Transcription
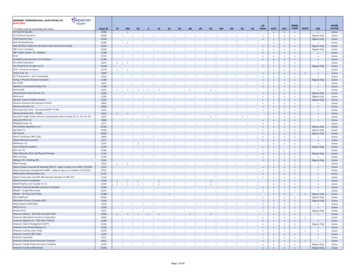
NCPDP Version D.0 Payer SheetMedicaidIMPORTANT NOTE: Express Scripts only accepts NCPDP Version D.0 electronic transactions. Thisdocumentation is to be used for programming the fields and values Express Scripts will accept when processingthese claims.Claim transaction segments not depicted within this document may be accepted during the transmission of aclaim. However, Express Scripts may not use the information submitted to adjudicate claims. All valuessubmitted will be validated against the NCPDP External Code List version as indicated below.This payer sheet includes processing information for both Legacy Express Scripts and Legacy Medco.General Information:Payer Name: Express ScriptsProcessor: Express ScriptsEffective: January 1, 2018NCPDP Data Dictionary Version Date: October 2016Communication Date: December 2017Switch:Version/Release Number: D.0NCPDP External Code List Version Date: October 2016NCPDP Emergency External Code List Version Date: July 2017Contact/Information Source: Network Contracting & Management Account Manager, or(800) 824-0898, or Express-Scripts.comPharmacy Help Desk Info: (800) 824-0898Other versions supported: N/ANote: All fields requiring alphanumeric data must be submitted in UPPER CASE.BIN/PCN TablePlan Name/Group NameLegacy ESI MedicaidBINØØ3858Legacy Medco MedicaidLegacy Medco – Secondary to Medicare Part DOther Payer Patient ResponsibilityLegacy Medco – Secondary to Medicare Part DOther Payer Primary (Based on Other Payer Paid)Legacy Medco – Secondary Payer Non-MedicarePart D (Based on Other Payer Paid)Legacy Medco – Member Balance Inquiry –Secondary Payer Non-Medicare Part D –Reimbursement based on Co-Pay OnlyLegacy Medco – Secondary Payer Non-MedicarePart D – Reimbursement based on Co-Pay OnlyEmblem Health Medicaid61ØØ1461ØØ31PCNA4 (or as assigned by ESI)SC (Use when secondary to Medicare Part D only)MA (refer to member’s card)As provided on card or anything except Ø56COPAY61ØØ14COPAYØ15748ØØ2Ø111ØØ1SC (Use when secondary to Medicare Part D only)1Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidPlan Name/Group NameWellPoint MedicaidAmerigroup, Community Care (MD, DE, WV, VA,PA)BIN61ØØ53,61Ø575 orØØ3858(Check ID cardto determinecorrect number)61ØØ84PCNPCN Not requiredPCN SC or spaces when secondary to MedicarePart DPRODUR1Section I: Claim Billing (In Bound)Transaction Header Segment – Mandatory in all casesField #NCPDP Field NameValue1Ø1-A11Ø2-A21Ø3-A31Ø4-A41Ø9-A9BIN NumberVersion Release NumberTransaction CodeProcessor Control NumberTransaction Count2Ø2-B22Ø1-B14Ø1-D111Ø-AKService Provider ID QualifierØ1 NPIService Provider IDPharmacy NPIDate of ServiceSoftware Vendor/Certification IDPatient Segment – RequiredField #NCPDP Field Name111-AM331-CX332-CY3Ø4-C43Ø5-C5Segment IdentificationPatient ID QualifierPatient IDDate of BirthPatient Gender Code31Ø-CA311-CB322-CM323-CNPatient First NamePatient Last NamePatient Street AddressPatient CitySee BIN/PCN table, aboveDØ Version D.0B1 BillingAs indicated above1 One Occurrence2 Two Occurrences3 Three Occurrences4 Four OccurrencesValueØ1 PatientAs indicated on member ID card1 Male2 FemaleExample: JohnExample: Smith2Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”Payer UsageMMMMM(BIN 61ØØ56 onlyallows TRANSCOUNT 1). Allothers allow 1-4MMMOPayer UsageMOORRRROO
