Transcription
Medicare Secondary PayerFact Sheetfor Provider, Physician, andOther Supplier Billing StaffBackgroundMaintaining the viability and integrity of the Medicare Trust Fund becomes critical as the Medicare Programmatures and the “baby boomer” generation moves toward retirement. Providers, physicians, and othersuppliers can contribute to the appropriate use of Medicare by complying with all Medicare requirements,including those applicable to the Medicare Secondary Payer (MSP) provisions. The purpose of this fact sheetis to provide a general overview of the MSP provisions for individuals involved in the admission and billingprocedures at provider, physician, and other supplier settings.What Is Medicare Secondary Payer (MSP)?Since 1980, the Medicare Secondary Payer (MSP) provisions have protectedMedicare funds by ensuring that Medicare does not pay for services anditems that certain health insurance or coverage has primary responsibilitiesfor paying. The MSP provisions apply to situations when Medicare is notthe beneficiary’s primary insurance. It provides the following benefits forboth the Medicare Program and providers, physicians, and other suppliers: National program savings – Medicare saves more than 6 billion annuallyon claims processed by insurers that are primary to Medicare. Increased provider, physician, and other supplier revenue – Providers,physicians, and other suppliers that bill a liability insurer before billingMedicare may receive more favorable payment rates. Providers,physicians, and other suppliers can also reduce administrative costswhen health insurance or coverage is properly coordinated. Avoidance of Medicare recovery efforts – Providers, physicians, andother suppliers that file claims correctly the first time may preventfuture Medicare recovery efforts on that claim.To realize these benefits, providers, physicians, and other suppliers musthave access to accurate, up-to-date information about all health insuranceor coverage that Medicare beneficiaries may have. Current law andregulations require that all entities that bill Medicare for services or itemsrendered to Medicare beneficiaries must determine whether Medicare isthe primary payer for those services or items.1
When Does Medicare Pay First?Primary payers are those that have the primary responsibility for paying a claim. Medicare remains the primarypayer for beneficiaries who are not covered by other types of health insurance or coverage. Medicare isalso the primary payer in other instances, provided several conditions are met. Table 1 lists some commonsituations when Medicare may be the primary or secondary payer for a patient’s claims.Table 1. List of Common Situations When Medicare May Pay First or SecondIf the patient.And thiscondition exists Then this programpays first And this programpays secondIs age 65 or older, and is covered by a GroupHealth Plan through current employment orspouse’s current employment The employer has less than20 employees MedicareGroup Health PlanIs age 65 or older, and is covered by a GroupHealth Plan through current employment orspouse’s current employment The employer has 20 or moreemployees, or at least oneemployer is a multi-employergroup that employs 20 ormore individuals Group Health PlanMedicareHas an employer retirement plan and is age65 or older or disabled and age 65or older The patient is entitledto Medicare MedicareRetiree coverageIs disabled and covered by a Large GroupHealth Plan through his or her own currentemployment or through a family member’scurrent employment The employer has less than100 employees.MedicareLarge GroupHealth PlanIs disabled and covered by a Large GroupHealth Plan through his or her own currentemployment or through a family member’scurrent employment The employer has 100 ormore employees, or at leastone employer is a multiLarge Group Health Planemployer group that employs100 or more individuals MedicareHas End Stage Renal Disease and GroupHealth Plan Coverage Is in the first 30 months ofeligibility or entitlementto Medicare Group Health PlanMedicareHas End Stage Renal Disease and GroupHealth Plan Coverage After 30 months MedicareGroup Health PlanHas End Stage Renal Disease andCOBRA coverage Is in the first 30 months ofeligibility or entitlementto Medicare.COBRAMedicareHas End Stage Renal Disease andCOBRA coverage After 30 months MedicareCOBRAIs covered under Workers’ Compensationbecause of a job-related illness or injury The patient is entitledto Medicare Workers’ Compensation(for health care items orservices related to jobrelated illness or injury)MedicareHas been in an accident or other situationwhere no-fault or liability insuranceis involved The patient is entitledto Medicare No-fault or liabilityinsurance for accident orother situation relatedhealth care servicesMedicareIs age 65 or older OR is disabled andcovered by Medicare and COBRA The patient is entitledto Medicare MedicareCOBRAAre There Any Exceptions to the MSP Requirements?In most cases, Federal law takes precedence over state laws and private contracts. Even if a state law orinsurance policy states that they are a secondary payer to Medicare, the MSP provisions should be followedwhen billing for services.2
