Transcription
NEW MEXICOUBA dentalUBA Dental PlanMember Driven Value.Certificate of InsuranceBroad Coverage For Brighter Smiles.Download Claim Forms:ubamembers.com/claimforms.htmlDENTAL INSURANCEThis certificate of insurance is for the UBA Dental Plan purchasedon or after 040518. You can call your personal memberconcierge at 866.438.4274 for any questions with your certificate.UBAUBA Dental CertificateofInsurance v0419United Business Association409 W Vickery Blvd, Fort Worth, TX 76104 866.438.4274 ubamembers.com
Member Driven Value.Group Dental Insurance Certificate of InsuranceRenaissanceFamily.com/FindADentistIf you decide to contact a dental office directly,please refer to the following network partners that adental office will likely recognize:Maximum Care Maverest Connection DentalASSOCIATION BENEFITSPROVIDED BY:UBAINSURANCE COVERAGEUNDERWRITTEN BY:BILLING, FULFILLMENT,& CUSTOMER SERVICEPROVIDED BY:Healthyamerica
Renaissance PPONew Mexico GroupDental CertificateUnited BusinessAssociationThis type of plan is NOT considered “minimum essential coverage” under the Affordable Care Act andtherefore does NOT satisfy the individual mandate that you have health insurance coverage. If you do not haveother health insurance coverage, you may be subject to a tax penalty. Please consult your tax advisor.P.O. Box 1596 Indianapolis, IN 46206-1596 www.renaissancefamily.com
RENAISSANCE PPONEW MEXICO GROUP DENTAL CERTIFICATETable of ContentsSummary of Dental Plan Benefits.1I.Renaissance PPO Group Dental Certificate .3II.Definitions.3III.General Eligibility Rules.6IV.Benefits .7V.Exclusions and Limitations .11VI.Accessing Your Benefits.12VII.Questions and Answers .13VIII.Coordination of Benefits .14IX.Disputed Claims Procedure.17X.Termination of Coverage .18XI.Continuation of Coverage .18XII.General Conditions .19Important Cancellation Information – Please Read Section X Entitled “Termination of Coverage”.NOTE: This PPO Group Dental Certificate should be read in conjunction with the Summary of DentalPlan Benefits that is provided with the Certificate. The Summary of Dental Plan Benefits lists thespecific provisions of your group dental plan. Your group dental plan is a legal contract between thePolicyholder and Renaissance Life & Health Insurance Company of America (“RLHICA”).READ YOUR PPO GROUP DENTAL CERTIFICATE CAREFULLY.D-200A-2017-NMAGii
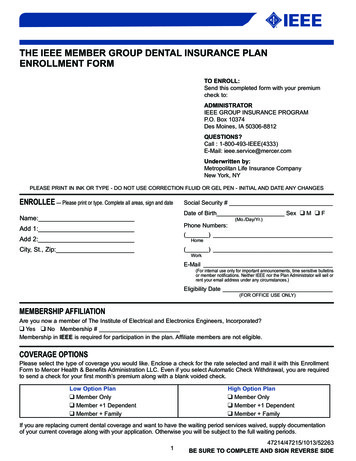
Renaissance Life & Health Insurance Company of AmericaRenaissance Group Dental Preferred Provider CertificateSummary of Dental Plan BenefitsFor Group#3621United Business AssociationThis Summary of Dental Plan Benefits is part of, and should be read in conjunction with your Group Dental Certificate. YourGroup Dental Certificate will provide you with additional information about your RENAISSANCE LIFE & HEALTHINSURANCE COMPANY OF AMERICA (“RLHICA”) coverage, including information about exclusions and limitations.Benefit Year –January 1 through December 31In-NetworkOut-of-NetworkYouPayYouPayNo chargeNo chargeNo chargeNo charge30%30%No chargeNo charge30%30%30%30%No chargeNo chargePeriodontal Maintenance – Periodontal maintenance following active periodontal therapy30%30%Other Basic Services –miscellaneous services including, but not limited to cephalometric films,tests and examinations, anesthesia and professional consultations and/or visits30%30%50%50%50%50%50%50%Major Restorative Services – Used when teeth can't be restored with another filling material (forexample, crowns)Prosthodontic Services – Used to replace missing natural teeth (for example, bridges, endostealimplants, partial dentures, and complete dentures)Relines and Repairs – Relines and repairs to fixed bridges, partial dentures, and complete dentures50%50%50%50%50%50%Other Major Services – Occlusal guards, and limited occlusal adjustments50%50%100%100%Covered ServicesDiagnostic And Preventive ServicesDiagnostic and Preventive Services - Used to evaluate existing conditions and/or to prevent dentalabnormalities or disease (includes exams, cleanings, bitewing X-rays and fluoride treatments)Brush Biopsy – Used to detect oral cancerBasic ServicesEmergency Palliative Treatment - Used to temporarily relieve painRadiographs/Diagnostic Imaging/Diagnostic Casts - X-rays as required for routine care or asnecessary for the diagnosis of a specific conditionMinor Restorative Services – Used to repair teeth damaged by disease or injury (for example,silver fillings and white fillings)Simple Extractions – Simple extractions including local anesthesia, suturing, if needed and routinepost-operative careSealants – Sealants for the occlusal surface of first and second permanent molarsMajor ServicesOral Surgery Services – Extractions and dental surgery and services for the diagnosis andtreatment of temporomandibular disorders including craniomandibular and temporomandibularjoint disorders (coverage for craniomandibular and temporomandibular joint disorders include bothsurgical and non-surgical procedures)Endodontic Services – Used to treat teeth with diseased or damaged nerves (for example, rootcanals)Periodontic Services – Used to treat diseases of the gums and supporting structures of the teethOrthodontic ServicesOrthodontic Services – Services , treatment, and procedures to correct malposed teeth (forexample, braces) {including Orthodontic Services for Children to the age of 19} includingOrthodontic Services for adultsD-200A-2017-NMAG1