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name324-CO Patient State or Province325-CP Patient Zip/Postal Code3Ø7-C7 Place of Service335-2C Pregnancy Indicator384-4X Patient ResidenceValueØ1 PharmacyBlank Not specified1 Not Pregnant2 PregnantPayer UsageOR*ROR*For Emergency/Natural Disaster claims, enter the current ZIP code of displaced patient in conjunction with Prior AuthorizationType Code (461-EU) and Prior Auth ID (462-EV) field.Insurance Segment – MandatoryField #NCPDP Field Name111-AM3Ø2-C2312-CC313-CD524-FO3Ø9-C9Segment IdentificationCardholder IDCardholder First NameCardholder Last NamePlan IDEligibility Clarification CodeValueØ4 InsuranceID assigned to the cardholder1 No Override2 Override3 Full Time Student4 Disabled Dependent5 Dependent Parent6 Significant OtherPayer UsageMMRROR3Ø1-C1 Group ID3Ø3-C3 Person CodeAs appears on card001-010Code assigned to specific person in a familyRR3Ø6-C6 Patient Relationship CodeØ Not Specified1 Cardholder – Individual who is enrolled in andreceives benefits from a health plan2 Spouse – Patient is the husband/wife/partner ofthe cardholder3 Child – Patient is a child of the cardholder4 Other – Relationship to cardholder is not preciseR359-2A Medigap IDO3Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidClaim Segment – MandatoryField #NCPDP Field Name111-AM455-EMSegment IdentificationPrescription/Service ReferenceNumber Qualifier4Ø2-D2436-E1Prescription/Service ReferenceNumberProduct/Service ID Qualifier4Ø7-D7442-E74Ø3-D3Product/Service ID*Quantity DispensedFill Number4Ø5-D54Ø6-D6Days SupplyCompound Code4Ø8-D8414-DE415-DFDispense as Written(DAW)/Product Selection CodeDate Prescription WrittenNumber of Refills Authorized419-DJPrescription Origin Code354-NXSubmission Clarification CodeCount42Ø -DKSubmission Clarification CodeValueØ7 Claim1 Rx Billing**Pharmacist should enter “1” when processingclaim for a vaccine drug and vaccineadministration.ØØ Not Specified*Ø3 National Drug CodeØ Original Dispensing1 to 99 Refill number1 Not a Compound2 Compound*Payer UsageMMMMMRRRRRØØ No refills authorizedØ1 through 99, with 99 being as needed, refillsunlimitedØ Not known1 Written2 Telephone3 Electronic4 Facsimile5 PharmacyMaximum count of 3RRRRW(SubmissionClarification Code(42Ø –DK) is usedRW (Clarification isneeded and valuesubmitted is greaterthan zero Ø). Thevalue of 2 is used torespond to a MaxDaily Dose/HighDose Reject)4Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValueØ Not Specified by patient1 No other coverage2 Other coverage exists - payment collected**3 Other coverage billed - claim not covered**4 Other coverage exists - payment notcollected**8 Claim is billing for patient financial responsibilityonly**Payer Usage3Ø8-C8Other Coverage CodeR454-EKScheduled Prescription IDNumber6ØØ-28Unit of MeasureEA EachGM GramsML Milliliters418-DILevel of ServiceØ Not specified1 Patient consultation (professional serviceinvolving provider/patient discussion of disease,therapy or medication regimen or other healthissues)2 Home delivery—provision of medications frompharmacy to patient’s place of residence3 Emergency—urgent provision of care4 24-hour service—provision of care throughoutthe day and night5 Patient consultation regarding generic productselection—professional service involvingdiscussion of alternatives to brand-namemedications6 In-Home Service—provision of care in patient’splace of residenceRW(This field couldresult in differentcoverage, pricing orpatient financialresponsibility)461-EUPrior Authorization Type CodeØ Not specified1 Prior Authorization2 Medical Certification6 Family Planning8 Payer Defined Exemption9 Emergency Preparedness***RW(Value 1, 6, 8 or 9 isused in conjunctionwith PriorAuthorization IDSubmitted (462-EV)RW(Must be providedwhen StateMedicaidRegulations requirethis information)5Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”R