What Happens if the PrimaryPayer Denies a Claim?collect accurate MSP beneficiary information forthe COBC to coordinate the information.In the following situations, Medicare may makepayment assuming the services are covered and aproper claim has been filed.To support the goals of the MSP provisions, theCOBC manages several data gathering programs.These programs were implemented in threephases, as discussed in the next section. The Group Health Plan (GHP) denies paymentfor services because the beneficiary is notcovered by the health plan; The no-fault or liability insurer does not pay, ordenies the medical bill; The Workers’ Compensation (WC) programdenies payment, as in situations where WCis not required to pay for a given medicalcondition; or The WC Medicare Set-aside Arrangement(WCMSA) is exhausted.In these situations, providers, physicians, andother suppliers should include documentationfrom the primary payer stating that the claim hasbeen denied and/or benefits have been exhaustedwhen submitting the claim to Medicare.When Will Medicare Make aConditional Payment?Medicare will make a conditional payment forMedicare covered services in liability, no-fault, andWC situations where another payer is responsiblefor payment and the claim is not expected to bepaid within the promptly period. Medicare makesconditional payments to prevent the beneficiaryfrom using his or her own money to pay the claim.However, Medicare has the right to recover anyconditional payments.How Is Beneficiary HealthInsurance or CoverageInformation Collectedand Coordinated?The Centers for Medicare & Medicaid Services(CMS) established the Coordination of BenefitsContractor (COBC) to collect, manage, andmaintain information on Medicare’s CommonWorking File (CWF) regarding other healthinsurance or coverage for Medicare beneficiaries.Providers, physicians, and other suppliers mustWhat Are Some of theActivities Managed bythe COBC?Activities that the COBC performs to collect MSPdata include: Initial Enrollment Questionnaire (IEQ) –The COBC sends out the IEQ approximatelythree months before an individual is eligiblefor Medicare. This questionnaire asks thebeneficiary if he or she has other healthinsurance or coverage (including prescriptiondrug coverage) that may be primaryto Medicare. Internal Revenue Service/Social SecurityAdministration/CMS (IRS/SSA/CMS) DataMatch Project Coordination – The OmnibusBudget Reconciliation Act of 1989 requires eachagency to share information it has regardingemployment of Medicare beneficiaries or theirspouses. This information helps determinewhether a beneficiary may be covered bya GHP that pays primary to Medicare. Thisinformation is sent to the COBC, whichcoordinates the Data Match Project. Data Match Project – The Voluntary DataSharing Agreement (VDSA) program allowsfor the electronic data exchange of GHPeligibility and Medicare information betweenCMS, employers, and prescription drug plans.Employers, to meet the mandatory reportingrequirements, can sign a VDSA in lieu ofcompleting and submitting the IRS/SSA/CMSData Match Questionnaire. CMS has alsodeveloped a new data exchange, similar tothe VDSA program, for Supplemental DrugPlans [Non-Qualified State PharmaceuticalAssistance Programs (SPAPs)] to coordinatewith Medicare Part D.3
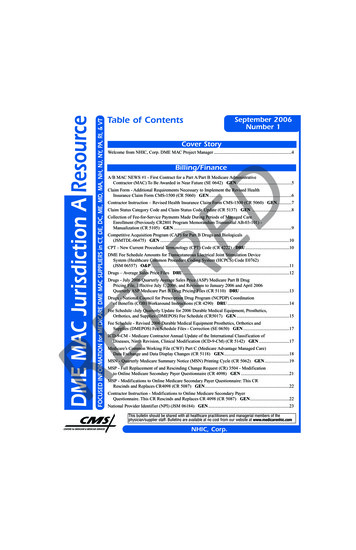
MSP Claims Investigation Process – The COBCis responsible for all initial MSP developmentactivities previously performed by Medicarecontractors1. The COBC provides a one-stopcustomer service approach for all MSP-relatedinquiries. However, the COBC does not processclaims, nor does it handle any mistakenpayment recoveries or claim-specific inquiries.Each provider, physician, or other suppliershould continue to call the Medicare contractorthat processes their claims regarding specificclaim-based issues. MSP Mandatory Reporting Process – Section111 of the Medicare, Medicaid, State Children’sHealth Insurance Program (SCHIP) ExtensionAct of 2007 (MMSEA) adds new mandatoryreporting requirements for GHP arrangementsand for liability insurance (including selfinsurance), no-fault insurance, and WC (NonGroup Health Plans). Responsible ReportingEntities (RREs) are now mandated to submitGHP and Non-Group Health Plan informationto strengthen the MSP coordination ofbenefits process.What Is Section 111 MSPMandatory Reporting?Section 111 of MMSEA adds to existing MSPprovisions of