Transcription
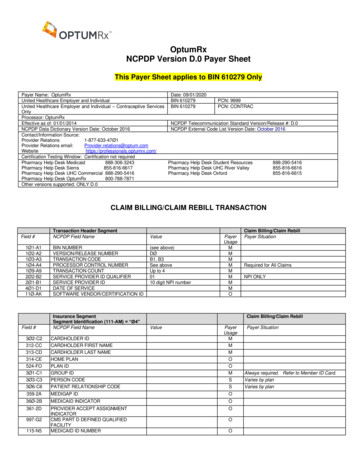
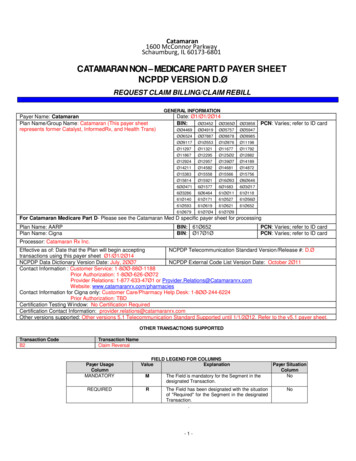
Catamaran1600 McConnor ParkwaySchaumburg, IL 60173-6801CATAMARAN NON – MEDICARE PART D PAYER SHEETNCPDP VERSION D.ØREQUEST CLAIM BILLING/CLAIM REBILLGENERAL INFORMATIONPayer Name: CatamaranPlan Name/Group Name: Catamaran (This payer sheetrepresents former Catalyst, InformedRx, and Health Trans)Date: Ø1/Ø1/2Ø14BIN:ØØ3452 61Ø67961Ø7Ø461Ø7Ø9PCN: Varies; refer to ID cardFor Catamaran Medicare Part D- Please see the Catamaran Med D specific payer sheet for processingPlan Name: AARPPlan Name: CignaBIN: 61Ø652BIN: Ø17Ø1ØPCN: Varies; refer to ID cardPCN: Varies; refer to ID cardProcessor: Catamaran Rx Inc.NCPDP Telecommunication Standard Version/Release #: D.ØEffective as of: Date that the Plan will begin acceptingtransactions using this payer sheet Ø1/Ø1/2Ø14NCPDP Data Dictionary Version Date: July, 2ØØ7NCPDP External Code List Version Date: October 2Ø11Contact Information : Customer Service: 1-8ØØ-88Ø-1188Prior Authorization: 1-8ØØ-626-ØØ72Provider Relations: 1-877-633-47Ø1 or Provider.Relations@Catamaranrx.comWebsite: www.catamaranrx.com/pharmaciesContact Information for Cigna only: Customer Care/Pharmacy Help Desk: 1-8ØØ-244-6224Prior Authorization: TBDCertification Testing Window: No Certification RequiredCertification Contact Information: provider.relations@catamaranrx.comOther versions supported: Other versions 5.1 Telecommunication Standard Supported until 1/1/2Ø12. Refer to the v5.1 payer sheet.OTHER TRANSACTIONS SUPPORTEDTransaction CodeB2Transaction NameClaim ReversalPayer UsageColumnMANDATORYREQUIREDFIELD LEGEND FOR COLUMNSValueExplanationMThe Field is mandatory for the Segment in thedesignated Transaction.RThe Field has been designated with the situationof "Required" for the Segment in the designatedTransaction.-1-Payer SituationColumnNoNo
Yes―Required when‖. The situations designated havequalifications for usage ("Required if x", "Notrequired if y").Fields that are not used in the Claim Billing transactions and those that do not have qualified requirements(i.e. not used) for this payer are excluded from the payer sheet.CLAIM BILLING/CLAIM REBILL TRANSACTIONThe following lists the segments and fields in a Claim Billing Transaction for the NCPDP Telecommunication Standard Implementation Guide vD.Ø.QUALIFIED REQUIREMENTTransaction Header SegmentRWCheckThis Segment is always sentSource of certification IDs required in SoftwareVendor/Certification ID (11Ø-AK) is Switch/VAN issuedXSource of certification IDs required in SoftwareVendor/Certification ID (11Ø-AK) is Not usedField 4Ø1-D111Ø-AKTransaction Header SegmentNCPDP Field NameBIN NUMBERVERSION/RELEASE NUMBERTRANSACTION CODEPROCESSOR CONTROL NUMBERTRANSACTION COUNTSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICESOFTWARE VENDOR/CERTIFICATIONIDInsurance SegmentThis Segment is always sentThis payer does support partial fillsField #115-N53Ø1-C1Insurance SegmentSegment Identification (111-AM) “Ø4”NCPDP Field NameClaim BillingXUse value for Switch‘s requirements. If submitting claim without aswitch, populate with blanks.XUse value for Switch‘s requirements. If submitting claim without aswitch, populate with blanks.ValueDØB1- Claim B3 - RebillØ1,Ø2,Ø3,Ø 4Payer UsageMMMMMØ1- NPI - National Provider IDCheckMMMMClaim BillingPayer SituationBIN listed in General InformationRequired from ID cardAccept up to 1 to 4 transactions pertransmission except for Multi-IngredientCompound claims which should be only1 transaction.Only value ‘Ø1‘ (NPI) accepted.NPI OF PHARMACY requiredYYYYMMDDUse value for Switch‘s requirements. Ifsubmitting claim without a switch, populatewith blanks.Claim Billing/Claim RebillXXClaim Billing/Claim RebillValuePayerUsageRWMEDICAID ID NUMBERGROUP IDMPayer SituationImp Guide: Required, if known, when patient hasMedicaid coverage.