Transcription
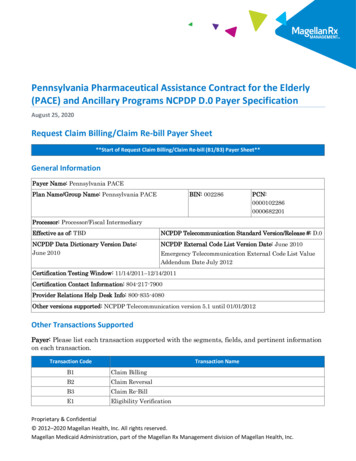
Pennsylvania Pharmaceutical Assistance Contract for the Elderly(PACE) and Ancillary Programs NCPDP D.0 Payer SpecificationAugust 25, 2020Request Claim Billing/Claim Re-bill Payer Sheet**Start of Request Claim Billing/Claim Re-bill (B1/B3) Payer Sheet**General InformationPayer Name: Pennsylvania PACEPlan Name/Group Name: Pennsylvania PACEBIN: 002286PCN:00001022860000682201Processor: Processor/Fiscal IntermediaryEffective as of: TBDNCPDP Telecommunication Standard Version/Release #: D.0NCPDP Data Dictionary Version Date:June 2010NCPDP External Code List Version Date: June 2010Emergency Telecommunication External Code List ValueAddendum Date July 2012Certification Testing Window: 11/14/2011–12/14/2011Certification Contact Information: 804-217-7900Provider Relations Help Desk Info: 800-835-4080Other versions supported: NCPDP Telecommunication version 5.1 until 01/01/2012Other Transactions SupportedPayer: Please list each transaction supported with the segments, fields, and pertinent informationon each transaction.Transaction CodeTransaction NameB1Claim BillingB2Claim ReversalB3Claim Re-BillE1Eligibility VerificationProprietary & Confidential 2012–2020 Magellan Health, Inc. All rights reserved.Magellan Medicaid Administration, part of the Magellan Rx Management division of Magellan Health, Inc.
Field Legend for ColumnsPayer Usage YMThe Field is mandatory for the Segment in the designatedTransaction.NoREQUIREDRThe Field has been designated with the situation of“Required” for the Segment in the designated Transaction.No“Required when.” The situations designated havequalifications for usage (“Required if x,” “Not required if y”).YesQUALIFIEDREQUIREMENTRWFields that are not used in the Claim Billing/Claim Re-bill transactions and those that do nothave qualified requirements (i.e., not used) for this payer are excluded from the document.Claim Billing/Claim Re-bill TransactionThe following lists the segments and fields in a Claim Billing or Claim Re-bill Transaction for theNCPDP Telecommunication Standard Implementation Guide Version D.Ø.Transaction Header Segment QuestionsThis Segment is always sentXSource of certification IDs required inSoftware Vendor/Certification ID(11Ø-AK) is Payer IssuedXTransaction Header SegmentField #Claim Billing/Claim Re-billIf Situational, Payer SituationCheckClaim Billing/Claim Re-billNCPDP Field NameValuePayerUsage1Ø1-A1 BIN NUMBERØØ2286M1Ø2-A2 VERSION/RELEASENUMBERDØM1Ø3-A3 TRANSACTION CODEB1 BillingMB2 ReversalB3 Re-billE1 Eligibility VerificationPage 2 Pennsylvania PACE D.0 Payer SpecificationPayer Situation
Transaction Header SegmentField #Claim Billing/Claim Re-billNCPDP Field Name1Ø4-A4 PROCESSOR CONTROLNUMBERPayerUsageValueTrOOP Claims:MØØØØ1Ø2286Payer SituationIMPORTANT: USE THECORRECT PCN:TrOOP claims include thefollowing programs:Non-TrOOP Claims:ØØØØ6822Ø1PACE, CRDP, SPBP1, and SPBP2Non-TrOOP claims include:CF, SB, MSUD, PKU, PAP1Ø9-A9 TRANSACTION COUNT1 One OccurrenceM2 Two Occurrences3 Three Occurrences4 Four Occurrences2Ø2-B2 SERVICE PROVIDER IDQUALIFIERØ1 – National ProviderIdentifier (NPI)M2Ø1-B1 SERVICE PROVIDER IDNPIM4Ø1-D1 DATE OF SERVICEFormat CCYYMMDDM11Ø-AK SOFTWAREVENDOR/CERTIFICATIONIDMInsurance Segment QuestionsXInsurance SegmentSegment Identification (111-AM) “Ø4”Field #Claim Billing/Claim Re-billNCPDP Field NameValue3Ø2-C2 CARDHOLDER ID3Ø1-C1 GROUP IDClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentAssigned by Magellan yer SituationMPACE through PAP - 9 characterIDRPACE PACE/PACENETCRDP Chronic Renal DiseaseProgramADAP Special PharmaceuticalBenefits Program SP1cardholdersPennsylvania PACE D.0 Payer Specification Page 3