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name462-EVPrior Auth ID Submitted357-NVDelay Reason Code995-E2Route of Administration147-U7Pharmacy Service Type456-ENAssociated Prescription/ServiceReference Number457-EPAssociated Prescription/ServiceDate343-HDDispensing Status344-HFQuantity Intended to beDispensed345-HGDays Supply Intended to beDispensedValueSubmitted when requested by processor.Examples: Prior authorization procedures forphysician authorized dosage or days supplyincreases for reject 79 'Refill Too Soon'.Ø1 Community/Retail Pharmacy ServicesØ3 Home Infusion Therapy ServicesØ5 Long Term Care Pharmacy ServicesP PartialC CompletePayer UsageRW(Field 461-EU 1,8 or 9)RW(Needed to specifythe reason thatsubmission oftransaction hasbeen delayed)†RW(Required forCompounds)RRW(Field 343-HD C or P)RW(Field 343-HD C or P)RW(Partial fill orcompletion of a fill)RW(Partial fill orcompletion of a fill)RW(Partial fill orcompletion of a fill)* The Product/Service ID (4Ø7-D7) must contain a value of “Ø” and Product/Service ID Qualifier (436-E1) must contain a value of“ØØ” when used for multi-ingredient compounds. Partial fills are not allowed for Multi-Ingredient Compound claims.**If Field 3Ø8-C8 is populated with Values 2, 3, 4 or 8, the COB segment should be sent. Note: For WellPoint claims, Values of 2, 3and 4 are acceptable. Value of 8 is not an acceptable value.***For Field 461-EU (Prior Authorization Type Code), Ø, 1, 2, 6, 8 and 9 are acceptable values. If value “9 EmergencyPreparedness” is populated in Field 461-EU, use 911ØØØØØØØ1 Emergency Preparedness (EP) Refill Too Soon Edit Override inField 462-EV when an emergency healthcare disaster has been officially declared by the appropriate U.S. government agency.Other values for the Field 462-EV for certain states are provided in the Express Scripts Network Provider Manual.†For Field 357-NV (Delay Reason Code), all valid values are accepted. Values of 1, 2, 7, 8, 9, 1Ø may be allowed to override Reject81 (Claim Too Old).6Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidPricing Segment – MandatoryField #NCPDP Field NameValuePayer Usage111-AM4Ø9-D9412-DC433-DX438-E3Segment IdentificationIngredient Cost SubmittedDispensing Fee SubmittedPatient Paid Amount SubmittedIncentive Amount Submitted11 PricingMRRORW(Value has an effecton Gross Amount(43Ø-DU)calculation. Usewhen submittingclaim for vaccinedrug andadministrative feetogether)481-HAFlat Sales Tax Amount SubmittedRW **(Value has an effecton Gross Amount(43Ø-DU)calculation)482-GEPercentage Sales Tax AmountSubmittedRW **(Value has an effecton Gross Amount(43Ø-DU)calculation)483-HEPercentage Sales Tax RateSubmittedRW **(Percentage SalesTax AmountSubmitted (482-GE)and PercentageSales Tax BasisSubmitted (484-JE)are used or ifneeded to calculatePercentage SalesTax Amount Paid(559-AX)7Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name484-JEPercentage Sales Tax BasisSubmitted426-DQ43Ø-DU423-DNUsual and Customary ChargeGross Amount DueBasis of Cost Determination*ValuePayer UsageRW(Percentage SalesTax AmountSubmitted(482-GE) andPercentage SalesTax Rate Submitted(483-HE) are used)RRR* All valid values are accepted. A value of “8” or “9” is accepted in field 423-DN for 34ØB dispensed drugs per StateMedicaid requirements. To identify 34ØB claims: Submitting Basis of Cost Determination code ―”Ø8” in field 423-DNplus their 34ØB acquisition cost in field 4Ø9-D9 (Ingredient Cost Submitted) OR Submitting Submission ClarificationCode value of ”2Ø” in field 42Ø-DK.