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if necessary forstate/federal/regulatory agency programs.Required if needed for pharmacy claimprocessing and payment.Payer Requirement: Required from ID card3Ø2-C2CARDHOLDER ID3Ø3-C3PERSON CODEMRWImp Guide: Required if needed to uniquelyidentify the family members within theCardholder ID.Payer Requirement: Refer to on-lineresponse for additional detail.-2-
3Ø6-C6PATIENT RELATIONSHIP CODEMImp Guide: Required if needed to uniquelyidentify the relationship of the Patient to theCardholder.Payer Requirement: Refer to on-lineresponse for additional detailInsurance SegmentSegment Identification (111-AM) “Ø4”3Ø9-C9Claim Billing/Claim RebillELIGIBILITY CLARIFICATION CODERWImp Guide: Required if needed for receiverinquiry validation and/or determination, wheneligibility is not maintained at the dependentlevel. Required in special situations as definedby the code to clarify the eligibility of anindividual, which may extend coverage.Payer Requirement: Refer to on-line responsefor additional detail312-CC313-CDCARDHOLDER FIRST NAMERWCARDHOLDER LAST NAMERWImp Guide: Required if necessary forPayer Requirement: Refer to on-line responsestate/federal/regulatory agency programs whenfor additional detailthe cardholder has a first name.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-line responsefor additional detail314-CE359-2A36Ø-2BHOME PLANRWMEDIGAP IDRWMEDICAID INDICATORRWImp Guide: Required if needed for receiverbilling/encounter validation and/or determinationfor Blue Cross or Blue Shield, if a Patient hascoverage under more than one plan, todistinguish each plan.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required, if known, whenpatient has Medigap coverage.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required, if known, when patient hasMedicaid coverage.Payer Requirement: Refer to on-line responsefor additional detail361-2DPROVIDER ACCEPT ASSIGNMENTINDICATORRWImp Guide: Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-line responsefor additional detail524-FOPLAN IDRWImp Guide: Optional.Payer Requirement: Refer to on-line responsefor additional detail.-3-
997-G2CMS PART D DEFINED QUALIFIEDFACILITYRWImp Guide: Required if specified in tradingpartner agreement.Payer Requirement: Refer to on-line responsefor additional detailPatient SegmentThis Segment is always sentField331-CX332-CYPatient SegmentSegment Identification (111-AM) “Ø1”NCPDP Field NameCheckClaim Billing/Claim RebillXClaim Billing/Claim RebillValuePayerUsageRWPATIENT ID QUALIFIERPATIENT IDRWPayer SituationImp Guide: Required if Patient ID (332-CY) isused.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if necessary forstate/federal/regulatory agency programs tovalidate dual eligibility.Payer Requirement: Refer to on-line responsefor additional detail3Ø4-C4DATE OF BIRTH3Ø5-C5PATIENT GENDER CODE31Ø-CAPATIENT FIRST NAMER311-CBPATIENT LAST NAMER322-CMPATIENT STREET ADDRESS323-CNRØ - Not Specified1 - Male2 - FemaleRPATIENT CITY ADDRESSRWImp Guide: Optional.RWPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Optional.Payer Requirement: Refer to on-line responsefor additional detail324-COPATIENT STATE/ PROVINCE ADDRESSRWImp Guide: Optional.Payer Requirement: Refer to on-line responsefor additional detail325-CPPATIENT ZIP/ POSTAL ZONERWImp Guide: Optional.Payer Requirement: Refer to on-line responsefor additional detail326-CQPATIENT PHONE NUMBERRWImp Guide: Optional.Payer Requirement: Refer to on-line responsefor additional detail.-4-