the Social Security Act to providefor mandatory reporting for GHP arrangements,liability insurance (including self-insurance),no-fault insurance, and WC. The provisions wereimplemented January 1, 2009, for informationabout GHP arrangements and July 1, 2009, forliability insurance (including self-insurance),no-fault insurance, and WC. The purpose of thereporting process is to enable CMS to correctly payfor the health insurance of Medicare beneficiariesby determining primary versus secondarypayer. Under the new Section 111 requirements,enrollment and settlement data will be submittedFor more information and official instructionsfor Section 111 MSP reporting, please visit theMandatory Insurer Reporting Web Page at http://www.cms.hhs.gov/MandatoryInsRep/ontheCMS website.What Is the Provider’s,Physician’s, or Other Supplier’sRole in the MSP Provisions?Providers, physicians, and other suppliers must aidin the collection and coordination of beneficiaryhealth insurance or coverage information by: Asking the patient or his/her representativequestions concerning the patient’s MSP status.A suggested method is to incorporate an MSPquestionnaire into all patient health records. Billing the primary payer before billingMedicare, as required by the SocialSecurity Act.How Do Providers, Physicians,and Other SuppliersGather Accurate Datafrom the Beneficiary?Providers, physicians, and other suppliers cansave time and money by collecting patient healthinsurance or coverage information at each patientvisit. Some suggested questions that providers,physicians, and other suppliers should ask include,but are not limited to: Is the patient covered by any GHP through hisor her current or former employment? If so,how many employees work for the employerproviding coverage?Medicare Contracting Reform (MCR) Update – In Section 911 of the Medicare Prescription Drug, Improvement, and ModernizationAct of 2003 (MMA) Congress mandated that the Secretary of the Department of Health and Human Services replace the currentcontracting authority under Title XVIII of the Social Security Act with the new Medicare Administrative Contractor (MAC) authority.This mandate is referred to as Medicare Contracting Reform. Medicare Contracting Reform is intended to improve Medicare’sadministrative services to beneficiaries and health care providers. All Medicare work performed by Fiscal Intermediaries and Carrierswill be replaced by the new A/B MACs by 2011. Providers may access the most current MCR information to determine the impactof these changes and to view the list of current MACs for each jurisdiction at n the CMS website.14electronically to the COBC. These requirements donot change or eliminate any existing obligationsunder the MSP statutory provisions or regulations.The new Section 111 requirements add reportingrules to the existing MSP requirements.
Is the patient covered by a GHP through his orher spouse or other family member’s currentor former employment? If so, how manyemployees work for the employer providingthe GHP? Is the patient receiving WC benefits? Does the patient have a WCMSA? Is the patient covered under no-fault insuranceor liability insurance? Is the patient being treated for an injuryor illness for which another party could beheld liable?Providers, physicians, and other suppliers mayalso use a model questionnaire published byCMS to collect patient information. This tool isavailable online in the MSP Manual in Chapter 3,Section 20.2.1 at .pdf on the CMS website.If the provider, physician, or other supplier doesnot furnish Medicare with a record of other healthinsurance or coverage that may be primary toMedicare on any claim and there is an indicationof possible MSP considerations, the COBC mayrequest that the provider, physician, or othersupplier complete a Development Questionnaire.Why Gather AdditionalBeneficiary Health Insuranceor Coverage Information?The goal of MSP information-gathering activitiesis to quickly identify possible MSP situations,thus ensuring correct primary and secondarypayments by the responsible parties. This effortmay require that providers, physicians, and othersuppliers complete Development Questionnairesto collect accurate beneficiary health insuranceor coverage information. Many of the questionson the Development Questionnaires are similarto the questions that providers, physicians, andother suppliers might ask a beneficiary during aroutine visit. This similarity provides another goodreason to routinely ask patients about their healthinsurance or coverage. If a provider, physician,or other supplier gathers information about abeneficiary’s other health insurance or coverageand uses that information to complete the claimproperly, a Development Questionnaire maynot be necessary. Accurate submittal of claimsmay accelerate the