**It is not permissible to submit Sales Tax unless required by State law.Prescriber Segment – Situational(This segment should only be submitted for claims that require a prescription.)Field #NCPDP Field Name111-AM466-EZSegment IdentificationPrescriber ID QualifierØ3 PrescriberØ1 NPI411-DB427-DR367-2NPrescriber IDNPI*Prescriber Last NamePrescriber State/Province AddressValuePayer UsageMRROO*Express Scripts edits the qualifiers in field 466-EZ. A valid Prescriber ID is required for all claims. Claims unable to bevalidated may be subject to post-adjudication review.Coordination of Benefits/Other Payments Segment – Situational(Required only for secondary, tertiary, etc. claims. Will support one transaction per transmission.)Field #111-AM337-4CNCPDP Field Name338-5C339-6CSegment IdentificationCoordination of Benefits/OtherPayments CountOther Payer Coverage TypeOther Payer ID Qualifier34Ø-7COther Payer IDValueØ5 COB/Other PaymentsMaximum count of 9Ø3 BINØ5 Medicare Carrier NumberPayer UsageMMMRW(Other Payer ID34Ø-7C is used)R8Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name443-E8341-HBOther Payer DateOther Payer Amount Paid Count342-HCOther Payer Amount PaidQualifier431-DVOther Payer Amount Paid471-5EOther Payer Reject Count472-6EOther Payer Reject Code353-NROther Payer – PatientResponsibility Amount Count351-NPOther Payer – PatientResponsibility Amount QualifierValueMaximum count of 9Maximum count of 5Maximum count of 139Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”Payer UsageRRW(Other PayerAmount PaidQualifier (342-HQ)is used)RW(Other PayerAmount Paid(431-DV) is used)RW(If other payer hasapproved paymentfor some/all of thebilling) (Not used fornon-governmentalagency programs ifOther Payer-PatientResponsibilityAmount (352-NQ) issubmitted) (Notused for patientfinancialresponsibility onlybilling)RW(Other Payer RejectCode 472-6E)is used)RW(Other Payer RejectCount (471-5E)is used)RW(Other Payer-PatientResponsibilityAmount Qualifier(351-NP) is used)RW(Other Payer-PatientResponsibilityAmount (352-NQ)is used)
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue352-NQOther Payer – PatientResponsibility Amount392-MUBenefit Stage CountMaximum count of 4393-MVBenefit Stage QualifierOccurs up to 4 times394-MWBenefit Stage AmountPayer UsageRW(Necessary forPatient FinancialResponsibilityOnly Billing)RW(Secondary toMedicare)RW(Secondary toMedicare)RW(Secondary toMedicare)The COB segment and all required fields must be sent if the Other Coverage Code (3Ø8-C8) field with values 2 through 4 or 8 aresubmitted in the claim segment.Note: If field 3Ø8-C8 (Other Coverage Code) is populated with: Value of 2 Other coverage exists – payment collected; fields 341-HB, 342-HC and 431-DV are required and must havevalues entered. Field 431-DV must not be zero ( 0.00). The sum of all occurrences must not be zero.Value of 3 Other coverage billed – claim not covered; fields 471-5E and 472-6E are required and must have valuesentered.Value of 4 Other coverage exists – payment not collected; fields 341-HB, 342-HC and 431-DV are required and must havevalues entered. Field 431-DV must be zero ( 0.00). The sum of all occurrences must be zero.Value of 8 Claim is billing for patient financial responsibility only; fields 353-NR, 351-NP and 352-NQ are required and musthave values entered. Note: WellPoint and Priority Health does not accept a value of 8 in field 3Ø8-C8.DUR/PPS Segment – SituationalField #NCPDP Field Name111-AM Segment Identification473-7E DUR/PPS Code Counter439-E4 Reason for Service Code44Ø-E5 Professional Service Code441-E6 Result of Service CodeValueØ8 DUR/PPS1 Rx Billing (Maximum of 9 occurrences)AT Additive ToxicityDD Drug-Drug InteractionØØ No interventionMØ Prescriber consultedMA Medication Administered – indicates theadministration of a covered vaccine*1G Filled, With Prescriber Approval10Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”Payer UsageMRRRR
