Transcription
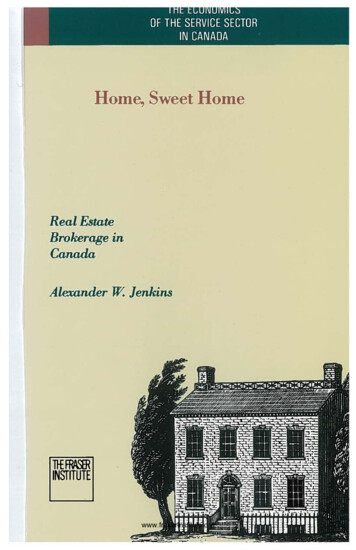
Allysin e. bridgessArAh l. szAnTonAllyson i. evelyn-gusTAveFeliciA r. smiThlAurA n. giTlinHomeSweetHomeInterprofessional Team HelpsOlder Adults Age in Place SafelyPictured: Carol Glover,CAPABLE program participantPhotograph CHRIS HARTLOVEMs.V,68 years old, haschronic bronchitis, depression, andpainful arthritis. She lives in a two-storyrow home in Baltimore with her 20-yearold granddaughter, JJ, and her husband.She needs assistance from JJ to get inand out of the tub and wash her back.She has trouble walking more than twoblocks due to shortness of breath. Shealso experiences pain from bending andstooping due to arthritis, which makesit difficult for her to pick up mail thathas been delivered through the door slotor get pots and pans from low cabinets.Ms. V is the primary caregiver for herhusband, who is recovering from severalstrokes and is not able to leave theirhome. She receives little assistance fromher family, except for JJ. Ms. V used towalk around a nearby reservoir for dailyexercise, but now she rarely walks orgoes anywhere, including her church(a place she loves), because she doesn’thave the time due to caregiving responsibilities, is unable to leave her husbandalone, and has declining endurance.Her time is consumed by caring forOT PRACTICE SEPTEMBER 9, 2013The Baltimore-based CAPABLE program combines the talentsof occupational therapists, registered nurses, and handymento address clients’ self-identified problems in home safety,fall prevention, and basic and instrumental activities ofdaily living.her spouse and doing housework. Mostimportantly to her, she has no timefor herself, especially to take part inorganized social or leisure activities, likegardening or going to church.Ms. V has been in her home formore than 20 years. Her home tourrevealed several issues and challenges.There are eight front steps to enter thehouse, with bilateral railings, and a backturf-covered porch that has seven steps.Ms. V’s living room is tidy and uncluttered, yet there are 13 scatter rugsthroughout her home. In the first floorbathroom, the floor is collapsing, the rugslides, there are no grab bars in the tub,and the tub surface has no tread. Thebasement flooring is loose and torn inmany areas. The washer and dryer aretoo low, and there are no railings on the14 steps leading to the second floor.The ProblemMs. V’s case is not unlike that of themore than 39 million older adults in theUnited States.1 It is estimated that by2050, the same population will morethan double to 88.5 million.1Older adults almost universallyreport wanting to age in their ownhomes. However, as the populationages, so do the homes in which theyreside. Many older adults live on a fixedincome, and they have high fixed costs,such as medical and prescription bills.This can make repairing and maintain119
A Possible soluTionThe Johns Hopkins School of Nursingprogram, called Community Agingin Place, Advancing Better Living forElders (CAPABLE), uses the threepronged approach of an occupationaltherapist, registered nurse, and handyman working in a coordinated fashion toaddress clients’ self-identified problemsin the areas of home safety, fall risk andprevention, and carrying out activitiesof daily living (ADLs) and instrumental ADLs (IADLs). The occupationaltherapy component specifically tacklesdysfunction in ADLs, IADLs, functionalmobility, and leisure and socializationand how the home environment, asdescribed in Ms. V’s case, contributes todaily functional challenges.Through a 4-million, 5-year grantfrom the National Institutes of Health,CAPABLE builds on and extends theAdvancing Better Living for Elders(ABLE) program, a previous occupational therapy intervention with lowincome older adults in Baltimore Citythat was developed by author LauraN. Gitlin and her colleagues at ThomasJefferson University (TJU) and isdesigned to maximize functionality inolder adults aging with a disability.5–7ABLE is currently used by some homecare agencies, including Jefferson ElderCare, a home care program at TJU10that provides evidence-based services.ABLE involves up to five home visitsby an occupational therapist; one homevisit by a physical therapist; and recommendations for and training in homemodifications to address client-identified functional difficulties, home safetyconcerns, fear of falling, and fall risks.In a randomized trial of 319 older adultsin Philadelphia from 2000 to 2005,ABLE reduced functional difficulties,improved home safety, enhanced efficacy in carrying out everyday activitiesat 6 and 12 months, and reducedmortality risk up to 3 years from studyenrollment.5,8 CAPABLE expands ABLEto include two additional components.First, it adds a nurse to help older adultsaddress pain, depression, and medication issues that