Method of Payment – For services rendered or items provided by an In-Network Dentist, the Allowed Amount is a prenegotiated fee that the provider has agreed to accept as payment in full. For services rendered or items provided by an Outof-Network Dentist, RLHICA determines the Allowed Amount using statistically valid claims data submitted to RLHICA andits affiliates which show the most frequently charged fees by providers in the same geographic areas for comparable services orsupplies. The claims data and fees are updated periodically using the most current codes and nomenclature developed andmaintained by the American Dental Association. RLHICA will base Benefits on the lesser of the Submitted Amount and theAllowed Amount. If the Submitted Amount for an Out-of-Network Dentist is more than the Allowed Amount, you arenot only responsible for paying the Dentist that percentage listed in the “You Pay” column, but are also responsible forpaying the Dentist the difference between the Submitted Amount and the Allowed Amount.Maximum Payment – 1,000 per person per Benefit Year on Diagnostic and Preventive, Basic, and Major Servicescollectively.Maximum Carryover – If at least one Covered Service is paid in a Benefit Year and the total Benefit paid does notexceed 500 in that Benefit Year, 250 will carry over to the next Benefit Year’s Maximum Payment. This amount willaccumulate from one Benefit Year to the next, but will not exceed 1,000.Deductible – 50 Deductible per person per Benefit Year limited to a maximum Deductible of 150 per family perBenefit Year. The Deductible does not apply to Diagnostic and Preventive, including Sealants and Radiographs.Waiting Period - You (and your Eligible Dependents, if covered) will be eligible for coverage on the next availableeffective date.You (and your Eligible Dependents, if covered) will be eligible for coverage for Major Services 12 months following thedate you or your Eligible Dependent is enrolled. (Eligible Dependents enrolled after your date of enrollment will havetheir own waiting period.)Eligibility (Certificate Holder and Eligible Dependents) – All dues paying members in good standing are eligible toelect coverage hereunder.Also eligible are your Legal Spouse and any individuals who meet the definition of Child(ren) as set forth in your GroupDental Certificate.Where two individuals are eligible under the same group policy and are legally married to each other, they will beenrolled under one application and will receive Benefits under a single Certificate without coordination of benefits underthe Policy.You pay the full cost of this coverage.D-200A-2017-NMAG2
PLEASE NOTE: RLHICA recommends a PreTreatment Estimate before any services arerendered where the total charges will exceed 200.You and your Dentist should review your PreTreatment Estimate before your Dentist proceedswith treatment.II. DefinitionsAdverse Benefit DeterminationMeans any denial, reduction, or termination of the Benefitsfor which you filed a claim. Or a failure to provide or tomake payment (in whole or in part) of the Benefits yousought, including any such determination based oneligibility, application of any utilization review criteria, or adetermination that the item or service for which Benefitsare otherwise provided was experimental or investigational,or was not medically necessary or appropriate.I. Renaissance PPO GroupDental CertificateRLHICA issues this Renaissance Dental PPOCertificate to you, the Certificate Holder. TheCertificate is a summary of your dental benefitscoverage. It reflects and is subject to the agreementbetween RLHICA and your organization (the“Policyholder”).Allowed AmountMeans the maximum dollar amount upon which RLHICAwill base Benefit. For services rendered by In-NetworkDentist, the Allowed Amount are pre-negotiated fees thatthe provider has agreed to accept as payment in full. Forservices rendered by Out-of-Network Dentist, RLHICAdetermines the Allowed Amount based upon treatmentrendered and a periodically determined