Transcription
GUIDELINES ON THE CARE OF URINARY CATHETERS(URETHRAL & SUPRA-PUBIC)Version NumberV1Date of IssueDecember 2018Reference NumberCUCUS-12-2018-CHFQ-V1Review Interval3 yearlyApproved BySignatureDate:SignatureDate: December 2018SignatureDate: December 2018Name: Prof Feargal QuinnTitle: Consultant UrologistName: Fionnuala O’ NeillTitle: Nurse Practice Development CoordinatorAuthorised ByName: Rachel KennaTitle: Director of NursingAuthor/sName: Carol Hilliard, Nurse Practice DevelopmentCoordinatorName: Prof Feargal Quinn, Consultant UrologistLocation of CopiesOn Hospital Intranet and locally in departmentDocument Review HistoryReview DateReviewed BySignatureDr Mary WaldronJuly 2017Michelle O’Gorman, CNFTess Farrelly, CNSpDocument Change HistoryChange to DocumentReason for ChangeInclusion of care bundleIn line with local procedures, and national and international guidanceTo ensure best available evidence is usedUpdating of evidenceDepartment of Nursing
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 2 of 19CONTENTSPage Number1.0Introduction42.0Definition of Guideline43.0Applicable to44.0Objectives of the Guideline45.0Definitions / Terms46.0Guidelines on the care of urinary catheters6.1 Indications for Catheterisation56.2 Complications of Urinary Catheterisation56.3 Meatal cleansing before catheter insertion56.4 Insertion of an Indwelling Urethral Urinary Catheter66.5 Care of an Indwelling Urinary Catheter86.6 Obtaining a Catheter Sample of Urine106.7 Removal of an Indwelling Urinary catheter116.8 Care of a Supra-Pubic Catheter for Urodynamics Studies127.0Urinary Catheter Care Bundle148.0Special Considerations159.0Companion Documents1510.0Implementation Plan1511.0Evaluation and Audit1512.0References16Appendix 1: Outline of commonly used catheter materialsAppendix 2: Urinary Catheter Troubleshooting GuideAppendix 3: Urinary Catheter Care Bundle171819
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 3 of 191.0IntroductionUrinary catheters are a common and vital intervention in the acute clinical setting. However, catheterassociated urinary tract infection is one of the most common healthcare associated infections (SARI2011). Healthcare professionals can play a key role in reducing and preventing the risk of catheterrelated infections.2.0Definition of GuidelinesUrinary catheterisation is defined as an intervention to enable emptying of the bladder by insertion of acatheter. Catheterisation may be indwelling or intermittent. Indwelling urinary catheterisation iscategorised as either short-term (in situ less than 28 days) or long-term (in situ greater than 28 days).These Urinary Catheter Guidelines represent the written instructions about how to ensure high qualitycare is provided. Guidelines must be accurate, up to date, evidence-based, easy to understand, nonambiguous and emphasise safety. When followed they should lead to the required standards ofperformance.3.0Applicable toThese guidelines are applicable to all registered nurses and nursing students involved in the insertion,care and removal of intermittent or indwelling urinary catheters.4.0Objectives of the GuidelinesThe purpose of the Urinary Catheter Guidelines is to promote safe, effective and consistent practice inrelation to Urinary Catheters.5.0Definitions / TermsUrinary catheterisation: an intervention to enable emptying of the bladder by insertion of a catheter.Short-term indwelling urinary catheter: catheter is in situ less than 28 daysLong-term indwelling urinary catheter: catheter is in situ greater than 28 days.Urinary catheter: a soft hollow tube which is inserted into the bladder for the purpose of draining urineor instilling fluid. The catheter may be introduced via the urethral or suprapubic route (via abdominalwall), or via a surgically constructed channel (Mitrofanoff). Catheters are made from different materialswhich influence their selection and use (Appendix 1).Supra-pubic catheter: a urinary catheter inserted, through an artificial tract in the abdominal wall, justabove the pubic bone and into the dome of the bladder.Urinary tract infection (UTI): an infection involving any part of the urinary system, including urethra,bladder, ureters, and kidney.Catheter associated urinary tract infection (CAUTI): UTI associated with a urinary catheterClean intermittent catheterisation (CIC): insertion and removal of a catheter several times a day topromote urinary continence
