867) using the Quit Line FaxBack Form as appropriate.f.Foot evaluation and care-Early recognition andappropriate management of patients with insensatefeet is important to reduce risk of amputation.1)All patients with diabetes should have an annualcomprehensive foot examination as described inthe Objective Section. Patients with insensatefeet, foot deformities, ulcers and complaints ofnumbness and/or burning, should, at minimum,have a visual inspection of their feet at eachvisit.Diabetes17.10
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20162)All patients should receive general foot careinstructions. Patients with neuropathy, insensatefeet, history of foot ulcers, or deformities as wellas those with visual impairment, should be givenenhanced foot care instructions and/or referralto a specialist or podiatrist. See PatientEducation/Counseling Section for additionalinformation.g. Psychological assessment and care-Depression is notuncommon in persons with diabetes and may affect apatient’s ability to perform self-management activities.1)2)3)Patients should routinely be asked how diabetesand its care is impacting their lives, if they arefeeling anxious, down or helpless, changes insleep patterns, and additional financial burden ofdiabetes.The Patient Health Questionnaire (PHQ)-9 is abrief depression self-report scale that is a usefulscreening tool and can be found at:http://phqscreeners.com/pdfs/02 PHQ9/English.pdf.Referral to mental health resources may beappropriate for patients who might benefit from amore comprehensive evaluation and when poorglycemic control persists despite ongoingadjustments in management regimen.h.Dental patients with diabetes, especially if poorlycontrolled, are at greater risk for periodontal disease.This can lead to difficulty chewing, pain, possible lossof teeth, and persistent bad breath. Patients shouldbrush and floss daily, regular visits to a dentist, goodglucose control, and avoidance of tobacco products.i.Immunizations are important preventive services forpersons with diabetes to reduce diabetes-relatedhospitalizations and to prevent morbidity and mortality.1)2)3)4)Provide routine vaccinations as for the generalpopulationAnnual flu vaccinationsAdminister pneumococcal poly-saccharidevaccine23 (PPSV23) to all patients with diabetesAdults 65 years of age or greater, if notpreviously vaccinated should receivepneumococcal conjugate13 (PCV 13) vaccineDiabetes17.11
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses20165)6)followed by PPSV23 within 6-12 months afterinitial vaccination.Adults 65 years of age or greater, if previouslyvaccinated with PPSV23 should also receive aPCV13 vaccine no sooner than 12 months afterreceiving PPSV23.Administer hepatitis B vaccine to unvaccinatedadults, aged 19-59 years, with diabetes. Consideradministering hepatitis B vaccination at thediscretion of the treating clinician tounvaccinated persons aged equal to and olderthan 60 years.Pharmacologic- Diabetes Medication Management, Type 2 DiabetesIn patients with markedly symptomatic and/or elevated blood glucose levels( 300-350 mg/dL) or A1c ( 10-12 %) consider initiating insulin therapy. If insulintherapy is indicated please refer these patients to an outside provider.Note: Be familiar with local discount drug programs and keep an up-to-date list(may change frequently). To the extent possible, order medications from theselists. Consult with the delegating physician as appropriate.1.Monotherapy- Metformin is the preferred first agent, unless itis contraindicated or not tolerated.a.Biguanides: Metformin (Glucophage):Mechanism of action: Inhibits hepatic glycogenolysisand gluconeogenesis. Enhances insulin sensitivity inmuscle and fat.1)2)3)4)5)6)7)Efficacy: 1-1.5 % A1c; Greater effect onFPG PPGSide effects: Gastrointestinal , Lactic acidosis(rare), Vitamin B12 deficiencyContraindications: Avoid in renal impairment(Men: SCr 1.5 mg/dL, Women: SCr 1.4 mg/dL)Advantages: No weight gain, No hypoglycemiaCost: LowDosing: Take with meals; Due to GI side effectsstart once daily and titrate up as tolerated ( 500mg per week or 850 mg increases every 2 weeks)Elderly patients should not be titrated tomaximum doseDrugMetformin(Glucophage)DiabetesInitial Dose500 mgonce orMax Dose2000 mgSupplied500, 850,1000 mg tab17.12
Department of Public HealthStandard Nurse Protocols for Registered Professional Nurses2016twice dailywith mealsb.ER: 500, 750mg tabA sulfonylurea or meglitinide (see below) may be usedas first line therapy in patients unable to takeMetformin.Considerations: Consider adding additional agents if A1C goal is not reachedafter 3 months of monotherapy OR if A1C is equal to or greater than 9%. Pleasesee list below for additional agents.2.Dual therapy: Sulfonylureas, DPP-4 inhibitor, meglitinidesmay be added as second line therapy. Use appropriatemonitoring of FPG and A1C measurements to ensure that thepatient is not subjected to excessive drug exposure orincreased probability of secondary drug failure. If glucosetargets are not achieved after a suitable trial of combinationtherapy and lifestyle changes, consider discontinuing thesedrugs and refer to an outside provider for initiation of insulintherapy.a.Sulfonylureas (SU):Mechanism of action: Stimulates pancreatic insulinsecretion.1)First generation: Not recommended in currentguidelines (Chlorpropamide, Tolbutamide)2)Second generation agents: Glimepiride (Amaryl);Glipizide (Glucotrol); Glyburide (DiaBeta,Micronase).1)Efficacy: 1-2% A1c; PPG, reducedefficacy over time.2)Side effects: Hypoglycemia, Weight gain3)Contraindications: Avoid in poor renalfunctioni)Glimepiride: CrCl less than 30ml/minii)Glipizide: CrCl less than 10 ml/miniii)Glyburide: CrCl less than 50 ml/min4)Cost: Low5)Dosing: Do not cut/crush/chew ExtendedRelease (ER) formulations;i)Glimepiride daily dose may beincreased by 1-2 mg at weekly or biweekly intervals.ii)Glipizide doses greater than 15mg/day should be given in divideddoses. Extended Release is dosedonce daily. Titration of dose ifDiabetes17.13
Department of Public HealthStandard Nurse Protocols for Registered Professional cotrol)Glipizide XLneeded should be no morefrequently than every 7 days. Elderlypatients initial dosing of 2.5 mg andtitrating at 1 to 2 week intervals.Glyburide should be titrated asneeded at 2.5 mg daily at weeklyintervals. Use conservative initialand maintenance doses in elderlypatients.Initial Dose1-2 mg dailygive withfirst mainmeal5 mg onceor twicedaily 30minutesbeforemeals(once for ERformulation)ExtendedRelease: 5mg oncedailyGlyburide(DiaBeta,Micronase)2.5-5 mgonce dailywithbreakfast orfirst mealMax Dose8 mgSupplied1, 2, 4 mgtab40 mg(maxeffectivedose 20mg)5, 10 mgtabER: 2.5, 5,10 mg tabExtended ExtendedRelease:Release:20 mg/day 2.5 mg, 5mg, 10mg tab20 mg1.25, 2.5,5 mg tabNote: Meglitinides (See below under Specific Situation therapy) may beused in place of Sulfonylureas in patients with a sulfa allergy and/orirregular meals schedules or who have late rise in postprandial glucoselevels on SU’s.b.Dipeptidyl Peptidase- 4 (DPP-4) inhibitors: Alogliptin(Nesina); Linagliptin(Tradjenta); Sitagliptin (Januvia);Saxagliptin(Onglyza)Mechanism
report rapid onset of symptoms. 3. There may or may not be a family history or obvious risk factors. 4. The following should be assessed and documented in chart: a. Current diabetes self-management routine, if previously diagnosed, to include: 1) Duration of diabetes, including age and characteristics of onset, such as diabetic