Transcription
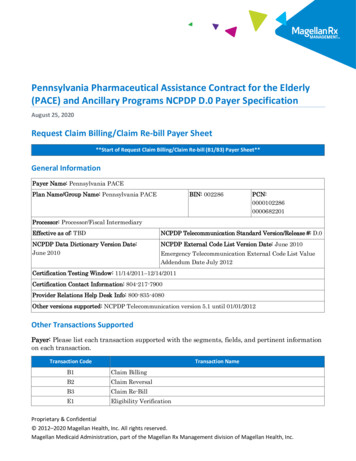
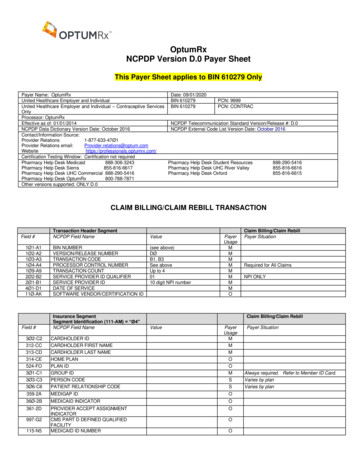
OptumRxNCPDP Version D.0 Payer SheetThis Payer Sheet applies to BIN 610279 OnlyPayer Name: OptumRxDate: 09/01/2020United Healthcare Employer and IndividualBIN 610279PCN: 9999United Healthcare Employer and Individual – Contraceptive Services BIN 610279PCN: CONTRACOnlyProcessor: OptumRxEffective as of: 01/01/2014NCPDP Telecommunication Standard Version/Release #: D.0NCPDP Data Dictionary Version Date: October 2016NCPDP External Code List Version Date: October 2016Contact/Information Source:Provider Relations1-877-633-47Ø1Provider Relations rofessionals.optumrx.com/Certification Testing Window: Certification not requiredPharmacy Help Desk Medicaid888-306-3243Pharmacy Help Desk Student Resources888-290-5416Pharmacy Help Desk Sierra855-816-6617Pharmacy Help Desk UHC River Valley855-816-6616Pharmacy Help Desk UHC Commercial 888-290-5416Pharmacy Help Desk Oxford855-816-6615Pharmacy Help Desk OptumRx800-788-7871Other versions supported: ONLY D.0CLAIM BILLING/CLAIM REBILL TRANSACTIONField 4Ø1-D111Ø-AKField #Transaction Header SegmentNCPDP Field NameBIN NUMBERVERSION/RELEASE NUMBERTRANSACTION CODEPROCESSOR CONTROL NUMBERTRANSACTION COUNTSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICESOFTWARE VENDOR/CERTIFICATION IDInsurance SegmentSegment Identification (111-AM) “Ø4”NCPDP Field NameValue(see above)DØB1, B3See aboveUp to 40110 digit NPI RDHOLDER IDCARDHOLDER FIRST NAMECARDHOLDER LAST NAMEHOME PLANPLAN IDGROUP IDPERSON CODEPATIENT RELATIONSHIP CODE359-2AMEDIGAP IDO36Ø-2BMEDICAID INDICATORO361-2DPROVIDER ACCEPT ASSIGNMENTINDICATORCMS PART D DEFINED QUALIFIEDFACILITYMEDICAID ID NUMBERO115-N5Required for All ClaimsNPI ONLYClaim Billing/Claim 33Ø6-C6997-G2Claim Billing/Claim RebillPayer SituationOOPayer SituationAlways required. Refer to Member ID Card.Varies by planVaries by plan
323-CN324-CO325-CP326-CQ3Ø7-C7333-CZ384-4XField 6-D64Ø8-D8414-DE415-DF419-DJ354-NXPatient SegmentSegment Identification (111-AM) “Ø1”NCPDP Field NameClaim SegmentSegment Identification (111-AM) “Ø7”NCPDP Field Name3Ø8-C8OTHER COVERAGE CODE446-EB418-DI461-EU462-EV995-E2ORIGINALLY PRESCRIBEDPRODUCT/SERVICE ID QUALIFIERORIGINALLY PRESCRIBEDPRODUCT/SERVICE CODEORIGINALLY PRESCRIBED QUANTITYLEVEL OF SERVICEPRIOR AUTHORIZATION TYPE CODEPRIOR AUTHORIZATION NUMBERSUBMITTEDROUTE OF ADMINISTRATIONPayerUsageOORRRROOOOOSOOPayer SituationClaim Billing/Claim RebillValuePRESCRIPTION/SERVICE REFERENCEØ1 Rx BillingNUMBER QUALIFIERPRESCRIPTION/SERVICE REFERENCENUMBERPRODUCT/SERVICE ID QUALIFIERPRODUCT/SERVICE IDQUANTITY DISPENSEDFILL NUMBERDAYS SUPPLYCOMPOUND CODEDISPENSE AS WRITTEN (DAW)/PRODUCTSELECTION