3Ø7-C7PLACE OF SERVICESee Appendix for acceptedvaluesRWImp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Required for Long TermCare ClaimsPatient SegmentSegment Identification (111-AM) “Ø1”333-CZClaim Billing/Claim RebillEMPLOYER IDRWImp Guide: Required if ―required by law‖ asdefined in the HIPAA final Privacy regulationssection 164.5Ø1 definitions (45 CFR Parts 16Øand 164 Standards for Privacy of IndividuallyIdentifiable Health Information; Final Rule Thursday, December 28, 2ØØØ, page 828Ø3and following, and Wednesday, August 14,2ØØ2, page 53267 and following.)335-2CPREGNANCY INDICATORRWPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if pregnancy could result indifferent coverage, pricing, or patient financialresponsibility.Required if needed for Workers‘ Compensationbilling. if ―required by law‖ as defined in theRequiredHIPAA final Privacy regulations section 164.5Ø1definitions (45 CFR Parts 16Ø and 164Standards for Privacy of IndividuallyIdentifiable Health Information; Final RuleThursday, December 28, 2ØØØ, page 828Ø3and following, and Wednesday, August 14,2ØØ2, page 53267 and following.)Payer Requirement: Refer to on-line responsefor additional detail35Ø-HN384-4XPATIENT EMAIL ADDRESSPATIENT RESIDENCERWSee Appendix for acceptedvaluesRWImp Guide: May be submitted for the receiver torelay patient health care communications via theInternet when provided by the patient.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-line responsefor additional detailClaim SegmentCheckThis Segment is always sentThis payer supports partial fillsClaim SegmentSegment Identification (111-AM) “Ø7”Claim Billing/Claim RebillRequired for Long Term Care ClaimsXXClaim Billing/Claim Rebill.-5-
Field #NCPDP Field Name455-EMPRESCRIPTION/SERVICE REFERENCENUMBER QUALIFIER4Ø2-D2436-E1PRESCRIPTION/SERVICE REFERENCENUMBERClaim SegmentSegment Identification (111-AM) “Ø7”PRODUCT/SERVICE ID QUALIFIER4Ø7-D7PRODUCT/SERVICE IDValuePayerUsageMØ1 Rx BillingPayer SituationImp Guide: For Transaction Code of ―B1‖, inthe Claim Segment, the Prescription/ServiceReference Number Qualifier (455-EM) is ―1‖(Rx Billing).MClaim Billing/Claim RebillØØ – If CompoundØ1 – Universal Product Code(UPC)Ø3 National Drug Code(NDC)MØ If Compound, otherwiseM11 digit NDC456-ENRWASSOCIATED PRESCRIPTION/SERVICEREFERENCE NUMBERImp Guide: Required if the ―completion‖transaction in a partial fill (Dispensing Status(343-HD) ―C‖ (Completed)).Required if the Dispensing Status (343-HD) ―P‖ (Partial Fill) and there are multipleoccurrences of partial fills for this prescription.457-EPRWASSOCIATED PRESCRIPTION/SERVICEDATEPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if the ―completion‖transaction in a partial fill (Dispensing Status(343-HD) ―C‖ (Completed)).Required if Associated Prescription/ServiceReference Number (456-EN) is used.Required if the Dispensing Status (343-HD) ―P‖ (Partial Fill) and there are multipleoccurrences of partial fills for this prescription.458-SERWPROCEDURE MODIFIER CODE COUNTPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if Procedure ModifierCode (459-ER) is used.Payer Requirement: Refer to on-line responsefor additional detail459-ERRWPROCEDURE MODIFIER CODEImp Guide: Required to define a further level ofspecificity if the Product/Service ID (4Ø7-D7)indicated a Procedure Code was submitted.Payer Requirement: Refer to on-line responsefor additional detail442-E7QUANITITY DISPENSEDR4Ø3-D3FILL NUMBER4Ø5-D5DAYS SUPPLY4Ø6-D6COMPOUND CODE4Ø8-D8DISPENSE AS WRITTEN(DAW)/PRODUCT SELECTION CODER414-DEDATE PRESCRIPTION WRITTENRØ New - Original1-99 Refill numberRR1 NOT A COMPOUND2 COMPOUND.-6-RRequired if this field could result in differentcoverage, pricing, or patient financialresponsibility.