Insurance SegmentSegment Identification (111-AM) “Ø4”Field #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsagePKUPAPSPBP Special PharmaceuticalBenefits Program SP2cardholdersCF Cystic FibrosisSB Spina BifidaMSUD Maple Syrup UrineDiseasePKU PhenylketonuriaPAP PA Patient AssistanceProgram3Ø6-C6 PATIENT RELATIONSHIPCODEPatient Segment QuestionsPayer SituationR1 CardholderClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXPatient SegmentSegment Identification (111-AM) “Ø1”FieldNCPDP Field NameClaim Billing/Claim Re-billValue3Ø4-C4 DATE OF BIRTH3Ø5-C5 PATIENT GENDER CODERequired for B1 and B3 transactions.PayerUsagePayer SituationRØ Not Specified1 Male2 Female31Ø-CA PATIENT FIRST NAMERRImp Guide: Required when thepatient has a first name.Payer Requirement: Required forpatient name validation.311-CB PATIENT LAST NAMERImp Guide: Required when thepatient has a last name.Payer Requirement: Required forpatient name validation.384-4X PATIENT RESIDENCEPage 4 Ø Not Specified1 Home2 Skilled NursingFacility. PART BONLYPennsylvania PACE D.0 Payer SpecificationRImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.
Patient SegmentSegment Identification (111-AM) “Ø1”FieldNCPDP Field NameClaim Billing/Claim Re-billPayerValueUsagePayer Requirement: Same as ImpGuide.3 Nursing Facility4 Assisted LivingFacility5 Custodial CareFacility. PART BONLYPatient Residence 3 NursingFacility required whenrecipient is identified as along-term care resident.Ø “Not Specified” will deny.6 Group Home7 Inpatient PsychiatricFacility8 Psychiatric Facility –PartialHospitalization9 Intermediate CareFacility/MentallyRetarded1Ø ResidentialSubstance AbuseTreatment Facility11 Hospice12 PsychiatricResidential TreatmentFacility13 ComprehensiveInpatientRehabilitation Facility14 Homeless ShelterClaim Segment QuestionsXThis payer supports partial fillsXClaim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field Name455-EM PRESCRIPTION/SERVICEREFERENCE NUMBERQUALIFIERClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentPayer SituationClaim Billing/Claim Re-billValue1 Rx BillingPayerUsageMPayer SituationPayer Requirement: ForTransaction Code of “B1,” in theClaim Segment, thePrescription/Service ReferencePennsylvania PACE D.0 Payer Specification Page 5
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationNumber Qualifier (455-EM) is “1”(Rx Billing).4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBERM436-E1 PRODUCT/SERVICE IDQUALIFIERØ3 National Drug Code(NDC)M4Ø7-D7 PRODUCT/SERVICE IDNDC for non-compoundclaims“Ø” for compound claimsMØØ Not Specified456-EN ASSOCIATEDPRESCRIPTION/SERVICEREFERENCE NUMBERRWPayer Requirement: Use “ØØ” forcompounds.Required if the “completion”transaction in a partial fill(Dispensing Status [343-HD] “C” [Completed]).Required if the Dispensing Status(343-HD) “P” (Partial Fill) andthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide.457-EP ASSOCIATEDPRESCRIPTION/SERVICEDATERWImp Guide: Required if the“completion” transaction in apartial fill (Dispensing Status[343-HD] “C” [Completed]).Required if AssociatedPrescription/Service ReferenceNumber (456-EN) is used.Required if the Dispensing Status(343-HD) “P” (Partial Fill) andthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide.442-E7 QUANTITY DISPENSEDMetric Decimal Quantity460-ET QUANTITY PRESCRIBEDPage 6 Pennsylvania PACE D.0 Payer SpecificationRRWImp Guide: Required when atransmission is for a Scheduled IIdrug as defined in 21 CFR1308.12 and per CMS-0055-F(Compliance Date 9/21/2020.