CODEDATE PRESCRIPTION WRITTENNUMBER OF REFILLS AUTHORIZEDPRESCRIPTION ORIGIN CODESUBMISSION CLARIFICATION CODEMaximum count of 3.COUNTSUBMISSION CLARIFICATION CODEQUANTITY PRESCRIBED445-EAValuePATIENT ID QUALIFIERPATIENT IDDATE OF BIRTHPATIENT GENDER CODEPATIENT FIRST NAMEPATIENT LAST NAMEPATIENT STREET ADDRESSPATIENT CITY ADDRESSPATIENT STATE / PROVINCE ADDRESSPATIENT ZIP/POSTAL ZONEPATIENT PHONE NUMBERPLACE OF SERVICEEMPLOYER IDPATIENT RESIDENCE42Ø-DK46Ø-ET453-EJClaim Billing/Claim RebillPayerUsageMMMMRRRRRRORWOORW00020308Payer SituationVaries by planRequired if Submission Clarification Code(42Ø-DK) is used.Effective 09/21/2020Required when claim is for Schedule II drugsor when a compound contains a Schedule IIdrug.RWRequired for Coordination of Benefits.OVaries by planRequired if Originally PrescribedProduct/Service Code (455-EA) is used.OOORWRWOVaries by planVaries by plan
Field #Claim SegmentSegment Identification (111-AM) “Ø7”NCPDP Field Name996-G1COMPOUND TYPE147-U7PHARMACY SERVICE TYPEField #Prescriber SegmentSegment Identification (111-AM) “Ø3”NCPDP Field SCRIBER ID QUALIFIERPRESCRIBER IDPRESCRIBER LAST NAMEPRESCRIBER PHONE NUMBERPRIMARY CARE PROVIDER ID QUALIFIERPRIMARY CARE PROVIDER IDPRIMARY CARE PROVIDER LAST NAMEClaim Billing/Claim RebillValuePayerUsageOOClaim Billing/Claim RebillValuePayerUsageMMOOOOO364-2JPRESCRIBER FIRST NAMEO365-2KPRESCRIBER STREET ADDRESSO366-2MPRESCRIBER CITY ADDRESSO367-2NPRESCRIBER STATE/PROVINCEADDRESSPRESCRIBER ZIP/POSTAL ZONEO368-2PPayer SituationPayer SituationNPI should be submitted whenever possibleOFor BIN 610297 we will select one of the following COB options:Scenario 1 - Other Payer Amount Paid Repetitions Only.Scenario 2 – Other Payer -Patient Responsibility Amount RepetitionsField #337-4CCoordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”NCPDP Field Name338-5C339-6CCOORDINATION OF BENEFITS/OTHERPAYMENTS COUNTOTHER PAYER COVERAGE TYPEOTHER PAYER ID QUALIFIER34Ø-7C443-E8341-HBOTHER PAYER IDOTHER PAYER DATEOTHER PAYER AMOUNT PAID COUNT342-HCOTHER PAYER AMOUNT PAID QUALIFIER431-DVOTHER PAYER AMOUNT PAID471-5EOTHER PAYER REJECT COUNT472-6EOTHER PAYER REJECT CODEField #Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”NCPDP Field NameValueMaximum count of 9.PayerUsageRMRMRMaximum count of 9.RRRWRWMMaximum count of 5.ValueClaim Billing/Claim RebillScenario 1 - Other Payer Amount PaidRepetitions OnlySituationalRequired if Other Payer ID (34Ø-7C) is used.Other payer BINRequired if Other Payer Amount Paid Qualifier(342-HC) is used.Required if Other Payer Amount Paid (431DV) is used.Required if other payer has approved paymentfor some/all of the billing.RWRequired if Other Payer Reject Code (472-6E)is used.RWRequired when the other payer has denied thepayment for the billing, designated with OtherCoverage Code (3Ø8-C8) 3 (Other CoverageBilled – claim not covered).PayerUsageClaim Billing/Claim RebillScenario 2- Other Payer-PatientResponsibility Amount RepetitionsPayer Situation