percentile of feescharged by a sample of Dentist of similar training withinyour geographic area.The Benefits provided under This Plan may change ifany state or federal laws change.RLHICA agrees to provide Benefits as described inthis Certificate.All the provisions in the following pages, read inconjunction with the Summary of Dental Plan Benefitsand all attachments and addendums, form a part of thisdocument as fully as if they were stated over thesignature below.Benefit YearMeans the calendar year, unless your organization elects adifferent Benefit Year. The Benefit Year is specified in theSummary of Dental Plan Benefits.IN WITNESS WHEREOF, this Certificate is executedby an authorized officer of RLHICA.BenefitsMeans payment for Covered Services.CertificateMeans this document. RLHICA will provide dentalBenefits as described in this Certificate. Any changes inthis Certificate will be based on changes to the Policy.Changes to the Certificate will be in the Summary ofDental Plan Benefits Section.Robert P. MulliganPresident and CEOHome Office:RENAISSANCE LIFE & HEALTHINSURANCE COMPANY OF AMERICAAttn: Renaissance AdministrationCertificate HolderMeans you, when your organization certifies to RLHICAthat you are eligible to receive Benefits under This Plan.P.O. Box 1596Indianapolis, IN 46206-1596Administrative Direct Line: 1-800-745-7509Customer Service Direct Line: 1-888-358-9484(TTY users call 711)D-200A-2017-NMAG3
application of the child’s other parent, the stateagency administering the Medicaid program or thestate agency administering 42 U.S.C. Sections 651through 669, the child support enforcement program.Child(ren)Means your natural children, stepchildren, adoptedchildren, or foster children placed in the foster home,children by virtue of legal guardianship or who areresiding with you during the waiting period for legaladoption or guardianship. Your Child(ren) who has not yet reached the endof the calendar year of his or her 26th birthday;or, Your Child(ren) for whom you or your legalspouse are financially responsible for medical,health, or dental care under terms of a courtdecree; or, The child will not be disenrolled or coverage eliminatedunless RLHICA is provided satisfactory writtenevidence that (a) the court or administrative order is nolonger in effect; or (b) the child is or will be enrolled incomparable health coverage through another insurer thatwill take effect no later than the effective date ofdisenrollment.CoinsuranceMeans the percentage of the Allowed Amount for CoveredServices that the Certificate Holder must pay towardtreatment.Your children who has reached the end of thecalendar year of his or her 26th birthday and isboth (1) incapable of self-sustainingemployment by reason of a mental or physicalcondition and (2) chiefly dependent upon theCertificate Holder for support and maintenance.In the event that RLHICA denies a claim underthis Plan for the reason that the child hasattained the Limiting Age for dependentchildren, you will have the burden ofestablishing that the child continues to meet thetwo criteria specified above. If requested byRLHICA, you submit medical reportsconfirming that the child meets the two criteriaspecified above.Completion DatesMeans the date that treatment is complete. Treatment iscomplete:Coverage for Child(ren) of Non-custodialParents. When a child has health coveragethrough an Certificate Holder who is a noncustodial parent, RLHICA shall (1) provide suchinformation to the custodial parent as may benecessary for the child to obtain benefits; (2)permit the custodial parent or the provider, withthe custodial parent’s approval, to submit claimsfor covered services without the approval of thenon-custodial parent; and (3) make payments onclaims submitted to the custodial parent, theprovider or the state Medicaid agency.for dentures and partial dentures, on the deliverydate; for crowns and bridgework, on the permanentcementation date; for root canals and periodontal treatment, on thedate of the final procedure that completes thetreatment.CopaymentMeans the dollar amount that the Certificate Holder mustpay toward treatment.Covered ServicesMeans the unique dental service(s) selected for coverage asdescribed in the Declarations Section and subject to theterms and conditions of this Policy.When an insured parent is required by a court oradministrative order to provide health coveragefor a child, such Insured shall be permitted toenroll a child who is otherwise eligible forcoverage without regard to any enrollmentperiod restrictions.DeductibleMeans the amount an individual and/or a family must paytoward Covered Services before RLHICA begins payingfor those services under this Policy. If the Policyholder hasselected a Deductible, it will be indicated in theDeclarations Section.If the parent is enrolled but fails to makeapplication to obtain coverage for the child, theparent shall be permitted to enroll the child uponD-200A-2017-NMAG 4