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationRefer to the Version D.0 EditorialDocument).4Ø3-D3 FILL NUMBERØ Original dispensingRefill number – Numberof the replenishment4Ø5-D5 DAYS SUPPLYRR4Ø6-D6 COMPOUND CODE1 Not a Compound2 CompoundR4Ø8-D8 DISPENSE AS WRITTEN(DAW)/PRODUCTSELECTION CODEØ No Product SelectionIndicated1 Substitution NotAllowed by Prescriber2 Substitution AllowedPatient RequestedProduct Dispensed3 Substitution AllowedPharmacist SelectedProduct Dispensed4 Substitution AllowedGeneric Drug Not inStock5 Substitution AllowedBrand DrugDispensed as aGeneric6 Override7 Substitution NotAllowed-Brand DrugMandated by Law8 Substitution AllowedGeneric Drug NotAvailable inMarketplace9 Substitution AllowedBy Prescriber butPlan Requests Brand– Patient's PlanRequested BrandProduct To BeDispensedRPACE Maximum of 30 whenprimary. Other program’s daysupply may differ.PACE, CRDPDAW 1 subject to M.E. process forPACE.DAW 5 used only when submittedU&C is equal to or less thangeneric. DAW 5 not acceptedin lieu of a Medical Exceptionfor an A Rated brand productwhen PACE is primary payer.Pennsylvania PACE D.0 Payer Specification Page 7
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValue414-DE DATE PRESCRIPTIONWRITTEN415-DF NUMBER OF REFILLSAUTHORIZEDPayerUsagePayer SituationRØ No refills authorized1-99 Authorized Refillnumber – with 99being as needed,refills unlimitedRImp Guide: Required if necessaryfor plan benefit administration.Payer Requirement: Same as ImpGuide. PACE, CRDP, SPBP, andall other PennsylvaniaDepartment of Agingadministered plans use aninternal counter that limits refillsto maximum of 5 althoughprescriber may authorize more.Note: Value of “99” is notacceptable for any PDAadministered programs.419-DJ PRESCRIPTION ORIGINCODE354-NX SUBMISSIONCLARIFICATION CODECOUNT42ØDKPage 8SUBMISSIONCLARIFICATION CODE Ø Not Known1 Written2 Telephone3 Electronic4 Facsimile5 PharmacyMaximum count of 3.RImp Guide: Required if necessaryfor plan benefit administration.Payer Requirement: Value of “Ø”will deny as Invalid. All othercodes are accepted.RW*** Imp Guide: Required ifSubmission Clarification Code(42Ø-DK) is used.Payer Requirement: Required ifSubmission Clarification Code(42Ø-DK) is used.1 No Override2 Other Override3 Vacation Supply4 Lost Prescription5 Therapy Change6 Starter Dose7 Medically Necessary8 Process CompoundFor ApprovedIngredients9 Encounters1Ø Meets PlanLimitations11 Certification on FilePennsylvania PACE D.0 Payer SpecificationRWImp Guide: Required ifclarification is needed and valuesubmitted is greater than zero(Ø).Payer Requirement: Requiredwhen needed to provideadditional information forcoverage purposes.NOTE: SPBP1 providers: SeeSPBP1 Provider AgreementSection I.N.Value #8 may be used for multiingredient compounds.