Field #337-4CCoordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”NCPDP Field Name338-5C339-6CCOORDINATION OF BENEFITS/OTHERPAYMENTS COUNTOTHER PAYER COVERAGE TYPEOTHER PAYER ID QUALIFIER34Ø-7C443-E8OTHER PAYER IDOTHER PAYER DATE353-NROTHER PAYER-PATIENTRESPONSIBILITY AMOUNT COUNT351-NPOTHER PAYER-PATIENTRESPONSIBILITY AMOUNT QUALIFIEROTHER PAYER-PATIENTRESPONSIBILITY AMOUNT352-NQValueMaximum count of 9.PayerUsageMMRWRWRMaximum count of 25.RWRWRWClaim Billing/Claim RebillScenario 2- Other Payer-PatientResponsibility Amount RepetitionsPayer SituationImp Guide: Required if Other Payer ID (34Ø7C) is used.Other Payer BINImp Guide: Required if identification of theOther Payer Date is necessary forclaim/encounter adjudication.Imp Guide: Required if Other Payer-PatientResponsibility Amount Qualifier (351-NP) isused.Imp Guide: Required if Other Payer-PatientResponsibility Amount (352-NQ) is used.Imp Guide: Required if necessary for patientfinancial responsibility only billing.Not used if Other Payer Amount Paid (431-DV)is submitted along with other coverage code 02or 03.Field E483-HE484-JE426-DQ43Ø-DU423-DNField #Pricing SegmentSegment Identification (111-AM) “11”NCPDP Field NameINGREDIENT COST SUBMITTEDDISPENSING FEE SUBMITTEDINCENTIVE AMOUNT SUBMITTEDOTHER AMOUNT CLAIMED SUBMITTEDCOUNTOTHER AMOUNT CLAIMED SUBMITTEDQUALIFIEROTHER AMOUNT CLAIMED SUBMITTEDFLAT SALES TAX AMOUNT SUBMITTEDPERCENTAGE SALES TAX AMOUNTSUBMITTEDPERCENTAGE SALES TAX RATESUBMITTEDPERCENTAGE SALES TAX BASISSUBMITTEDUSUAL AND CUSTOMARY CHARGEGROSS AMOUNT DUEBASIS OF COST DETERMINATIONDUR/PPS SegmentSegment Identification (111-AM) “Ø8”NCPDP Field NameClaim Billing/Claim RebillValueMaximum count of 3.SSMMRClaim Billing/Claim RebillValueMaximum of 9 occurrences.439-E4REASON FOR SERVICE CODEDDHD441-E6RESULT OF SERVICE CODERequired if Other Amount Claimed SubmittedQualifier (479-H8) is used.Required if Other Amount Claimed Submitted(48Ø-H9) is used.SDUR/PPS CODE COUNTERPROFESSIONAL SERVICE CODEThis segment is always RWRWRWPayer SituationImp Guide: Required if DUR/PPS Segment isused.Imp Guide: Required for drug utilization reviewoutcome.Required when overriding Drug-DrugInteractions and High Dose RejectsFOR BIN 610279ONLYImp Guide: Required for drug utilization reviewoutcome.Required when overriding Drug-DrugInteractions and High Dose RejectsFOR BIN 610279ONLYImp Guide: Required for drug utilization reviewoutcome.