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary catheters6.0Reference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 4 of 19Guidelines on the care of urinary catheters6.1 Indications for Catheterisation: Monitor urinary outputManage urinary retentionPost urological, pelvic or abdominal surgeryDiagnostic purposes, e.g. urodynamics or x-ray interventionDuring epidural analgesiaTo promote healing of a sacral or perineal wound, where appropriateFacilitating continence / maintaining skin integrity (when all treatment methods have failed)(McQueen et al. 2012, RCN 2012)6.2 Complications of Urinary Catheterisation: InfectionBladder spasmTraumaUrethral perforationUrethral strictureBypassing, i.e. urine leakingaround catheter HaematuriaErosion of the bladder wallCatheter encrustationBladder calculiAltered body imageAllergy to Latex6.3 Meatal cleansing before catheter insertionThere is some debate in the literature and in practice about the use of antiseptic solution versus sterilesaline for meatal cleansing before insertion of a catheter. While some guidelines recommend that there isno clinical advantage to using antiseptic solutions to prepare the meatus (Loveday et al. 2014), the issueremains unresolved (SARI 2011).In OLCHC, if a child has a urology, nephrology or other condition which increases their risk of CAUTI,antiseptic solution should be used to prepare the meatus before the insertion of a catheter. Similarly, if achild requires catheterisation for Micturating Cystourethrogram, an antiseptic solution should be used toclean the urethral orifice before catheterising. For other children, sterile saline is sufficient. Discuss with theUrology or Nephrology Team if in doubt.6.4 Insertion of an Indwelling Urethral Urinary CatheterDue to the risk of CAUTI, the decision to catheterise should only be taken after there is full consideration ofthe implications of the procedure, and when there is no alternative (SARI 2011, Loveday et al. 2014, NICE2014).In OLCHC doctors catheterise male patients when indwelling catheters are required. Nurses may insert anindwelling catheter in female patients. The healthcare professional must have acquired the necessaryknowledge and skill prior to insertion, caring for, or removing a catheter. Each nurse must assess if the skillis within her/his scope of practice (Nursing & Midwifery Board of Ireland (NMBI) 2015b). The insertion ofindwelling urinary catheters must be carried out in accordance with the ‘Guidelines for Prevention of Abuse
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 5 of 19of Children in Hospital’ (OLCHC 2007).When reasonable efforts to catheterise fail, the procedure is discontinued. In OLCHC it is recommendedthat catheterisation should be attempted only once in an occurrence. Because of the risks of urethraloedema, subsequent attempts are likely to prove increasingly painful and may be unsuccessful. In thisinstance, consult the paediatric urology team.Standard precautions must be used by all healthcare professionals when caring for a child with a urinarycatheter (OLCHC 2011, SARI 2011).EquipmentTrolley (cleaned with soap/water & disinfected with Chlorhexidine Gluconate 0.5% w/v in 70% alcohol v/v)Disinfection wipeSterile catheterisation pack containing receiver, gauze, fenestrated drape i.e. drape with pre-cut hole Sterile anaesthetic gel or K-Y Gel 0.9% Saline or antiseptic solution for cleansingmeatus (See Section 6.3) Sterile catheter of appropriate size Sterile 5ml syringe Sterile drainage bag and stand 10ml vial of sterile water (to inflate balloon) Powder free sterile gloves Adhesive tape or catheter fixation deviceACTIONRATIONALE & REFERENCEAssess the child in relation to need for To reduce the risk of CAUTI, only catheterisecatheterisation, and the type, length and size of when clinically indicated and after other methodscatheter to be used.of management have been considered. Lovedayet al. 2014 NICE 2014Use the smallest gauge catheter which will allow To prevent urethral trauma Loveday et al. 2014urinary outflow.To help prepare and support them for theExplain the procedure to the child and parentsprocedure Hockenberry et al. 2016All efforts must be made to protect the privacy To protect the child’s best interests OLCHC 2007and dignity of the child during the procedureClean meatal area with soap, water and clean To prevent contamination of the urethra SARIcloth. This may be done during a bath.2011, Loveday et al. 2014Position child comfortably.Female: Lying flat with knees flexedTo facilitate insertion of the catheter andmaintain child’s comfort McQueen et al. 2012Male: Semi-recumbentOpen equipment onto prepared trolleyFrom this point use Aseptic Non-Touch Hand hygiene and ANTT Technique areTechnique (ANTT) Level 2 when performing this essential to prevent infection SARI 2011,