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValue12 DME ReplacementIndicator13 Payer-RecognizedEmergency/DisasterAssistance Request14 Long-Term CareLeave of Absence15 Long-Term CareReplacementMedication16 Long-Term CareEmergency box (kit)or automateddispensing machine17 Long-Term CareEmergency supplyremainder18 Long-Term CarePatientAdmit/ReadmitIndicator2Ø 34ØB21 LTC dispensing: 14days or less notapplicable – Fourteenday or less dispensingis not applicable dueto CMS exclusionand/or manufacturerpackaging may not bebroken or specialdispensingmethodology (i.e.,vacation supply, leaveof absence, ebox,spitter dose).Medication quantitiesare dispensed as billed22 LTC dispensing: 7days – Pharmacydispenses medicationin 7 day suppliesPayerUsagePayer SituationValue #3 accepted only forSpecial Pharmaceutical BenefitsProgram cardholders.Value #20 MUST be enteredwhen submitting a drugpurchased under Section 340B ofthe Public Health Service Act.Other values accepted, but editedONLY for data integrity, i.e. noillegal characters, etc.Pennsylvania PACE D.0 Payer Specification Page 9
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValue23 LTC dispensing: 4days – Pharmacydispenses medicationin 4 day supplies24 LTC dispensing: 3days – Pharmacydispenses medicationin 3 day supplies25 LTC dispensing: 2days – Pharmacydispenses medicationin 2 day supplies26 LTC dispensing: 1day – Pharmacy orremote (multipleshifts) dispensesmedication in 1 daysupplies27 LTC dispensing: 4-3days – Pharmacydispenses medicationin 4 day, then 3 daysupplies28 LTC dispensing: 2-3days – Pharmacydispenses medicationin 2 day, then 2 day,then 3 day supplies29 LTC dispensing: dailyand 3-day weekend –Pharmacy or remotedispensed dailyduring the week andcombines multipledays dispensing forweekends30 LTC dispensing: Pershift dispensing –Remote dispensingper shift (multiplemed passes)31 LTC dispensing: Permed pass dispensing –Page 10 Pennsylvania PACE D.0 Payer SpecificationPayerUsagePayer Situation
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer SituationRemote dispensingper med pass32 LTC dispensing:PRN on demand –Remote dispensing ondemand as needed33 LTC dispensing: 7day or less cycle nototherwise represented34 LTC dispensing: 14days dispensing –Pharmacy dispensesmedication in 14 daysupplies35 LTC dispensing: 8–14 day dispensingmethod not listedabove – 8–14-Daydispensing cycle nototherwise represented36 LTC dispensing:dispensed outsideshort cycle – Claimwas originallysubmitted to a payerother than MedicarePart D and wassubsequentlydetermined to be PartD.3Ø8-C8 OTHER COVERAGE CODE Ø Not Specified bypatient1 No other coverage2 Other coverage existspayment collected3 Other Coverage Billed– claim not covered4 Other coverage existspayment not collected429-DT SPECIAL PACKAGINGINDICATORRWImp Guide: Required if needed byreceiver, to communicate asummation of other coverageinformation that has beencollected from other payers.Required for Coordination ofBenefits.Payer Requirement: Same as ImpGuide.Ø Not Specified1 Not Unit Dose –Indicates the productPennsylvania PACE D.0 Payer Specification Page 11
Claim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValue23456Page 12 is not being dispensedin special unit dosepackaging. Manufacturer UnitDose – A code used toindicate a distinctdose as determined bythe manufacturer. Pharmacy Unit Dose –Used to indicate whenthe pharmacy hasdispensed the drug ina unit of use packagewhich was “loaded” atthe pharmacy – notpurchased from themanufacturer as aunit dose. Pharmacy Unit DosePatient CompliancePackaging – Unit doseblister, strip or otherpackaging designed incompliance-promptingformats that helppeople take theirmedications properly. Pharmacy Multi-drugPatient CompliancePackaging –Packaging that maycontain drugs frommultiplemanufacturerscombined to ensurecompliance and safeadministration Remote Device UnitDose– Drug isdispensed at thefacility, via a remotedevice, in a unit of usepackagePennsylvania PACE D.0 Payer SpecificationPayerUsagePayer Situation