Field #DUR/PPS SegmentSegment Identification (111-AM) “Ø8”NCPDP Field NameClaim Billing/Claim RebillValuePayerUsagePayer SituationRequired when overriding Drug-DrugInteractions and High Dose RejectsFOR BIN 610279ONLYField nd SegmentSegment Identification (111-AM) “1Ø”NCPDP Field NameCOMPOUND DOSAGE FORMDESCRIPTION CODECOMPOUND DISPENSING UNIT FORMINDICATORCOMPOUND INGREDIENT COMPONENTCOUNTCOMPOUND PRODUCT ID QUALIFIERCOMPOUND PRODUCT IDCOMPOUND INGREDIENT QUANTITYCOMPOUND INGREDIENT DRUG COST49Ø-UECOMPOUND INGREDIENT BASIS OF COSTDETERMINATION362-2GCOMPOUND INGREDIENT MODIFIERCODE COUNTCOMPOUND INGREDIENT MODIFIERCODE363-2HField #Clinical SegmentSegment Identification (111-AM) “13”NCPDP Field NameOptional SegmentRequired for CompoundsValueClaim Billing/Claim RebillPayerUsageRWPayer SituationRequired when compound is beingsubmitted.RWMaximum 25 ingredientsRWRWRWRWRWRWMaximum count of 1Ø.ORequired if needed for receiver claimdetermination when multiple products arebilled.Imp Guide: Required if needed for receiverclaim determination when multiple products arebilled.Imp Guide: Required when CompoundIngredient Modifier Code (363-2H) is sent.OClaim Billing/Claim RebillValueMaximum count of 5.PayerUsageO491-VEDIAGNOSIS CODE COUNT492-WEDIAGNOSIS CODE QUALIFIERO424-DODIAGNOSIS CODEOPayer SituationImp Guide: Required if Diagnosis Code Qualifier(492-WE) and Diagnosis Code (424-DO) areused.Imp Guide: Required if Diagnosis Code (424DO) is used.
CLAIM BILLING/CLAIM REBILL PAID (OR DUPLICATE OF PAID) RESPONSEResponse Transaction Header SegmentField Field #5Ø4-F4Field #NCPDP Field NameValueVERSION/RELEASE NUMBERTRANSACTION CODETRANSACTION COUNTHEADER RESPONSE STATUSSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICEDØB1, B3Same value as in requestA AcceptedSame value as in requestSame value as in requestSame value as in requestResponse Message SegmentSegment Identification (111-AM) “2Ø”NCPDP Field NameMESSAGEResponse Insurance SegmentSegment Identification (111-AM) “25”NCPDP Field Name3Ø1-C1524-FOGROUP IDPLAN ID3Ø2-C2CARDHOLDER IDField #31Ø-CA311-CB3Ø4-C4Field #Response Patient SegmentSegment Identification (111-AM) “29”NCPDP Field NameResponse Status SegmentSegment Identification (111-AM) “21”NCPDP Field NameTRANSACTION RESPONSE STATUS5Ø3-F3547-5F548-6F13Ø-UFAUTHORIZATION NUMBERAPPROVED MESSAGE CODE COUNTAPPROVED MESSAGE CODEADDITIONAL MESSAGE INFORMATIONCOUNTADDITIONAL MESSAGE INFORMATIONQUALIFIERADDITIONAL MESSAGE INFORMATIONADDITIONAL MESSAGE INFORMATIONCONTINUITY526-FQ131-UGField eClaim Billing/Claim Rebill – Accepted/Paid(or Duplicate of Paid)Payer SituationImp Guide: Required if text is needed forclarification or detail.Claim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationPart-DCommercialImp Guide: Required if the identification to beused in future transactions is different thanwhat was submitted on the request.Claim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationPATIENT FIRST NAMEPATIENT LAST NAMEDATE OF BIRTH112-AN132-UHValuePayerUsageMMMMMMMClaim Billing/Claim Rebill – Accepted/Paid(or Duplicate of Paid)Payer SituationResponse Claim SegmentSegment Identification (111-AM) “22”NCPDP Field NamePRESCRIPTION/SERVICE REFERENCENUMBER QUALIFIERValueP PaidD Duplicate of PaidMaximum count of 5.PayerUsageMClaim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationRSSMaximum count of 25.Value1 RxBillingPayerUsageMClaim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationImp Guide: For Transaction Code of “B1”, inthe Response Claim Segment, thePrescription/Service Reference NumberQualifier (455-EM) is “1” (Rx Billing).