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 6 of 19procedureOLCHC 2017, Loveday et al. 2014Perform antiseptic hand hygiene before applyingsterile glovesAttach drainage bag to catheter before insertionClean meatal area with sterile salineantiseptic solution as appropriateTo maintain a closed system Loveday et al. 2014OR To reduce the risk of introducing infection SARI2011, Urology/Nephrology Teams 2013Female: Separate labia majora. Clean urethralorifice in downward strokes using gauze andcleansing solutionMale: Retract foreskin (if present). Clean the This is age dependent and the foreskin shouldglansnever be forced back.Place fenestrated drape over genital areaTo create a sterile field SARI 2011Apply single use lubricating gel to the tip of the To reduce discomfort, to facilitate the insertion ofcatheter and the urethral orifice.the catheter and to prevent urethral traumaMcQueen et al. 2012 Loveday et al. 2014If using anaesthetic lubricating gel *Female: place on gauze square and lay gauze Full local anaesthetic effect is achieved within 510minutes of application of anaesthetic gel.over urethral orificeManufacturer’s InstructionsMale: inject into urethra using nozzle*Follow manufacturer’s dosing guidelinesGently introduce the catheter into the urethral This ensures the catheter is not misplaced in theorifice. When urine flows, advance the catheter urethrauntil urine flows freely (approx 2.5cms)Inflate the balloon with the correct amount of Fluid may leak via the balloon membrane. Oversterile water as specified by the manufacturer.inflating the balloon may cause trigonal irritation,incomplete drainage of the bladder and ruptureDO NOT over inflate the balloonof the balloon Trigg & Mohammed 2011Always ensure urine is flowing before inflating the To avoid inflating the balloon in the urethraballoonSecure catheter to the abdomen or groin using To minimise trauma to the urethral meatus andadhesive tape or a catheter fixation devicebladder neck. Trauma is a particular risk if childmobilises with a catheter which is incorrectlysecured McQueen et al. 2012Secure the drainage bag to the child’s abdomen Prevents accidental dislodgement of catheterusing tape and attach to the standmeatal trauma Trigg & Mohammed 2011Praise and thank the childTo maintain the trusting relationship with thechild Hockenberry et al. 2016Discard the equipment in the Healthcare Non-risk OLCHC 2014waste (Household Waste) unless contaminatedwith blood.
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 7 of 19Record the intervention in child’s healthcarerecord: reason for catheterisation, time and date catheter was inserted & bywhom, anydifficultiesexperiencedduringprocedure, number of attempts to catheterise if urine specimen was obtained, size of catheter & balloon inflation volume, volume of urine drained when to remove catheterTo ensure all staff are aware of the catheter careneeds of the child SARI 2011, McQueen et al.2012, Loveday et al. 2014To ensure effective communication throughaccurate recording of care. NMBI 2015a6.5 Care of an Indwelling Urinary CatheterThe principal aim of effective catheter care is to prevent infection and minimise complications (SARI 2011,McQueen et al. 2012, Loveday et al. 2014). Please refer to Appendix 2: Troubleshooting Guide to manageproblems that arise.ACTIONRATIONALE & REFERENCEAll efforts must be made to protect the privacy To protect the child’s best interests OLCHC 2007and dignity of the child who is catheterisedStandard precautions must be applied by all To prevent infection SARI 2011healthcare professionals when caring for a urinarycatheterUse Aseptic Non-Touch Technique (ANTT) Level To prevent infection OLCHC 20173 when providing catheter care unless “breaking”a connection, e.g. changing drainage bag, whenANTT Level 2 is used.All healthcare professionals should perform To prevent infection OLCHC 2017antiseptic hand hygiene before and after anyinteraction with the catheter or drainage bag.Maintain a closed urinary drainage systemChoose a drainage system appropriate to thechild’s needs:Patient on bed-rest: 24 hour drainage bagAmbulant patient: leg-bag by day. Connect a 24hour drainage bag to the leg-bag at nightPatient requiring close monitoring of output:drainage bag with an hourly urometerTo reduce risk of infection SARI 2011