415-DFNUMBER OF REFILLS AUTHORIZEDRWImp Guide: Required if necessary for planbenefit administration.Payer Requirement: Refer to on-line responsefor additional detailClaim SegmentSegment Identification (111-AM) “Ø7”419-DJ354-NXPRESCRIPTION ORIGIN CODEClaim Billing/Claim Rebill1 Written – Prescriptionobtained via paper.2 Telephone – Prescriptionobtained via oral instructions orinteractive voice response using aphone.3 Electronic – Prescriptionobtained via SCRIPT or HL7Standard transactions4 Facsimile – Prescriptionobtained via transmission using afax machine.MPayer Requirement: Refer to on-lineresponse for additional detailRWSUBMISSION CLARIFICATION CODECOUNTImp Guide: Required if necessary for planbenefit administration.Imp Guide: Required if SubmissionClarification Code (42Ø-DK) is used.Payer Requirement: Required whenSubmission Clarification Code value is used.42Ø-DKSUBMISSION CLARIFICATION CODE8 Process Compound ForApproved IngredientsRWImp Guide: Required if clarification is neededand value submitted is greater than zero (Ø).If the Date of Service (4Ø1-D1) contains thesubsequent payer coverage date, theSubmission Clarification Code (42Ø-DK) isrequired with value of ―19‖ (Split Billing –indicates the quantity dispensed is theremainder billed to a subsequent payer whenMedicare Part A expires. Used only in longterm care settings) for individual unit of usemedications.Payer Requirement: Refer to on-lineresponse for additional detail46Ø-ETQUANTITY PRESCRIBEDRWImp Guide: Required for all Medicare Part Dclaims for drugs dispensed as Schedule II. Maybe used by trading partner agreement forclaims for drugs dispensed as Schedule II only.Payer Requirement: Refer to on-line responsefor additional detail3Ø8-C8OTHER COVERAGE CODE1 No other Coverage2 Other coverage existspayment collected – Code used incoordination of benefitstransactions to convey that othercoverage is available, the payerhas been billed and paymentreceived3 Exists-Claim not Covered4 Exists-Payment not Collected8 Claim Billing for PatientFinancial Responsibility Only.-7-RWImp Guide: Required if needed by receiver, tocommunicate a summation of other coverageinformation that has been collected from otherpayers.Required for Coordination of Benefits.Payer Requirement: Required Only forCoordination of Benefits claim processing.
429-DTUNIT DOSE INDICATORRWImp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-line responsefor additional detailClaim SegmentSegment Identification (111-AM) “Ø7”453-EJClaim Billing/Claim RebillORIG PRESCRIBED PRODUCT/SERVICE IDQUALIFIERRWImp Guide: Required if Originally PrescribedProduct/Service Code (455-EA) is used.Payer Requirement: Refer to on-line responsefor additional detail445-EA446-EB6ØØ-28ORIGINIALLY PRESCRIBEDPRODUCT/SERVICE CODERWORIGINALLY PRESCRIBED QUANTITYRWUNIT OF MEASURERWImp Guide: Required if the receiver requestsassociation to a therapeutic, or a preferredproduct substitution, or when a DUR alert hasbeen resolved by changing medications, or analternative service than what was originallyprescribed.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if the receiver requestsreporting for quantity changes due to atherapeutic substitution that has occurred or apreferred product/service substitution that hasoccurred, or when a DUR alert has beenresolved by changing quantities.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if necessary forstate/federal/regulatory agency programs.Required if this field could result in differentcoverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-line responsefor additional detail418-DILEVEL OF SERVICERWI Imp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-line responsefor additional detail461-EUPRIOR AUTHORIZATION TYPE CODERW.-8-Imp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Required if this field could result in differentcoverage, pricing, or patient financialPayer Requirement: Refer to on-line responseresponsibility.for additional detail