Field #4Ø2-D2551-9F552-AP553-AR554-AS555-AT556-AUField #5Ø5-F55Ø6-F65Ø7-F7558-AW559-AXResponse Claim SegmentSegment Identification (111-AM) “22”NCPDP Field NamePRESCRIPTION/SERVICE REFERENCENUMBERPREFERRED PRODUCT COUNTPREFERRED PRODUCT ID QUALIFIERPREFERRED PRODUCT IDPREFERRED PRODUCT INCENTIVEPREFERRED PRODUCT COST SHAREINCENTIVEPREFERRED PRODUCT DESCRIPTIONResponse Pricing SegmentSegment Identification (111-AM) “23”NCPDP Field NameValueMaximum count of 6.ValuePayerUsageMSSSSSFuture capabilitiesFuture capabilitiesFuture capabilitiesFuture capabilitiesFuture capabilitiesSFuture capabilitiesPayerUsageRRRSS56Ø-AYPATIENT PAY AMOUNTINGREDIENT COST PAIDDISPENSING FEE PAIDFLAT SALES TAX AMOUNT PAIDPERCENTAGE SALES TAX AMOUNTPAIDPERCENTAGE SALES TAX RATE PAID561-AZPERCENTAGE SALES TAX BASIS PAID521-FLINCENTIVE AMOUNT PAID563-J2OTHER AMOUNT PAID COUNT564-J3OTHER AMOUNT PAID QUALIFIERS565-J4OTHER AMOUNT PAIDS566-J5OTHER PAYER AMOUNT RECOGNIZEDS5Ø9-F9522-FMTOTAL AMOUNT PAIDBASIS OF REIMBURSEMENTDETERMINATIONAMOUNT ATTRIBUTED TO SALES TAXRSACCUMULATED DEDUCTIBLE AMOUNTREMAINING DEDUCTIBLE AMOUNTREMAINING BENEFIT AMOUNTAMOUNT APPLIED TO PERIODICDEDUCTIBLEAMOUNT OF COPAYAMOUNT EXCEEDING PERIODICBENEFIT MAXIMUMAMOUNT OF COINSURANCEESTIMATED GENERIC SAVINGSSPENDING ACCOUNT AMOUNTREMAININGAMOUNT ATTRIBUTED TO PROVIDERNETWORK SELECTIONAMOUNT ATTRIBUTED TO PRODUCTSELECTION/BRAND DRUGAMOUNT ATTRIBUTED TO PRODUCTSELECTION/NON-PREFERREDFORMULARY m count of 3.Claim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationSSSSSSSSSSClaim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationImp Guide: Required if Percentage SalesTax Amount Paid (559-AX) is greater thanzero (Ø).Imp Guide: Required if Percentage SalesTax Amount Paid (559-AX) is greater thanzero (Ø).Required if Incentive Amount Submitted(438-E3) is greater than zero (Ø).Imp Guide: Required if Other Amount Paid(565-J4) is used.Imp Guide: Required if Other Amount Paid(565-J4) is used.Required if Other Amount ClaimedSubmitted (48Ø-H9) is greater than zero (Ø).Required if Other Payer Amount Paid (431DV) is greater than zero (Ø) andCoordination of Benefits/Other PaymentsSegment is supported.Required if Basis of Cost Determination(432-DN) is submitted on billing.Imp Guide: Required if Patient Pay Amount(5Ø5-F5) includes sales tax that is thefinancial responsibility of the member but isnot also included in any of the other fieldsthat add up to Patient Pay Amount.