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 8 of 19Position urinary drainage bag below the level of To promote drainage and prevent backflow ofthe bladderurine into bladder Loveday et al. 2014Ensure drainage bag is not touching the floorTo prevent contamination Gould et al. 2009, SARI2011Empty the drainage bag using a clean container To prevent contamination Gould et al. 2009 SARI(separate container for each patient).2011Avoid splashing and avoid contact between thedrainage tap and the container.Cleansing Catheter SiteTo prevent contamination of the catheter andprevent infection SARI 2011Urethral catheter: Wash or shower child daily tomaintain meatal hygiene.Expert opinion and international guidelinesindicate that there is no advantage to usingFor the child on bed-rest, clean urethral meatusantiseptic solutions for meatal cleansing comparedwith soap and water.with routine bathing / showering / washing GouldAdditional meatal hygiene is needed if child soils. et al. 2009, SARI 2011, Loveday et al. 2014When attending to child’s hygiene, leave drainage To maintain closed system drainagebag attached and dry the bag.To prevent infection SARI 2011, OLCHC 2013,Supra-pubic Catheter: ANTT Level 2 should beMcQueen et al. 2012used when caring for insertion site until it ishealed, after which Level 3 ANTT may be used.Cleanse site using sterile saline and apply asterile dressing if necessary.To prevent infection SARI 2011, McQueen et al.Once the supra-pubic insertion site is healed, it2012may be nursed exposed and washed daily withwarm soapy water.Changing the Drainage Bags24hour drainage bags:change weeklyLeg-bags:change weeklyOvernight drainage bags: change dailyAs per manufacturer’s instructionsThis should be clearly documented in thepatient’s healthcare record.Note: Change bag if visibly soiled or if bag To prevent contamination Gould et al. 2009,becomes disconnectedMcQueen 2012Desired urinary output isInfant/child:1-2ml/kg/hourAdolescent: 0.5-1ml/kg/hourThese values are generally accepted normalranges but may vary depending on the child’sclinical condition. Assess each child according tohis/her intake and insensible fluid losses.
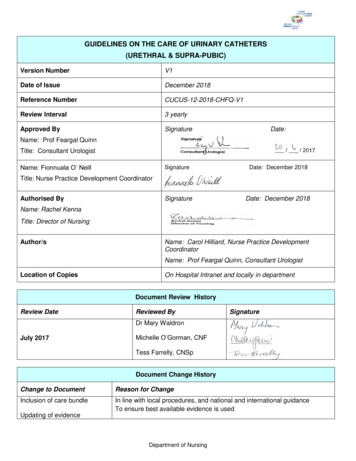
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 9 of 19Flushing of urinary cathetersRoutine flushing of indwelling urethral catheters is Flushing of catheters exposes the child to thenot recommended practice.introduction of infection to the bladder as well asthe discomfort that can be associated with theprocedure.Prevention of catheter blockage by ensuring aCaution: Flushing of catheters should only begood fluid intake and maintaining satisfactoryperformed post reconstructive urological surgeryurine drainage is of paramount importance.or on the specific instructions of the surgicalteam.6.6Obtaining a Catheter Sample of UrineA catheter sample of urine should only be taken when clinically indicated (SARI 2011). A sampling port on theurine drainage bag enables a urine sample to be obtained without opening the drainage system. Maintaininga closed system helps to prevent infection (SARI 2011).Equipment: 5ml sterile syringe Sterile orange needle Swab impregnated with chlorhexidine gluconate 2% in 70% isopropyl alcohol Urine specimen jar Non sterile glovesACTIONRATIONALE & REFERENCEExplain procedure to child/parentTo help prepare and support them for theprocedure Hockenberry et al. 2016All efforts must be made to protect the dignity of thechildTo protect the best interests of the child OLCHC2007Only obtain sample from specific sampling port on To avoid damage to catheter and to prevent thedrainage bag. (See Fig.1 below)introduction of infection, SARI 2011, Loveday etal. 2014Do not open drainage system to obtain sample.To maintain closed system. SARI 2011Use Aseptic Non-Touch Technique Level 3 when To prevent risk of infection. OLCHC 2017performing this procedurePerform hand hygiene and apply glovesTo prevent cross infection. OLCHC 2010Disinfect sampling port with impregnated swab and To prevent contamination of sampleallow to dry.Using needle and syringe aspirate the requiredamount of urine from the sampling port.
