Transcription
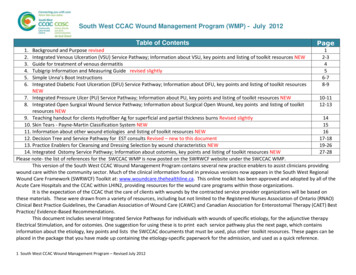
South West CCAC Wound Management Program (WMP) - July 2012Table of Contents1.2.3.4.5.6.PageBackground and Purpose revised1Integrated Venous Ulceration (VSU) Service Pathway; Information about VSU, key points and listing of toolkit resources NEW2-3Guide for treatment of venous dermatitis4Tubigrip Information and Measuring Guide revised slightly5Simple Unna’s Boot Instructions6-7Integrated Diabetic Foot Ulceration (DFU) Service Pathway; Information about DFU, key points and listing of toolkit resources8-9NEW7. Integrated Pressure Ulcer (PU) Service Pathway; Information about PU, key points and listing of toolkit resources NEW10-118. Integrated Open Surgical Wound Service Pathway; Information about Surgical Open Wound, key points and listing of toolkit12-13resources NEW9. Teaching handout for clients Hydrofiber Ag for superficial and partial thickness burns Revised slightly1410. Skin Tears - Payne-Martin Classification System NEW1511. Information about other wound etiologies and listing of toolkit resources NEW1612. Decision Tree and Service Pathway for EST consults Revised – new to this document17-1813. Practice Enablers for Cleansing and Dressing Selection by wound characteristics NEW19-2614. Integrated Ostomy Service Pathway; Information about ostomies, key points and listing of toolkit resources NEW27-28Please note- the list of references for the SWCCAC WMP is now posted on the SWRWCF website under the SWCCAC WMP.This version of the South West CCAC Wound Management Program contains several new practice enablers to assist clinicians providingwound care within the community sector. Much of the clinical information found in previous versions now appears in the South West RegionalWound Care Framework (SWRWCF) Toolkit at: www.woundcare.thehealthline.ca. This online toolkit has been approved and adopted by all of theAcute Care Hospitals and the CCAC within LHIN2, providing resources for the wound care programs within those organizations.It is the expectation of the CCAC that the care of clients with wounds by the contracted service provider organizations will be based onthese materials. These were drawn from a variety of resources, including but not limited to the Registered Nurses Association of Ontario (RNAO)Clinical Best Practice Guidelines, the Canadian Association of Wound Care (CAWC) and Canadian Association for Enterostomal Therapy (CAET) BestPractice/ Evidence-Based Recommendations.This document includes several Integrated Service Pathways for individuals with wounds of specific etiology, for the adjunctive therapyElectrical Stimulation, and for ostomies. One suggestion for using these is to print each service pathway plus the next page, which containsinformation about the etiology, key points and lists the SWCCAC documents that must be used, plus other toolkit resources. These pages can beplaced in the package that you have made up containing the etiology-specific paperwork for the admission, and used as a quick reference.MP:Venous Ulcerations Algorithm April 20111 South West CCAC Wound Management Program – Revised July 2012
Case ManagerETN/WCSACTIONSNURSINGACTIONS2 South West CCAC Wound Management Program – Revised July 2012Marv
Information about Venous Leg Ulcerations (VLU)Venous Leg Ulcerations Shallow, moist ulcers , irregular in shape with slopingedges Located on gaiter area of leg usually above or near medialmalleolus Yellow slough or fibrin with buds of granulation; rarelyhave escharCellulitis With Venous Disease Cellulitis infection presents as a diffuse, bright red, hotleg with tenderness and often fever. Clear serous exudate pour out of the small openings incopious amounts Large blisters (bullae) can form Often cannot tolerate their compression due to painDermatitis With Venous Disease Stasis dermatitis causes a red, itchy, &/or dry and scalyrash, can weep and form crusts. Skin appears brown or purple color Acute contact