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name474-8E DUR/PPS Level of EffortValue11 Level 1 (Lowest)12 Level 213 Level 314 Level 415 Level 5 (Highest)Payer UsageR***Indicates the claim billing includes a charge for the administration of the vaccine; leave blank if dispensing vaccine withoutadministration.**When submitting a compound claim, Field 474-8E is required; using the values consistent with your contract.Compound Segment – Situational(Required when submitting a compound claim. Will support only one transaction per transmission.)Field #NCPDP Field Name111-AM Segment Identification45Ø-EF Compound Dosage FormDescription Code451-EG Compound Dispensing Unit 1Ø CompoundValue1 Each2 Grams3 MillilitersCompound Ingredient Component Maximum 25 ingredientsCountCompound Product ID QualifierØ3 NDCCompound Product IDAt least 2 ingredients and 2 NDC #s.Number should equal field 447-EC.Compound Ingredient QuantityCompound Ingredient Drug CostCompound Ingredient Basis of CostDeterminationPayer UsageMMMMMMMRRClinical Segment – Situational(This segment may be required as determined by benefit design. When the segment is submitted, the fields defined below arerequired.)Field #111-AM491-VE492-WE424-DONCPDP Field NameSegment IdentificationDiagnosis Code CountDiagnosis Code QualifierDiagnosis CodeValue13 ClinicalMaximum count of 5Ø2 ICD-1011Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”Payer UsageMRRR
NCPDP Version D.0 Payer SheetMedicaidSection II: Response Claim Billing (Out Bound)Response Header Segment – MandatoryField #NCPDP Field Name1Ø2-A21Ø3-A31Ø9-A95Ø1-FIVersion Release NumberTransaction CodeTransaction CountHeader Response Status2Ø2-B2 Service Provider ID Qualifier2Ø1-B1 Service Provider ID4Ø1-D1 Date of ServiceValuePayer UsageDØ Version D.ØB1 BillingSame value as in requestA AcceptedR RejectedSame value as in requestSame value as in requestSame value as in requestMMMMMMMResponse Message Segment – SituationalField #NCPDP Field NameValuePayer UsageResponse Insurance Segment – MandatoryField #NCPDP Field NameValuePayer UsageValuePayer Usage111-AM Segment Identification5Ø4-F4 2Segment IdentificationGroup IDPlan IDNetwork Reimbursement IDPayer ID QualifierPayer IDCardholder ID2Ø Response Message25 Response Insurance5Ø3-F3 Authorization NumberMROROORNetwork IDResponse Status Segment – MandatoryField #NCPDP Field Name111-AM Segment Identification112-AN Transaction Response StatusMO21 Response StatusP PaidD Duplicate of PaidR Reject12MMRW(Transaction ResponseStatus P)Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name547-5F Approved Message Code CountValueMaximum count of 5548-6F Approved Message Code51Ø-FA Reject CountRW(Approved Message Code(548-6F) is used)RW(Approved Message CodeCount (547-5F) is used)Maximum count of 5511-FB Reject Code546-4F Reject Field Occurrence Indicator13Ø-UF Additional Message InformationCountPayer UsageMaximum count of 9132-UH Additional Message InformationQualifier526-FQ Additional Message InformationRW(Transaction ResponseStatus R)RW(Transaction ResponseStatus R)RW(Repeating field is in error toidentify repeating fieldoccurrence)RW(Additional Message(526-FQ) is used)RW(Additional Message(526-FQ) is used)RW(Additional text is needed forclarification or detail)RW(Current repetition ofAdditional MessageInformation(526-FQ) is used andanother repetition(526-FQ) follows, and text iscontinuation of the current)OOR*(*only returned on a rejectedresponse)131-UG Additional Message InformationContinuity549-7F Help Desk Phone Number Qualifier55Ø-8F Help Desk Phone Number987-MA URL13Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidResponse Claim Segment – MandatoryField #NCPDP Field Name111-AM Segment Identification455-EM Prescription/Service ReferenceNumber Qualifier4Ø2-D2 Prescription/Service ReferenceNumber551-9F