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 10 of 19Send specimen to laboratory.As per “Collection of Specimen” guideline toobtain microbiological or biochemical analysisof sample.Praise and thank the child for their cooperation.Record the intervention in the child’s healthcare To ensure effective communication throughrecord:accurate recording of care. NMBI 2015a time and date of sample, any difficulties experienced during procedure.Fig.1 Example of a urinary drainage bag with a sampling port6.7Removal of an Indwelling Urinary catheterThe longer a catheter remains in situ, the greater the risk of CAUTI. Assess the child daily to ensure thecatheter is removed at the earliest opportunity (SARI 2011, RCN 2012, Loveday et al. 2014).There is suggestive, but inconclusive evidence from research on adults that removal of a catheter at midnight,rather than early morning, is of benefit (Griffiths and Fernandez 2007). Slow filling of bladder overnight mayallow for easier voiding in the morning, and allows time to deal with problems, such as retention, which mayarise during the day. Until stronger evidence becomes available the time of catheter removal should bedetermined by patient needs and clinical indications.EquipmentNon-sterile gloves5ml sterile syringeAdhesive removal spray or wipesContainer for emptying drainage bagWater and disposable gauze/cloth
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 11 of 19ACTIONExplain procedure to child/parentRATIONALE & REFERENCETo help prepare and support them for theprocedure Hockenberry et al. 2016All efforts must be made to protect the dignity and To protect the best interests of the child OLCHCprivacy of the child2007Note: Empty catheter bag before removal.To measure output. To permit safe immediatedisposal of equipment following removal.Use Aseptic Non-Touch Technique Level 3 when To prevent infection. OLCHC 2017performing this procedurePerform hand hygiene and apply glovesTo prevent cross infection. OLCHC 2017Clean urinary meatus using water and gauze or cloth.To prevent risk of introducing infection Trigg &Mohammed 2011Remove adhesive tapes using removal spray / wipes.To allow easier removal of catheterRemove water from balloon using syringe (check care- To ensure balloon is completely deflatedplan to confirm volume).If the balloon does not deflate:Slide the plunger of the syringe up and down the barrel Prevents the plunger from adhering to the front ofof the syringe several times to “loosen it up.”the syringe barrel.Compress the plunger all the way and then pull backthe plunger slightlyGently insert the syringe in the catheter valve. Allow Aspiration that is too rapid, or too forceful, maythe pressure within the balloon to force the plunger cause the inflation lumen within the Foley catheterback and fill the syringe with water.to collapse (Bard 2012)Ask child to breath in and out –gently remove catheter To relax pelvic floor muscles, allowing easieron exhalation.removal of catheterClean urinary meatus using water and clothTo prevent risk of infection Loveday et al. 2014Discard equipment appropriately.Dispose of catheter and drainage bag inHealthcare Non-risk Waste. If contaminated withblood, dispose of in Healthcare Risk WasteOLCHC 2014Record intervention in the child’s healthcare record; time/date catheter was removed and by whom any difficulties experienced during procedure if urine specimen was obtained volume of urine drained prior to catheter removalTo ensure effective communicationaccurate recording of care. NMBI 2015athrough
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 12 of 196.8Care of a Supra-Pubic Catheter for Urodynamics StudiesA supra-pubic catheter is a urinary catheter that is inserted, through an artificial tract in the abdominal wall,just above the pubic bone and into the dome of the bladder.Urodynamic studies are a diagnostic investigation of the lower urinary tract in order to measure bladderpressure and urine flow rate during bladder filling and voiding. This enables the assessment of theneuromuscular function and dysfunction of the urinary tract, and identify the cause(s) of urine storage andvoiding dysfunction (Clements et al. 2013).Supra-pubic catheterisation for UrodynamicsA double lumen cystometric supra-pubic catheter is a catheter inserted for the purpose of performingUrodynamics. In OLCHC the decision to insert a supra-pubic catheter is made by the Urology team. Insertionof a supra-pubic catheter for urodynamics is always performed in theatre under general anaesthetic.As these catheters do not have a retaining balloon, they are held in situ using a suture and retention dressing.The retention dressing should be left undisturbed except on the instruction of the Surgeon/C.N.SUrodynamics. There may be leakage of urine from the catheter insertion site post-operatively: in this case theretention dressing should be re-enforced but not removed.The catheter is usually inserted the day before the test and removed once the test is completed. Removal isusually performed by the Nurse Specialist who performs the urodynamics test. A pressure dressing is appliedto the insertion site after removal of the catheter and left in situ for 24 hours.Complications associated with Supra-pubic Catheters Catheter related urinary tract infection Erosion of the bladder wall Bladder spasm Catheter encrustation Bypassing, i.e. urine leaking aroundcatheter Injury to abdominal organs Altered body image Expulsion Haematuria(Ahluwalia et al. 2006, Harrison et al. 2010)Types of CatheterThe catheter used in this hospital for urodynamics is a double lumen cystometric supra-pubic catheter. Thesupra-pubic urodynamics catheter is sent to theatre with the child.These catheters are only available in the Urodynamics Department. Please contact either the Urology CNSson bleep 8592 to obtain same. All catheters should be used in accordance with manufacturer's instructions.