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer Situation7 Remote Device Multi‐drug Compliance –Drug is dispensed atthe facility, via aremote device, withpackaging that maycontain drugs frommultiplemanufacturerscombined to ensurecompliance and safeadministration8 Manufacturer Unit ofUse Package (not unitdose) – Drug isdispensed bypharmacy in originalmanufacturer’spackage and relabeledfor use. Applicable inlong term care claimsonly (as defined in theTelecommunicationEditorial Document).6ØØ-28 UNIT OF MEASUREEA EachGM GramsML MillilitersRWImp Guide: Required if necessaryfor state/federal/regulatoryagency programs.Required if this field could resultin different coverage, pricing, orpatient financial responsibility.Payer Requirement: Same as ImpGuide. Required for all claimsubmissions.418-DI LEVEL OF SERVICEØ Not Specified1 Patient consultation2 Home delivery3 Emergency4 24-hour service5 Patient consultationregarding genericproduct selection6 In-Home ServiceRWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement:Note: Not used by PACE, CRDP,SPBP, or any of the PennsylvaniaDepartment of Agingadministered plans.Pennsylvania PACE D.0 Payer Specification Page 13
Claim SegmentSegment Identification (111-AM) “Ø7”Field #NCPDP Field Name343-HD DISPENSING STATUSClaim Billing/Claim Re-billValueP Partial FillC Completion of PartialFillPayerUsageRWPayer SituationImp Guide: Required for thepartial fill or the completion fill ofa prescription.Payer Requirement: Same as ImpGuide.344-HF QUANTITY INTENDED TOBE DISPENSEDRWImp Guide: Required for thepartial fill or the completion fill ofa prescription.Payer Requirement: Same as ImpGuide.345-HG DAYS SUPPLY INTENDEDTO BE DISPENSEDRWImp Guide: Required for thepartial fill or the completion fill ofa prescription.Payer Requirement: Same as ImpGuide.147-U7 PHARMACY SERVICETYPEPharmacy Provider Segment Questions1 Community/RetailPharmacy Services2 CompoundingPharmacy Services3 Home InfusionTherapy ProviderServices4 InstitutionalPharmacy Services5 Long-Term CarePharmacy Services6 Mail Order PharmacyServices7 Managed CareOrganizationPharmacy Services8 Specialty CarePharmacy Services99 OtherCheckThis Segment is always sentPage 14 Pennsylvania PACE D.0 Payer SpecificationRWImp Guide: Required when thesubmitter must clarify the type ofservices being performed as acondition for properreimbursement by the payer.Payer Requirement: Same as ImpGuide.Claim Billing/Claim Re-billIf Situational, Payer Situation
Pharmacy Provider Segment QuestionsThis Segment is situationalClaim Billing/Claim Re-billIf Situational, Payer SituationCheckXIt is used when a receiver needspharmacy provider information toperform claim/encounter determination.Claims will not be denied if this segmentis not sent.Pharmacy Provider SegmentSegment Identification (111-AM) “Ø2”Field #NCPDP Field NameClaim Billing/Claim Re-billValue465-EY PROVIDER ID QUALIFIER Ø2 State LicenseØ4 NameØ5 NPIPayerUsagePayer SituationRWImp Guide: Required if ProviderID (444-E9) is used.Payer Requirement: Same asImp Guide.04 (Name) applies only to DME.444-E9 PROVIDER IDRWImp Guide: Required if necessaryfor state/federal/regulatoryagency programs.Payer Requirement: Ø2Pharmacist License Number; Ø5Pharmacist NPI or Ø4 DMEname.Pricing Segment QuestionsThis Segment is always sentXPricing SegmentSegment Identification (111-AM) “11”Field #NCPDP Field Name4Ø9-D9 INGREDIENT COSTSUBMITTED412-DC DISPENSING FEESUBMITTEDClaim Billing/Claim Re-billIf Situational, Payer SituationCheckClaim Billing/Claim Re-billValuePayerUsageRPayer SituationNOTE: SPBP1 providers:See SPBP1 Provider AgreementSection I.N.RWImp Guide: Required if its valuehas an effect on the GrossAmount Due (43Ø-DU)calculation.Payer Requirement: Same asImp Guide.Pennsylvania PACE D.0 Payer Specification Page 15
Pricing SegmentSegment Identification (111-AM) “11”Field #Claim Billing/Claim Re-billNCPDP Field NameValue478-H7 OTHER AMOUNTCLAIMED SUBMITTEDCOUNTMaximum count of 3.479-H8 OTHER AMOUNTCLAIMED SUBMITTEDQUALIFIERØ1Ø2Ø3Ø4Ø9PayerUsagePayer SituationRW*** Imp Guide: Required if OtherAmount Claimed SubmittedQualifier (479-H8) is used.Payer Requirement: Same asImp Guide. Delivery CostRW*** Imp Guide: Required if Other Shipping CostAmount Claimed Submitted Postage Cost(48Ø-H9) is used. Administrative CostPayer Requirement: Same as CompoundImp Guide. All values will bePreparation Costaccepted.Submitted99 OtherRW*** Imp Guide: Required if its valuehas an effect on the GrossAmount Due (43Ø-DU)calculation.48Ø-H9 OTHER AMOUNTCLAIMED SUBMITTEDPayer Requirement: Same asImp Guide.426-DQ USUAL AND CUSTOMARYCHARGERImp Guide: Required if neededper trading partner agreement.Payer Requirement: Same asImp Guide.43ØDUGROSS AMOUNT DUE423-DN BASIS OF COSTDETERMINATIONRØØ DefaultØ1
Provider Relations Help Desk Info: 800-835-4080 Other versions supported: NCPDP Telecommunication version 5.1 until 01/01/2012 . Other Transactions Supported . Payer: Please list each transaction supported with the segments, fields, and pertinent information on each transaction. Transaction C