Preferred Product CountValuePayer Usage22 Response Claim1 Rx BillingMMMMaximum count of 6552-AP Preferred Product ID QualifierRW(Based on benefit and whenpreferred alternatives areavailable for the submittedProduct Service ID)RW(If Preferred Product ID(553-AR) is used)553-AR Preferred Product IDRW(If a product preference existsthat needs to becommunicated to the receivervia an ID)556-AU Preferred Product DescriptionRW(If a product preference existsthat either cannot becommunicated by thePreferred Product ID(553-AR) or to clarify thePreferred Product ID(553-AR)Response Pricing Segment – Mandatory(This segment will not be included with a rejected response)Field #111-AM5Ø5-F55Ø6-F65Ø7-F7NCPDP Field NameSegment IdentificationPatient Pay AmountIngredient Cost PaidDispensing Fee PaidValue23 Response Pricing14Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”Payer UsageMRRR
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue557-AV Tax Exempt Indicator558-AW Flat Sales Tax Amount Paid559-AX Percentage Sales Tax Amount PaidPayer UsageRW(If sender and/or patient is taxexempt and exemptionapplies to this billing)RW(If Flat Sales Tax AmountSubmitted (481-HA) isgreater than zero (Ø) or ifFlat Sales Tax Amount Paid(558-AW) is used to arrive atfinal reimbursement)RW(If Percentage Tax AmountSubmitted (482-GE) isgreater than zero (Ø) orPercentage Sales TaxRate Paid (56Ø-AY) andPercentage Sales TaxBasis Paid(561-AZ) are used)56Ø-AY Percentage Sales Tax Rate PaidRW(If Percentage Sales TaxAmount Paid (559-AX) isgreater than zero (Ø))561-AZ Percentage Sales Tax Basis PaidRW(If percentage Sales TaxAmount Paid (559-AX) isgreater than zero (Ø))521-FL Incentive Amount Paid563-J2564-J3565-J4566-J55Ø9-F9522-FMOther Amount Paid CountOther Amount Paid QualifierOther Paid AmountOther Payer Amount RecognizedTotal Amount PaidBasis of ReimbursementDeterminationRW(If Incentive AmountSubmitted (438-E3) isgreater than zero (Ø))Occurs up to 3 timesOccurs up to 3 times15Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”OOOORR
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue523-FN Amount Attributed to Sales Tax512-FC513-FD514-FE517-FHAccumulated Deductible AmountRemaining Deductible AmountRemaining Benefit AmountAmount Applied to PeriodicDeductible518-FIAmount of Co-payPayer UsageRW(If Patient Pay Amount (5Ø5F5) includes sales tax that isthe financial responsibility ofthe member but is not alsoincluded in any of the otherfields that add up to PatientPay Amount)OOORW(If Patient Pay Amount(5Ø5-F5) includes deductibleRW(Patient Pay Amount(5Ø5-F5) includesco-pay as patient financialresponsibility)RW(Patient Pay Amount(5Ø5-F5) includes amountexceeding periodic benefitmaximum)52Ø-FK Amount Exceeding Periodic BenefitMaximum571-NZ Amount Attributed to ProcessorFeeRW(If customer is responsible for100% of the prescriptionpayment and when theprovider net sale is less thanthe amount the customer isexpected to pay)575-EQ Patient Sales Tax AmountRW(Used when necessary toidentify Patient’s portion ofthe Sales Tax)574-2Y Plan Sales Tax AmountRW(Used when necessary toidentify Plan’s portion of theSales Tax)16Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue572-4U Amount of CoinsurancePayer UsageRW(Patient Pay Amount(5Ø5-F5) includescoinsurance as patientfinancial responsibility)577-G3 Estimated Generic SavingsRW(Patient selects brand drugwhen generic was available)128-UC Spending Account AmountRemainingRW(If known when transactionhad spending account dollarsreported as part of the patientpay amount)129-UD Health Plan-Funded AssistanceAmountRW(Patient meets the planfunded assistance criteria toreduce Patient Pay Amount(5Ø5-F5)134-UK Amount Attributed to