dermatitis causes itching, burning redareas on the leg corresponding to use of topical producte.g. creams or dressings lanolin, antibiotic creams andungs, perfumed, Vitamin A or E etc. or from dressingexudate being trapped on the skinMixed Venous/Arterial Disease Mixed symptoms of both venous and arterial disease butpain is more arterial, cannot use high compression ABI between 0.5 and 0.8 should be healable dependingon other co-morbidities, and using safe, low compressionImportant TipsAvoid use of adhesive products and known sensitizers due toincreased sensitivity of people with venous disease3 South West CCAC Wound Management Program Revised July 2012ItemSWCCACDocumentsthat must beusedTreat theCauseSWRWCFToolkitSection F.6VenousUlcers Treat the Cause and Resources“My Venous Ulcer” - teaching booklet to review with clients“My Wound Care-Venous & Compression ”- self-care guideSWCCAC Venous Wound Care Plan with time-specific goalsCompression therapy is the cornerstone of VLU treatmentNB* must be prescribed by a physician and should only beinitiated after a lower leg assessment including Ankle BrachialPressure Index measurement has been performed.Compression bandaging is an added skill for clinicians and theremust be an educational component and mentoring to ensuresafety and efficacy in application.“Compression for Life” is the best method to decrease risk ofrecurrences.www.woundcare.thehealthline.caB.2.1 Purpose and Instructions for Use for Lower LegAssessment – includes photos and definitions of signs andsymptoms of venous and arterial diseaseB.2.2 Lower Leg Assessment FormF.6Venous Ulcer And Mixed Venous Arterial UlcersF.6.1 Background and Extent of EtiologyF.6.2 Clinical Algorithm based on wound bed preparationF.6.3 Self-Care Teaching ToolF.6.4 My Venous Ulcer client teaching bookletF.6.5Evidence-Based Clinical Interventions (FromSWCCAC WMP 2011)F.6.5.1 Venous Stasis Ulceration Clinical InterventionsF.6.5.2 Venous Disease With Cellulitis Clinical InterventionsF.6.5.2 Venous Stasis Dermatitis Clinical InterventionsF.6.5 Principles of Compression BandagingF.6.7Resources Best Practice Recommendations for thePrevention and Treatment of Venous Leg Ulcers: Update 2006.Wound Care Canada
Treatment for Venous Stasis DermatitisAvoid SensitizersMoisturizeSeverely DryScaly Skin(Xerosis)Perfume, latex, dyes, lanolin orwool alcohols, balsam of peru,cetylsterol alcohol, parabens,colophony propylene glycol,neomycin, rubber, some adhesives,framycetin or gentamycin (Sibbaldet al. 2007)Glaxal Base (ask pharmacist ifnot on shelf), Cliniderm orMoisturel lotions (not cream) orplain Vaseline petrolatumointment to keep the skinhealthy and free of dry scales.Productscontaining ureasuch as Uremol orAtractain shouldbe used sparinglyStop if any signs ofdermatitis occur.Topical CorticosteroidPreparationsUse for only two weeks at a time(if being applied more frequentlythan 2 x/ week) –they thin the skinover time, making it more likely tobreak down or develop a rebounddermatitis.Client Teaching-Compression for life-Rubbing or scratching aninvolved area (eventhrough the bandage) willextend the rash x 3 moredays (Sibbald et al. 2007)Guidelines for management of different categories of venous eczemaSevere EczemaVery potent corticosteroid for 3-4 weeks emollientInfectedEczemaHighly potentcorticosteroid;antiseptic astringent agent andoral antibioticsMildEczemaWeepingEczemaModerately potentcorticosteroid for 3-4weeksAs for infected butwithout oralantibioticsNo EczemaDaily emollient (unless wrapped)Grey et al. 2006Arrows indicate direction of possible change in condition of eczemaFrom Grey , J.E., Enoch, S., Harding, K.G. 2006 ABC of wound healing Venous and arterial leg ulcers. BMJ 332:347-350.4 South West CCAC Wound Management Program Revised July 2012