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 13 of 19ActionRationale & ReferenceExplain procedure to child/parentTo help prepare and support them for theprocedure Hockenberry et al. 2016All efforts must be made to protect the dignity andprivacy of the childTo protect the best interests of the child OLCHC2007Pre-operative careThe Urology team/C.N.S Urodynamics will assess Only catheterise when clinically indicated tothe child to determine the need for a suprapubic prevent undue trauma and risk SARI 2011catheter for urodynamics.Attend to the child’s routine pre-operative care To prevent risk of infection during surgeryensuring child has had shower/bath prior tosurgery.Post-operative care:ANTT Level 2 should be used when caring for To prevent infection, SARI 2011, McQueen et al.2012, OLCHC 2017insertion site until it is healed.Use ANTT Level 3 when caring for the supra-pubiccatheter unless you are “breaking” a connection, inwhich case ANTT Level 2 should be used.Perform antiseptic hand hygiene before and after To prevent infection OLCHC 2017any handling of the catheter.The supra-pubic catheter is double-lumened, both The catheter is not usually required for drainageof which will be clamped. The catheter is not purposesconnected to a drainage system.The child can urinate per urethra unless otherwiseindicated. The child can also mobilise as normal.Care of the insertion site:A dressing will be in situ around the catheter To absorb leakage or exudate SARI 2011insertion site post-operatively.Do not remove or disturb the dressing as it holdsthe catheter in place. If site is oozing reinforce thedressing.If the child complains of bladder pain which is not These medications may alter the Urodynamicresolved with analgesia, then a relaxant such as results.Diazepam can be administered.NOTE: Children with supra-pubic Urodynamiccatheters in situ should not receive anti-cholinergicmedicationRemoval of catheter This is performed by the Urology CNSs aftercompletion of the Urodynamics test.
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 14 of 19 Prepare child and parents for procedure. To reduce the pain associated with theAssess the child’s level of pain and administer procedure, thus increasing the child’s comfortappropriate analgesia. Remove dressing using adhesive remover. Clean site using sterile saline and gauze. To absorb any leakage and to protect insertionCut suture if present and remove catheter by site. Note: it is not unusual for the entry site toooze urine for 2-3 hours post removal.pulling same using slow steady movement. Clean site using saline and gauze. Apply appropriate dressing to entryDressing can be removed in 24hrs.Discard equipment appropriately.site.Dispose of catheter and drainage bag inHealthcare Non-risk Waste. If contaminatedwith blood, dispose of in Healthcare RiskWaste OLCHC 2014Child should be encouraged to have a good fluid To ensure good bladder emptying with nointake following removal of the catheter.bladder irritation. Sometimes post removal ofcatheter the child may have some haematuriaIf concerned contact urology team.which usually resolves with good fluid intake.Praise and thank the child, and ensure he/she is To maintain a trusting relationship between thecomfortable.child and nurse, and to promote the child’scomfort Hockenberry et al. 2016Record intervention in the child’s healthcare record; To ensure effective communication through Date/Time of catheter insertion and removal accurate recording of care. NMBI 2015a Date and outcome of Urodynamic test Anydifficultiesexperiencedduringprocedure If urine specimen was obtained7.0Urinary Cather Care BundleCatheter associated urinary tract infection (CAUTI) is one of the most common healthcare associatedinfections (SARI 2011). Healthcare professionals can play a key role in reducing and preventing the risk ofcatheter related infections. A urinary catheter care bundle consists of a group of evidence based interventionswhich when fully implemented are known to decrease the incidence of CAUTI and result in improvedoutcomes (SARI 2011, OLCHC 2015).
Our Lady’s Children’s Hospital, CrumlinDocument Name: Guidelines on the care of urinary cathetersReference Number: CUCUS-12-2018-CHFQ-V1Version Number: V1Date of Issue: December 2018Page No: Page 15 of 197.1Care Bundle ComponentsThe care bundle strategies used in OLCHC include (see Appendix 3 for Care Bundle document):1.2.3.4.5.6.7.7.2Assess the need for a urinary catheter on each shiftHand hygiene is pe
7.0 Urinary Catheter Care Bundle 14 8.0 Special Considerations 15 9.0 Companion Documents 15 10.0 Implementation Plan 15 11.0 Evaluation and Audit 15 12.0 References 16 Appendix 1: Outline of commonly used catheter materials Appendix 2: Urinary Catheter Troubleshooting Guide Appendix 3: Urinary Catheter Care Bundle 17 18 19