contribute to functionaldifficulties, to provide strength andbalance training, and to facilitate skills incommunicating effectively with primarycare clinicians about medical issues.9Second, CAPABLE provides homerepairs in addition to home modificationsto address housing conditions that posea risk to daily functioning.CAPABLE involves up to 10 in-homevisits (six occupational therapy visitsand four registered nurse visits) over a4-month period, and the visits are staggered, so that the occupational therapistvisits twice before the registered nursevisits for the first time. The first two visitsfocus on evaluating the participant andthe home, and the later visits focuson providing education, identifyingbarriers to function as directed by theclient, making goals, solving problems,and conducting training. All visits arecustomized to the particular functionalneeds of the participant. Followinga home evaluation conducted by theoccupational therapist, the handymanreceives instructions on home repairs;modifications; and assistive devices,assistive technology, or durable medicalequipment specified by the occupationaltherapist. The handyman’s organization, CivicWorks, in Baltimore, ordersthe items, with an average of 1,200 ingrant money covering the materials andlabor. CivicWorks is also an AmeriCorpssite and therefore is able to provide anapprentice plus an experienced handyman for the cost of one handyman.As in ABLE, an essential feature ofCAPABLE is that the areas addressedare driven by the client and his or herself-perceived needs. Also, there isinterdisciplinary coordination, as teammembers consult one another regularlyvia e-mail, text messages, phone calls,and in-person team meetings. One of theoccupational therapists is the centralliaison for all issues with the handymanaspect of CAPABLE and receives weeklyupdates to ensure that the client’s goalsare being met in a coordinated fashion.For more on this process, see Table 1 onpage 11.On the first visit, the occupationaltherapist issues the participant a folderSEPTEMBER 9, 2013 WWW.AOTA.ORGPhotograph CHRIS HARTLOVEing a home difficult. Low-income andminority older adults are also morelikely to live in deteriorated housing2and to lack the resources necessary tomodify their homes to compensate fortheir declining capabilities.At the federal, state, and local levels,there are few programs that addressboth appropriate housing and healthneeds for seniors, as they usuallyaddress one or the other but do notlink health needs and housing conditions.3 Because housing conditions canpose health hazards and functionalchallenges,4 both the person and theenvironment are important considerations when helping older adults staysafe and independent in their ownhomes. To address this gap in the careof older adults, a team of researchers atthe Johns Hopkins Center for InnovativeCare in Aging is testing a program thatincludes occupational therapists, registered nurses, and handymen.
Table 1. oT, hm, and rn visits over a 4-month Period for each cAPAble clientoccupational therapist (oT)and participant togetherhandyman andapprenticeregistered nurse (rn)and participant togethervisit 1*Introduction; evaluate activities of daily living (ADLs)and instrumental ADLs and mobility; issue fall prevention and recovery pamphlet (from CDC).Introduction and assessment of pain,mood, strength, balance, polypharmacyand primary care provider access/communication.visit 2Determine goals and conduct house tour/evaluation.Determine goals together, start to brainstorm goal #1.After visit 2Develop work order for handyman (HM). Send to HMand receive pricing.Review medication list, including interactions and possible deletions.visit 3Brainstorm and develop action plan with client foridentified goal #1.visit 4Brainstorm and develop action plan with client foridentified goal #2; issue assistive equipment/durablemedical equipment when available.visit 5Brainstorm and develop action plan with client for identified goal #3; review HM work with participant.visit 6Wrap up, help participant generalize solutions for futureproblems; review goals.HM conductssite visit thengives OT pricing;starts work andcontinues untilcomplete.Brainstorm and provide develop actionplan for client identified goal #2.Brainstorm and provide action plan forclient identified goal #3.