Tubigrip/ Tubifast Information and Measuring GuideTubigrip is an interwoven stockinette with covered latex rubber yarns providing compression and support used for joint and venous conditions.Low, low-medium, medium and high compression can be obtained, depending on the size used and the size of the limb that it is applied to.*Wash Tubigrip 3 times only—it loses compression by the 4th wash.If client is unsure about whether they can wear compression, start with one layer or start with low compression and increase as tolerated.Precautions: Do not use in the presence of symptoms of Arterial disease unless the ABPI is 0.6 and/or a wound care expert or vascular surgeon haveassessed the safety.Do not apply Tubigrip over an existing compression bandaging system unless increased compression is the goal.Perform a lower leg assessment including ABPI if you are going to use it for moderate or high compression on the lower legs.Tubigrip-tubular measuring guide for correct sizing to obtain desired compression*Widest widthof limbLOW - 5-10 mm Hg(2 layers same size)Size - CCAC [Mölnlycke]codesMEDIUM – 10-20mm Hg(2 layers same size)Size – CCAC [Mölnlycke]codesHIGH - 20-30 mm Hg(2 layers same size)Alternate sizing method for 10-15 mm Hg** (2 layers)Size & SWCCACAppropriate for**CodeLimb size**Size - CCAC [Mölnlycke]codes10cm - 13.9cm14cm - 14.9cmnoneC-7010 [1443]noneB- 7009 [1436]nonenoneB- 7009 [1436]C-7010 [1443]Small hands and arms15cm - 24cmD -7011 [1437]C-7010 [1443]B- 7009 [1436]D -7011 [1437]25cm - 35cm36cm - 44.9cm45cm - 50cm51cm - 60cm61cm - 70cmE -7012 [1434]F -7013 [1438]G – 7014 [1439]D -7011 [1437]E -7012 [1434]F -7013 [1438]G – 7014 [1439]C-7010 [1443]D -7011 [1437]E -7012 [1434]F -7013 [1438]G – 7014 [1439]E -7012 [1434]F -7013 [1438]Large arms, med. Ankles, small kneesLarge ankles, medium knees, smallthighsG – 7014 [1439]*Information provided by Convatec 2005.Medium arms, small ankles13-16 cm.16-20 cm20-24 cmLarge Knees, medium thighs24-28 cm28-36 cmLarge thighs36-46 cm**Information provided by Molnlycke 2010To achieve graduated 30 mm Hg compression using Tubigrip tubular:1. Use sizing for LOW compression2. Cut first layer to go from above toes to below the knee providing 8 mm Hg.3. Cut second layer to go from the toes to below the knee proving an additional 8 mm Hg.4. Cut the third layer to fit from the toes to above the ankle in the gaiter area, providing a total of 24 mm Hg at the ankle (Melhuish et al ------------------------------------------Tubifast dressing retention bandage does not provide any compression, can be washed many times and can also be used to secure IV tubing.Use as a liner between the skin and the tubigrip to ease the application or hold dressings in place on difficult areas such as elbows or knees.Stretch the tubifast over the affected area- cover area below and above dressing by several cm. for adequate retention.Line colour & SWCCAC CodeRed - 7015Green- 7016Blue -7017Yellow -7018Product Usage**Small limbsSmall and medium limbsLarge limbsExtra-large limbs, heads, children’s trunks5 South West CCAC Wound Management Program Revised July 2012Width3.5 cm5 cm7.5 cm10.75 cm
Application of Simple Unna’s Paste BootGeneral Information & Terminology:Simple Unna’s Paste Boot: Named after German dermatologist Paul Gerson Unna, it consists of a paste bandage containing zinc oxide ointment, 3 to 4 inches wideand 10 yards long (SWCCAC Code 2900)and wrapped in a spiral with fan-folds to prevent constriction and ischemia, and covered by a spiral wrapped kling gauzebandage. It is used for the treatment of venous stasis ulcers and other venous insufficiencies of the leg (Instructions follow)Duke’s Boot: Created at Duke’s University in the late 1980’s, consists of a hydrocolloid dressing over the ulcer, covered by zinc paste bandage in fanfold spiralwrap, orthopedic padding and the original Coban retentive cohesive compression bandage (SWCCAC Code 4200). As of Sept. 2010, this is the ONLY safeapplication for compression with the original Coban that 3M Canada recommends.Modified Duke’s Boot: Consists of a primary dressing over the wound, the zinc paste