processing of the provider’s,physician’s, or other supplier’s claim.The COBC may submit a Secondary ClaimDevelopment (SCD) Questionnaire to providers,physicians, and other suppliers.What Is a SecondaryClaim Development(SCD) Questionnaire?An SCD Questionnaire may be sent to the provider,physician, or other supplier when a claim issubmitted with an Explanation of Benefits (EOB)attached from an insurer other than Medicare,and relevant information was not submitted toproperly adjudicate the submitted claim. TheCOBC provides the names and Health InsuranceClaim Number (HICN) of each individual for whichthe provider, physician, or other supplier mustcomplete an SCD Questionnaire. The provider,physician, or other supplier must complete andsubmit the SCD Questionnaire to the COBC.What Happens if the Provider,Physician, or Other SupplierSubmits a Claim to MedicareWithout Providing the OtherInsurer’s Information?The claim may be paid if it meets all Medicarerequirements, including Medicare coverageand medical necessity guidelines. However,5
if the beneficiary’s Medicare record indicatesthat another insurer should have paid primaryto Medicare, the claim will be either returnedunprocessed to the provider or denied orsuspended for development. If the Medicarecontractor has enough information, they mayforward the information to the COBC and the COBCmay send the provider, physician, or other suppliera SCD Questionnaire to complete for additionalinformation if they were the informant. Medicarewill review the information on the questionnaireand determine the proper action to take.Specific claim-based issues (including claimprocessing) should still be addressed to theprovider’s, physician’s, or other supplier’sMedicare claims processing contractor.What Happens if the Provider,Physician, or Other SupplierFails to File Correct andAccurate Claimswith Medicare? The Medicare Learning Network Home PageThe Medicare Learning Network (MLN) isthe brand name for official CMS educationalproducts and information for Medicarefee-for-service providers. For additionalinformation visit the Medicare LearningNetwork’s web page at http://www.cms.hhs.gov/MLNGenInfo on the CMS website.Where Can I Find MoreInformation on the Provider’s,Physician’s, or Other Supplier’sRole in MSP and COB?CMS offers several online references forinformation about MSP, COB, and theMedicare Program:Federal law permits Medicare to recover itsconditional payments. Providers, physicians, andother suppliers can be fined up to 2,000 forknowingly, willfully, and repeatedly providinginaccurate information relating to the existenceof other health insurance or coverage.How Does the Provider,Physician, or Other SupplierContact the COBC?Providers, physicians, and other suppliers maycontact the COBC at 1-800-999-1118 (TTY/TDD:1-800-318-8782), Monday - Friday, 8 a.m. to 8 p.m.Eastern Time (excluding holidays). Providers,physicians, and other suppliers may contact theCOBC to: Report potential MSP situations; Report incorrect insurance information; or Address general MSP questions/concerns. The Medicare Coordination of BenefitsHome he Medicare Coordination of Benefits HomePage features materials related to theMSP provisions. The Contacting the COBC Web 3ContactingtheCOBContractor.aspThe Contacting the COBC Web Page containsthe contact information and specificaddresses for submittingCOBC-requested materials.This fact sheet was current at the time it was published or uploaded onto the web. Medicare policy changes frequently so links tothe source documents have been provided within the document for your reference.This fact sheet was prepared as a tool to assist providers and is not intended to grant rights or impose obligations. Although everyreasonable effort has been made to assure the accuracy of the information within these pages, the ultimate responsibility for thecorrect submission of claims and response to any remittance advice lies with the provider of services. The Centers for Medicare& Medicaid Services (CMS) employees, agents, and staff make no representation, warranty, or guarantee that this compilationof Medicare information is error-free and will bear no responsibility or liability for the results or consequences of the use of thisguide. This publication is a general summary that explains certain aspects of the Medicare Program, but is not a legal document.The official Medicare Program provisions are contained in the relevant laws, regulations, and rulings.April 20096ICN# 006903
Medicare Secondary Payer. Fact Sheet. for Provider, Physician, and. Other Supplier Billing Staff Background. Maintaining the viability and integrity of the Medicare Trust Fund becomes critical as the Medicare Program matures and the "baby boomer" generation moves toward retirement. Providers, physicians, and other