Field #136-UNResponse Pricing SegmentSegment Identification (111-AM) “23”NCPDP Field NameValueAMOUNT ATTRIBUTED TO PRODUCTSELECTION/BRAND NON-PREFERREDFORMULARY SELECTIONResponse DUR/PPS SegmentSegment Identification (111-AM) “24”Situation SegmentNCPDP Field NameValue567-J6DUR/PPS RESPONSE CODE COUNTERMaximum 9 FV532-FW533-FX544-FY57Ø-NSREASON FOR SERVICE CODECLINICAL SIGNIFICANCE CODEOTHER PHARMACY INDICATORPREVIOUS DATE OF FILLQUANTITY OF PREVIOUS FILLDATABASE INDICATOROTHER PRESCRIBER INDICATORDUR FREE TEXT MESSAGEDUR ADDITIONAL TEXTField #PayerUsageSClaim Billing/Claim Rebill –Accepted/Paid (or Duplicate of Paid)Payer SituationClaim Billing/Claim Rebill – Accepted/Paid(or Duplicate of Paid)PayerUsageSSSSSSSSSSPayer Situation
CLAIM BILLING/CLAIM REBILL REJECTED/REJECTED RESPONSECLAIM BILLING/CLAIM REBILL REJECTED/REJECTED RESPONSEResponse Transaction Header SegmentField Field #5Ø4-F4Field FQ131-UGNCPDP Field NameValueVERSION/RELEASE NUMBERTRANSACTION CODETRANSACTION COUNTHEADER RESPONSE STATUSSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICEDØB1, B3Same value as in requestR RejectedSame value as in requestSame value as in requestSame value as in requestResponse Message SegmentSegment Identification (111-AM) “2Ø”Situation SegmentNCPDP Field NameValueMESSAGEResponse Status SegmentSegment Identification (111-AM) “21”NCPDP Field NameTRANSACTION RESPONSE STATUSAUTHORIZATION NUMBERREJECT COUNTREJECT CODEREJECT FIELD OCCURRENCEINDICATORADDITIONAL MESSAGE INFORMATIONCOUNTADDITIONAL MESSAGE INFORMATIONQUALIFIERADDITIONAL MESSAGE INFORMATIONADDITIONAL MESSAGE INFORMATIONCONTINUITYValueR RejectMaximum count of 5.Maximum count of 25.PayerUsageMMMMMMMClaim Billing/Claim RebillRejected/RejectedPayer SituationClaim Billing/Claim yer SituationClaim Billing/Claim RebillRejected/RejectedPayer Situation
CLAIM REVERSAL TRANSACTIONThe following lists the segments and fields in a Claim Reversal Transaction for the NCPDP Telecommunication StandardImplementation Guide Version D.Ø.Field 4Ø1-D111Ø-AKField #3Ø2-C23Ø1-C1Field #455-EM4Ø2-D2436-E14Ø7-D74Ø3-D33Ø8-C8Field #337-4C338-5CField #473-7E439-E444Ø-E5441-E6474-8ETransaction Header SegmentNCPDP Field NameBIN NUMBERVERSION/RELEASE NUMBERTRANSACTION CODEPROCESSOR CONTROL NUMBERTRANSACTION COUNTSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICESOFTWARE VENDOR/CERTIFICATION IDInsurance SegmentSegment Identification (111-AM) “Ø4”NCPDP Field NameValueSee B1 informationDØB2See B1 information1NPI01BlanksPRESCRIPTION/SERVICE REFERENCENUMBER QUALIFIERPRESCRIPTION/SERVICE REFERENCENUMBERPRODUCT/SERVICE ID QUALIFIERPRODUCT/SERVICE IDFILL NUMBEROTHER COVERAGE CODECoordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) “Ø5”NCPDP Field NameCOORDINATION OF BENEFITS/OTHERPAYMENTS COUNTOTHER PAYER COVERAGE TYPEDUR/PPS SegmentSegment Identification (111-AM) “Ø8”NCPDP Field NameDUR/PPS CODE COUNTERREASON FOR SERVICE CODEPROFESSIONAL SERVICE CODERESULT OF SERVICE CODEDUR/PPS LEVEL OF EFFORTClaim ReversalPayer SituationClaim ReversalValueCARDHOLDER IDGROUP IDClaim SegmentSegment Identification (111-AM) “Ø7”NCPDP Field NamePayerUsageMMMMMMMMMPayerUsageMSPayer SituationClaim ReversalValue1PayerUsageMPayer SituationMMMMMSituational SegmentValueMaximum count of 9.Claim ReversalPayerUsageMPayer SituationMSituational SegmentValueMaximum of 9 occurrences.Claim ReversalPayerUsagePayer Situation