462-EVSUBMIT PRIOR AUTHORIZATION NUMBERRWImp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-line responsefor additional detail463-EWINTERMEDIARY AUTHORIZATION TYPE IDRWClaim SegmentSegment Identification (111-AM) “Ø7”464-EXINTERMEDIARY AUTHORIZATION IDRWImp Guide: Required for overriding anauthorized intermediary system edit when thepharmacy participates with an intermediary.Payer Requirement: Refer to on-line responsefor additional detailClaim Billing/Claim RebillRequired if Intermediary Authorization ID (464EX)used.Required for overriding anImp isGuide:authorized intermediary system edit when thepharmacy participates with an intermediary.343-HDDISPENSING STATUSP Partial FillC Completion of Partial FillRWPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required for the partial fill or thecompletion fill of a prescription.Payer Requirement: Refer to on-line responsefor additional detail344-HFQUANTITY INTENDED TO BE DISPENSEDRWImp Guide: Required for the partial fill or thecompletion fill of a prescription.Payer Requirement: Payer Requirement: Referto on-line response for additional detail345-HGRWDAYS SUPPLY INTENDED TO BEDISPENSEDImp Guide: Required for the partial fill or thecompletion fill of a prescription.Payer Requirement: Refer to on-line responsefor additional detail357-NV391-MTRWDELAY REASON CODERWPATIENT ASSIGNMENT INDICATOR(DIRECT MEMBER REIMBURSEMENTINDICATOR)Imp Guide: Required when needed to specifythe reason that submission of the transactionhas been delayed.Payer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required when the claimsadjudicator does not assume the patientassigned his/her benefits to the provider orwhen the claims adjudicator supports apatient determination of whether he/shewants to assign or retain his/her benefits.Payer Requirement: Refer to on-lineresponse for additional detail995-E2RWROUTE OF ADMINISTRATIONImp Guide: Required if specified in tradingpartner agreement.Payer Requirement: Refer to on-lineresponse for additional detail.-9-
996-G1147-U7RWCOMPOUND TYPERWPHARMACY SERVICE TYPEImp Guide: Required if specified in tradingpartner agreement.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required when the submitter mustclarify the type of services being performed as acondition for proper reimbursement by thepayer.Payer Requirement: Refer to on-lineresponse for additional detailPricing SegmentThis Segment is always sentField #4Ø9-D9412-DC477-BE433-DXPricing SegmentSegment Identification (111-AM) “11”NCPDP Field NameCheckClaim Billing/Claim RebillXClaim Billing/Claim RebillValuePayerUsageMRWINGREDIENT COST SUBMITTEDDISPENSING FEE SUBMITTEDPROFESSIONAL SERVICE FEE SUBMITTEDPATIENT PAID AMOUNT SUBMITTEDPayer SituationImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.RWPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.RWPayer Requirement: For Vaccine BillingclaimsImp Guide: Required if this field could result indifferent coverage, pricing, or patient financialresponsibility.Payer Requirement: Refer to on-lineresponse for additional detail438-E3INCENTIVE AMOUNT SUBMITTEDRWImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.Payer Requirement: For Vaccine Billing claims478-H7479-H8OTHER AMOUNT CLAIMED SUBMITTEDCOUNTRWOTHER AMOUNT CLAIMED SUBMITTEDQUALIFIERRWImp Guide: Required if Other Amount ClaimedSubmitted Qualifier (479-H8) is used.Payer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required if Other Amount ClaimedSubmitted (48Ø-H9) is used.Payer Requirement: Refer to on-lineresponse for additional detail.- 10-
48Ø-H9OTHER AMOUNT CLAIMED SUBMITTEDRWImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.Payer Requirement: Refer to on-line responsefor additional detail481-HAFLAT SALES TAX AMOUNT SUBMITTEDRWImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.Payer Requirement: Refer to on-line responsefor additional detail482-GERWPERCENTAGE SALES TAX AMOUNTSUBMITTEDImp Guide: Required if its value has an effecton the Gross Amount Due (43Ø-DU)calculation.Payer Requirement: Refer to on-line responsefor additional detail483-HEPricing SegmentSegment Identification (111-AM) “11”PERCENTAGE SALES TAX RATESUBMITTEDClaim Billing/Claim RebillRWImp Guide: Required if Percentage Sales TaxAmount Submitted (482-GE) and PercentageSales Tax Basis Submitted (484-JE) are used.Required if this field could result in differentpricing.Required if needed to calculate PercentageSales Tax Amount Paid (559-AX).Payer Requirement: Refer to on-line responsefor additional detail484-JEPERCENTAGE SALES TAX BASISSUBMITTEDRWImp Guide: Required if Percentage Sales TaxAmount Submitted (482-GE) and PercentageSales Tax Rate Submitted (483-HE) are used.Required if this field could result in differentpricing.Required if needed to calculate PercentageSales Tax Amount Paid (559-AX).426-DQUSUAL AND CUSTOMARY CHARGER43Ø-DUGROSS AMOUNT DUER423-DNBASIS OF COST DETERMINATIONRImp Guide: Required if needed for receiverclaim/encounter adjudication.Payer Requirement: Refer to on-line responsefor additional detailPharmacy Provider SegmentThis Segment is situationalCheckXClaim Billing/Claim RebillThis segment may be required as determined by benefit design.Pharmacy Provider SegmentSegment Identification (111-AM) “Ø2”Claim Billing/Claim Rebill.- 11-
465-EYRProvider ID QualifierImp Guide: Required if Provider ID (444-E9) isused.Payer Requirement: Refer to on-line responsefor additional detail444-E9Provider IDRImp Guide: Required if necessary forstate/federal/regulatory agency programs.Required if necessary to identify the individualresponsible for dispensing of the prescription.Required if needed for reconciliation ofencounter-reported data or encounter reporting.Prescriber SegmentThis Segment is situationalField #466-EZPrescriber SegmentSegment Identification (111-AM) “Ø3”NCPDP Field NameCheckXClaim Billing/Claim RebillThis segment may be required as determined by benefit design.Claim Billing/Claim RebillValuePayerUsageMPRESCRIBER ID QUALIFIERPayer SituationImp Guide: Required if Prescriber ID (411-DB)is used.Payer Requirement: Refer to on-line responsefor additional detail411-DBPRESCRIBER IDMImp Guide: Required if this field could result indifferent coverage or patient financialresponsibility.Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-line responsefor additional detail427-DRPRESCRIBER LAST NAMEMImp Guide: Required when the Prescriber ID(411-DB) is not known.Required if needed for Prescriber ID (411-DB)validation/clarification.Payer Requirement: Refer to on-line responsefor additional detail.- 12-
498-PMPRESCRIBER PHONE NUMBERRWImp Guide: Required if needed for Workers‘Compensation.Required if needed to assist in identifying theprescriber.Required if needed for Prior Authorizationprocess.Payer Requirement: Refer to on-lineresponse for additional detail468-2EPRIMARY CARE PROVIDER ID QUALIFIERRWImp Guide: Required if Primary Care ProviderID (421-DL) is used.Payer Requirement: Refer to on-lineresponse for additional detail421-DLPRIMARY CARE PROVIDER IDRWImp Guide: Required if needed for receiverclaim/encounter determination, if known andavailable.Required if this field could result in differentcoverage or patient financial responsibility.Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-lineresponse for additional detailPrescriber SegmentSegment Identification (111-AM) “Ø3”47Ø-4EClaim Billing/Claim RebillPRIMARY CARE PROVIDER LAST NAMERWImp Guide: Required if this field is used as analternative for Primary Care Provider ID (421DL) when ID is not known.Required if needed for Primary Care ProviderID (421-DL) validation/clarification.Payer Requirement: Refer to on-lineresponse for additional detail364-2JPRESCRIBER FIRST NAMERWImp Guide: Required if needed to assist inidentifying the prescriber.Required if necessary forstate/federal/regulatory agency programs.365-2KPRESCRIBER STREET ADDRESSRWPayer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required if needed to assist inidentifying the prescriber.Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-lineresponse for additional detail.- 13-
366-2MPRESCRIBER CITY ADDRESSRWImp Guide: Required if needed to assist inidentifying the prescriber.Required if necessary forstate/federal/regulatory agency programs.367-2NPRESCRIBER STATE/PROVINCEADDRESSRWPayer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required if needed to assist inidentifying the prescriber.Required if necessary forstate/federal/regulatory agency programs.368-2PPRESCRIBER ZIP/POSTAL ZONERWPayer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required if needed to assist inidentifying the prescriber.Required if necessary forstate/federal/regulatory agency programs.Payer Requirement: Refer to on-lineresponse for additional detail.- 14-