*The visits are staggered so that OT visit 1 and 2 occur before RN visit 1. RN has four visits; the OT has six.to keep CAPABLE appointment calendars, hard copies of the brainstormingand action plans the participant doeswith the registered nurse and occupational therapist, and fall preventionpamphlets for reference. To date, allclients have preferred paper copies, butelectronic versions are also offered. Theparticipant and occupational therapistuse a standardized assessment tool,the Clinician and Client AssessmentProtocol (C-CAP), initially developed inABLE,10 in which the client and occupational therapist work together to identifyareas of concern. Specifically, the areasexamined include:1. ADLs: bathing, grooming, eating anddrinking, toileting, taking undergarments on and off (hooks, fasteners,buttons, zippers, snaps), takingclothing on and off, donning anddoffing socks and shoes (includingVelcro and ties), resting and sleeping,and engaging in sexual activity2. IADLs: housekeeping, bed making,washing dishes by hand, groceryOT PRACTICE SEPTEMBER 9, 2013shopping, using the telephone, takingmedicines, managing finances, maintaining health, prepping and cleaningfor meals, caring for pets, participating in leisure activities, workingor volunteering, and participating inorganized social activitiesThe participant works with theoccupational therapist to set threegoals based on difficulties found in theself-report and observation during theC-CAP. On the next visit, the occupational therapist finalizes goals with theparticipant and completes a home-riskevaluation, plus introduces fall prevention and recovery strategies.To address the participant’s chosen goals, the occupational therapistbrainstorms and develops an action planwith the client to discover why problemsmay be occurring, what the possibilitiesare of fixing them, and two things theclient will implement for the upcomingweek or two until a strategy that worksis established. At the end of all six of theoccupational therapy sessions, the clientreceives a booklet of strategies, initiallydeveloped in ABLE and now expandedto include a broader range of tipsreflecting the nurse component (givenby the registered nurse on the last visit)that is also reviewed by the occupationaltherapist with the client, focusing onADLs, falls, and safety.To complement the occupationaltherapy work on functional goals, thenurse addresses medical issues thatinhibit daily function, such as pain,mood, medication adherence and sideeffects, and strength and balance. Forexample, when a client has pain thatinterferes with his or her ability to cook,the registered nurse reviews currentpain medication, tailors an exerciseprogram suited to the individual, andencourages increased communicationwith the client’s primary care providerto address unresolved pain. The occupational therapist evaluates the need forassistive devices, assistive technology,and/or durable medical equipment;11
examines environmental factors thatcould exacerbate pain while standingor sitting; and introduces strategies todecrease pain while the client performsIADLs (e.g., recommending weightshifting or sitting vs. standing, orderinga high back chair with arms). Then theoccupational therapist gets the handyman involved for any modifications thatcould be implemented (e.g., lowering orraising a cooking surface, checking forfloor stability).improved ability to perform their ADLsand IADLs. The number of domains theyreported difficulties in improved from anaverage of 2.1 ADL difficulties at baseline to 0.7 ADL difficulties postintervention, and from an average 2.3 differentIADL difficulties to 1.2 postintervention,along with a decrease in their fear offalling. Of those who received CAPABLEservices, 100% indicated it helped them,and 94% stated that their lives had beenmade easier, their quality of life hadWhereas traditional occupational therapy andregistered nurse home care is client centered,CAPABLE is client directed.CAPABLE differs from traditionalhome care in important ways. InCAPABLE, the attention is directed tothe ability of the person to function inhis or her home environment versusaddressing a specific injury or impairment. The occupational therapist acts asa consultant, observing and discussingwith clients the difficulties they encounter performing valued daily activities.Importantly, the condition of the homeitself is considered in terms of how itcan best support the client. Whereastraditional occupational therapy andregistered nurse home care is client centered, CAPABLE is client directed. Thisis an important difference. The functional areas addressed are those that theclient self-identifies as most important.Personal goals such as walking arounda nearby lake or getting to church atleast twice a month become the focus oftreatment.CAPABLE was initially tested in aJohns Hopkins University InstitutionalReview Board–approved pil
Home Sweet. Allysin e. bridges sArAh l. szAnTon Allyson i. evelyn-gusTAve. Home. FeliciA r. smiTh lAurA n. giTlin. Interprofessional Team Helps Older Adults Age in Place Safely . Pictured: Carol Glover, CAPABLE program participant. 10 SEPTEMBER 9, 2013 WWW.AOTA.ORG. ing a home difficult. Low-income and minority older adults are also more likely to live in deteriorated housing2 and to lack .