CLAIM REVERSAL ACCEPTED/APPROVED RESPONSEField Field #5Ø4-F4Field #112-AN5Ø3-F3Field #Response Transaction Header SegmentNCPDP Field NameValueVERSION/RELEASE NUMBERTRANSACTION CODETRANSACTION COUNTHEADER RESPONSE STATUSSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICEDØB2Same value as in requestA AcceptedSame value as in requestSame value as in requestSame value as in requestResponse Message SegmentSegment Identification (111-AM) “2Ø”NCPDP Field NameTRANSACTION RESPONSE STATUSAUTHORIZATION NUMBERResponse Claim SegmentSegment Identification (111-AM) “22”NCPDP Field Name455-EMPRESCRIPTION/SERVICE REFERENCENUMBER QUALIFIER4Ø2-D2PRESCRIPTION/SERVICE REFERENCENUMBERClaim Reversal – Accepted/ApprovedPayer SituationClaim Reversal – Accepted/ApprovedValueMESSAGEResponse Status SegmentSegment Identification (111-AM) “21”NCPDP Field NamePayerUsageMMMMMMMPayerUsageRPayer SituationReversal AcceptedClaim Reversal – Accepted/ApprovedValueA ApprovedPayerUsageMRPayer SituationClaim Reversal – Accepted/ApprovedValue1 RxBillingPayerUsageMMPayer Situation
CLAIM REVERSAL REJECTED RESPONSEField Field #5Ø4-F4Field #112-AN5Ø3-F351Ø-FA511-FBField #Response Transaction Header SegmentNCPDP Field NameValueVERSION/RELEASE NUMBERTRANSACTION CODETRANSACTION COUNTHEADER RESPONSE STATUSSERVICE PROVIDER ID QUALIFIERSERVICE PROVIDER IDDATE OF SERVICEDØB2Same value as in requestA AcceptedSame value as in requestSame value as in requestSame value as in requestResponse Message SegmentSegment Identification (111-AM) “2Ø”NCPDP Field NameTRANSACTION RESPONSE STATUSAUTHORIZATION NUMBERREJECT COUNTREJECT CODEResponse Claim SegmentSegment Identification (111-AM) “22”NCPDP Field Name455-EMPRESCRIPTION/SERVICE REFERENCENUMBER QUALIFIER4Ø2-D2PRESCRIPTION/SERVICE REFERENCENUMBERClaim Reversal – Accepted/RejectedPayer SituationClaim Reversal – Accepted/RejectedValueMESSAGEResponse Status SegmentSegment Identification (111-AM) “21”NCPDP Field NamePayerUsageMMMMMMMPayerUsageRPayer SituationReversal Not ProcessedClaim Reversal – Accepted/RejectedValueR RejectMaximum count of 5.PayerUsageMRRRPayer SituationClaim Reversal – Accepted/RejectedValue1 RxBillingPayerUsageMMPayer SituationImp Guide: For Transaction Code of “B2”, inthe Response Claim Segment, thePrescription/Service Reference NumberQualifier (455-EM) is “1” (Rx Billing).
Pharmacy Help Desk UHC Commercial 888-290-5416 Pharmacy Help Desk Oxford 855-816-6615 Pharmacy Help Desk OptumRx 800-788-7871 Other versions supported: ONLY D.0 CLAIM BILLING/CLAIM REBILL TRANSACTION Transaction Header Segment Claim Billing/Claim Rebill Field # NCPDP Field Name Value Payer .