Coordination of Benefits/Other Payments SegmentCheckThis Segment is situationalXClaim BillingRequired only for secondary, tertiary, etc claims.Rather than provide separate payer sheets that are very repetitive, we have opted to indicate here the 2 types of COB methods for billing that aresupported by the plans in the General Information section.Scenario 1 - Other Payer Amount Paid Repetitions OnlyXScenario 2 - Other Payer-Patient Responsibility AmountRepetitions and Benefit Stage Repetitions OnlyXScenario 1 - Other Payer Amount Paid Repetitions OnlyCoordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”Field #337-4C338-5CNCPDP Field NameCOORDINATION OF BENEFITS/OTHERPAYMENTS COUNTOTHER PAYER COVERAGE TYPEClaim Billing/Claim RebillValueMaximum count of 9.PayerUsageMBlank Not SpecifiedMScenario 1 - Other Payer Amount PaidRepetitions OnlyPayer SituationØ1 Primary – FirstØ2 Secondary – SecondØ3 Tertiary – ThirdØ4 Quaternary – FourthØ5 Quinary – FifthØ6 Senary – SixthØ7 Septenary – SeventhØ8 Octonary – EighthØ9 Nonary – Ninth339-6C34Ø-7COTHER PAYER ID QUALIFIERRWOTHER PAYER IDRWImp Guide: Required if Other Payer ID (34Ø7C) is used.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if identification of theOther Payer is necessary for claim/encounteradjudication.Payer Requirement: Refer to on-line responsefor additional detail443-E8341-HB342-HCOTHER PAYER DATEOTHER PAYER AMOUNT PAID COUNTRWMaximum count of 9.OTHER PAYER AMOUNT PAID QUALIFIERRWRWImp Guide: Required if identification of theOther Payer Date is necessary forclaim/encounter adjudication.Payer Requirement: Refer to on-lineresponse for additional detailImp Guide: Required if Other Payer AmountPaid Qualifier (342-HC) is used.Payer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if Other Payer AmountPaid (431-DV) is used.Payer Requirement: Refer to on-line responsefor additional detail.- 14 -
Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”431-DVClaim Billing/Claim RebillScenario 1 - Other Payer Amount PaidRepetitions OnlyOTHER PAYER AMOUNT PAIDRWImp Guide: Required if other payer hasapproved payment for some/all of the billing.Not used for patient financial responsibility onlybilling.Not used for non-governmental agencyprograms if Other Payer-Patient ResponsibilityAmount (352-NQ) is submitted.471-5EOTHER PAYER REJECT COUNTRWPayer Requirement: Refer to on-line responsefor additional detailImp Guide: Required if Other Payer RejectCode (472-6E) is used.Payer Requirement: Refer to on-lineresponse for additional detail472-6EOTHER PAYER REJECT CODERWImp Guide: Required when the other payer hasdenied the payment for the billing.Payer Requirement: Refer to on-lineresponse for additional detailScenario 2 - Other Payer-Patient Responsibility Amount Repetitions and Benefit Stage Repetitions OnlyCoordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”Field #337-4C338-5CNCPDP Field NameCOORDINATION OF BENEFITS/OTHERPAYMENTS COUNTOTHER PAYER COVERAGE TYPEClaim Billing/Claim RebillScenario 2 - Other Payer – PatientResponsibility Amount Repetitions andBenefit Stage Repetitions OnlyValueMaximum count of 9.PayerUsageMBlank Not SpecifiedMPayer SituationØ1 Primary – FirstØ2 Secondary – SecondØ3 Tertiary – ThirdØ4 Quaternary – FourthØ5 Quinary – FifthØ6 Senary – SixthØ7 Septenary – SeventhØ8 Octonary – EighthØ9 Nonary – Ninth339-6COTHER PAYER ID QUALIFIERRWImp Guide: Required if Other Payer ID (34Ø7C) is used.Payer Requirement: Refer to on-line responsefor additional detail34Ø-7COTHER PAYER IDRWImp Guide: Required if identification of theOther Payer is necessary for claim/encounteradjudication.Payer Requirement: Refer to on-line responsefor additional detail.- 15 -
Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”443-E8Claim Billing/Claim RebillScenario 2 - Other Payer – PatientResponsibility Amount Repetitions andBenefit Stage Repetitions OnlyOTHER PAYER DATERWImp Guide: Required if identification of theOther Payer Date is necessary forclaim/encounter adjudication.Payer
For Catamaran Medicare Part D- Please see the Catamaran Med D specific payer sheet for processing . Customer Care/Pharmacy Help Desk: 1-8ØØ-244-6224 Prior Authorization: TBD Certification Testing Window: No Certification Required . 326-CQ PATIENT PHONE NUMBER RW Imp Guide: Optional. Payer Requirement: Refer to on-line response for .