DentistOut-of-Network DentistMeans a person licensed to practice dentistry in thestate or jurisdiction in which dental services arerendered.Means a Dentist who has not entered into a contract and isnot otherwise engaged by us to provide Covered Servicesfor pre-negotiated fees.Eligible DependentsPolicy YearMeans (a) the Certificate Holder’s Legal Spouse; (b)the Certificate Holder’s Child(ren); and (c) any otherdependents who meet the criteria for eligibility set forthin the Declarations Section. If dependent coverage hasbeen selected, it will be indicated in the DeclarationsSection.Means the 12-month period beginning on the EffectiveDate of the Policy and each 12-month renewal periodthereafter.Pre-Treatment EstimateMeans a voluntary and optional process where we issuea written estimate of dental benefits that may beavailable under your coverage for the proposed dentaltreatment to us in advance of providing the treatment toyou.In-Network DentistMeans a Dentist who has entered into a contract or isotherwise engaged by us to provide Coveredservices for pre-negotiated fees that the Dentist hasagreed to accept as payment in full. A current list ofIn-Network Dentists is available atwww.RenaissanceDental.com.A Pre-Treatment Estimate is for informational purposesonly and is not required before you receive dental care.It is not a prerequisite or condition for approval of futuredental benefits payment. You will receive the sameBenefits under this Policy whether or not a PreTreatment Estimate is requested. The benefits estimateprovided on a Pre-Treatment Estimate is based on thebenefits available on the date the notice is issued. It isnot a guarantee of future dental benefits or payment.Legal SpouseMeans a person who is any of the following: (a) thespouse of the Certificate Holder through a marriagelegally recognized by the state in which this Policy wasissued; or (b) the partner of the Certificate Holderthrough a civil union legally recognized by the state inwhich this Policy was issued.Availability of dental benefits at the time your treatmentis completed depends on factors. These factors include,but are not limited to, your continued eligibility forBenefits, your available annual or lifetime MaximumPayments, any coordination of benefits, the status ofyour Dentist, this Policy’s limitations and any otherprovisions, together with any additional information orchanges to your treatment. A request for a PreTreatment Estimate is not a claim for Benefits or apreauthorization, precertification or other reservation offuture Benefits.Limiting AgeMeans the age at which a Child of the CertificateHolder is no longer eligible for Benefits under thisPolicy pursuant to the definition of Child above.Maximum PaymentMeans the maximum dollar amount RLHICA will payin any Benefit Year or lifetime for Covered Services.The Maximum Payments are specified in theDeclarations Section.RLHICAMeans Renaissance Life & Health Insurance Company ofAmerica.Open Enrollment PeriodSubmitted AmountMeans the period of time as determined by thePolicyholder, during which an eligible person asindicated in the Declarations Section may enroll or beenrolled to receive Benefits.D-200A-2017-NMAGThe fee a Dentist bills to RLHICA for a specific service oritem.5
court or administrative order to otherwiseprovide Benefits for a Child or EligibleDependent.Summary of Dental Plan BenefitsMeans a list of specific provisions of This Plan and is apart of this Certificate.Once eligible, you and your Eligible Dependentsmust enroll for coverage within 30 days from thedate upon which you or your Eligible Dependentsbecome eligible for Benefits under the terms ofSection III B immediately above. You and yourEligible Dependents may properly enroll forcoverage by completing all enrollment formsrequired by RLHICA and submitting such forms toyour organization. If you and your EligibleDependents are not properly enrolled for coveragewithin 30 days from the date upon which you andyour Eligible Dependents become eligible forBenefits, then you and/or your EligibleDependents must wait until the next OpenEnrollment Period to enroll.This PlanMeans the dental coverage as provided for you andyour Eligible Dependents pursuant to this Certificate.III. General Eli
UBA Dental Plan Certificate of Insurance . Maverest Connection Dental. Renaissance PPO New Mexico Group Dental Certificate United Business . its affiliates which show the most frequently charged fees by providers in the same geographic areas for comparable services or