bandage in fanfold spiral wrap,a layer of orthopedic padding, and a layer ofcompression bandage specified by wound care specialist (e.g the original Coban - retentive cohesive compression bandage (SWCCAC Code 4200) or short-stretchcompression- Comprilan (SWCCAC 4201.02,03,05)Mechanism of Action for Simple Unna’s Paste Boot: - A rigid or inelastic system. The paste bandage hardens over 24 hours to the consistency of cardboard, andprovides hemodynamic support, protecting the skin and potentiating the calf muscle pump action when the individual ambulates. This improves the blood flowparticularly on the deep veins and reduces edema. As the edema reduces, the wraps must be replaced to fit the smaller leg size.Indications: Provides a support system that can be utilized upon admission in the absence of signs of severe ischemia, when ABIs cannot be obtained due toedema or calcified vessels (see Contraindications). Refer to vascular surgeon particularly if there is continuing rest pain. Mixed arterial and venous ulcer with arterial insufficiency: low compression (Burrows et al.2006) for ABI: 0.5-0.8 (Marston and Vowden 2003) (moderate ischemia), Ankle Sprain with venous insufficiency or atrophy Localized atopic dermatitis or venous dermatitis Can be used for mobile or immobile patients, works best if patient is able to ambulate some of the time.PrecautionsAcute skin infectionsHistory of congestive heart failureAtrophy of musclesHistory of dermatitis- many patients are sensitive to some of the constituents of paste bandages, such as parabens preservatives, so it is advisable to patchtest the patient with a small strip of bandage over at least 48 hours.Even if no sensitivity is noted with a patch test, an individual may go on to develop sensitivities on the involved limb, and any increase in dermatitis shouldresult in the paste wrap being discontinued.Contra-indications:If any of the following signs and symptoms are present, do not implement Unna’s Boot without a doctor’s order and a vascular assessment such as ABI’s orsegmental compression studiesPain in legs and feet when laying in bed with legs elevated and relieved by putting leg over the side of the bed or getting up and walking aroundCold legs or feetSymptoms of intermittent claudication (characterized by muscle pain or cramping in the legs triggered by a certain amount of activity, such as walking, butdisappears after a few minutes of rest. The location of the pain depends on the location of the clogged or narrowed artery. Calf pain is most common.)Diabetic microangiopathy (Damage to small blood vessels and capillary circulation causing retinopathy, nephropathy, neuropathy, diabetic foot disease)Dependent rubour/ pallor with elevation6 South West CCAC Wound Management Program Revised July 2012
Application of Simple Unna’s Paste BootLoss of feeling or protective sensation so that the individual could not detect discomfort if the wrap were too tight.AdvantagesDisadvantages Comfortable and soothes skin Sticky sensation in warm weather Protects skin from scratching Contact Dermatitis may occur in some patients Less effective for non-ambulatory patients Pressure decreases with reduced edema (reapply) Cannot absorb large amounts of drainage and exudate may “strike-through” requiring changing. It does not provide compression during periods of inactivity.TechniqueClean the patient's skin thoroughly by washing with tap water (not saline or sterile water) using a mild soap (Dove for sensitive skin) and rinse well. Pat to dry with aclean towel (not 4x4”s).Cleanse the wound as per Sections 10a & b Wound Cleansing Techniques.Add moisturizer to normal skin or topical corticosterioid if ordered for dermatitis. Have patient flex the knee and dorsiflex (toes to nose) the foot to prevent pressureover the tibialis anterior tendon.Apply Unna's boot using a fanfolded layered application without any tension, smoothingthe wrap with your hands using the following method:Start at the base of the toes (metatarsophalangeal joints). Wrap upward in a spiral manner,overlapping about 50% of the previous layer, without pressure, stopping at the lateralside of the leg with each turn, and fold back on itself (see ----- in diagram), avoidingany circumferential wrap that would cause constriction and potential pressure necrosis.This allows for expansion if edema should increase, preventing constriction.You must also allow for spread of the metatarsal bones and heel pad during gait. Continuethe spiral, over the heel and upward to the tibial tubercle, being sure not to compress theperoneal nerve, which is just below the head of the fibula. Each turn must be done at anangle to avoid compromising the circulation.If desired, 6-8 layers of paste wrap can be fanfolded back and forth just over the ulcer to create a semi-occlusive dressing.If bony prominences along anterior foot and leg are evident, use folded gauze to cushion these areas. Finish below tibial tubercle of knee, about 1 inch below theknee. If constriction develops as the dressing hardens, make a 2-inch slit in it below the knee.Place gauze on the outer side of the paste wrap over the ulcer area to absorb exudate and prevent strike-though (Strike-through is defined as the point at whichabsorbed fluid reaches the outer surface or edge of a dressing) (Thomas and Fram 2001)Wrap the Unna's boot with gauze kling-style bandage applied in a figure-8 pattern (this will be less likely to slip and fall down than a spiral wrap).Change q 3-4 days in the first week and decrease as able.Patient Teaching- as per ‘My Venous Ulcer’ booklet.This procedure is from the the CarePartners ET NOW P&P- used with permission. Connie Harris (2008). Editorial assistance Sandra J. Landolt MD FRCPC (Internal Medicine)FRCPC (Dermatology) Consultant in Medical Dermatology and Internal Medicine as pertains to the skin.7 South West CCAC Wound Management Program Revised July 2012
Case ManagerNursingACTIONSETN/WCSACTIONS8 South West CCAC Wound Management Program Revised July 2012
Information about Diabetic Foot Ulcerations (DFU)Neuropathy of the feet in people with diabetes leads to: Changes in muscle and bone alignment causingdeformities and areas of high pressure Loss of protective sensation (LOPS) Callus formationGreater than 85% of lower leg amputations are precipitatedby diabetic foot ulcers (Jones 2006), while 15% of DFUs end inamputation (Snyder et al. 2010). Early detection and appropriate treatment of theseulcers may prevent many amputations. Most DFU’s occur at areas of increased pressure - 90%of diabetic plantar ulcers are attributed to pressure(Orsted, Searles,Trowell et al 2006).Requires multi-disciplinary team approach Assess circulation Offload pressure Debridement Optimize nutritional intake Surgical interventionsKey Points Pain in an insensate foot can signify deepinfection/osteomyelitis Erythema extending more than 2 cm indicates a limbthreatening infection Avoid occlusive dressings (e.g. hydrocolloids) onplantar foot ulcers Manage exudate, prevent contamination through wetdressings and protect peri-wound skin Treat infection immediately(usually needs systemictreatment)9 South West CCAC Wound Management Program Revised July 2012ItemSWCCACDocumentsthat must beusedTreat theCauseTreat the Cause and Resources “My Diabetic Foot Ulcer” - teaching booklet to review withclients “My Wound Care-Diabetic Foot Ulcer”- self-care guide SWCCAC Diabetic Foot Ulcer Care Plan with time-specific goalsOffloading (relieving) the pressure from the ulcer is thecorne
5 South West CCAC Wound Management Program Revised July 2012 Tubigrip/ Tubifast Information and Measuring Guide Tubigrip is an interwoven stoc kinette with covered latex rubber yarns providing compression and support use d for joint and venous conditions. Low, low-medium, medium and high compression can be obtained, depending on the size used and the size of the limb that it is applied to.