ProductSelection/Brand DrugRW(Patient Pay Amount(5Ø5-F5) includes anamount that is attributableto a patient’s selectionof a Brand drug)133-UJ Amount Attributed to ProviderNetwork SelectionRW(Patient Pay Amount(5Ø5-F5) includes anamount that is attributable toa cost share differential dueto the selection of onepharmacy over another)17Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue135-UM Amount Attributed to ProductSelection/Non-Preferred FormularySelectionPayer UsageRW(Patient Pay Amount (5Ø5F5) includes an amount thatis attributable to a patient’sselection of a non-preferredformulary product)136-UN Amount Attributed to ProductSelection/Brand Non-PreferredFormulary SelectionRW(Patient Pay Amount (5Ø5F5) includes an amount thatis attributable to a patient’sselection of a Brand nonpreferred formulary product)148-U8 Ingredient CostContracted/Reimbursable AmountRW(Basis of ReimbursementDetermination (522-FM) is“14” (Patient ResponsibilityAmount) or “15” (Patient PayAmount) unless prohibited bystate/federal/regulatory agency)149-U9 Dispensing FeeContracted/Reimbursable AmountRW(Basis of ReimbursementDetermination (522-FM) is“14” (Patient ResponsibilityAmount) or “15” (Patient PayAmount) unless prohibited bystate/federal/regulatory agency)Response DUR/PPS Segment – SituationalField #NCPDP Field NameValue111-AM Segment Identification24 Response DUR/PPS567-J6 DUR/PPS Response Code Counter Maximum 9 occurrences supported439-E4 Reason for Service Code528-FS Clinical Significance CodeAT Additive ToxicityER OveruseDD Drug-Drug Interaction18Payer UsageMRW(Reason for Service Code(439-E4) is used)OPayer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”O
NCPDP Version D.0 Payer SheetMedicaidField #529-FT53Ø-FU531-FV532-FW533-FX544-FY57Ø-NSNCPDP Field NameValueOther Pharmacy IndicatorPrevious Date of FillQuantity of Previous FillDatabase IndicatorOther Prescriber IndicatorDUR Free Text MessageDUR Additional TextPayer UsageOOOOOOOResponse Prior Authorization Segment – Situational(Provided when the receiver has an opportunity to reprocess claim using a Prior Authorization ID)Field #NCPDP Field Name111-AM Segment Identification498-PY Prior Authorization ID - AssignedValuePayer Usage26 Response Prior AuthorizationMRW(Receiver mustsubmit this PriorAuthorization ID inorder to receivepayment for theclaim)Response Coordination of Benefits/Other Payers – Situational(This segment will not be included with a rejected response)Field #NCPDP Field Name111-AM Segment Identification355-NT Other Payer ID Count338-5C Other Payer Coverage Type339-6C Other Payer ID QualifierValue28 Response Coordination of Benefits/OtherPayersMaximum count of 9Payer UsageMMMRW(Other Payer ID(34Ø-7C) is used)34Ø-7C Other Payer ID991-MH Other Payer Processor ControlNumber356-NU Other Payer Cardholder ID992-MJ Other Payer Group IDRW*RW*RW*RW*19Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field NameValue142-UV Other Payer Person Code127-UB Other Payer Help Desk PhoneNumberPayer UsageRW (Needed to uniquelyidentify the family memberswithin the Cardholder ID, asassigned by other payer)RW (Needed to provide asupport telephone number ofother payer to the receiver)*Will be returned when other insurance information is available for COB.Section III: Reversal Transaction (In Bound)Transaction Header Segment – MandatoryField #NCPDP Field -B14Ø1-D111Ø-AKBIN NumberVersion Release NumberTransaction CodeProcessor Control NumberTransaction CountService Provider ID QualifierService Provider IDDate of ServiceSoftware Vendor/Certification IDValuePayer UsageValuePayer UsageValuePayer UsageBIN used on original claim submissionDØ Version D.ØB2 ReversalPCN used on original claim submission1 One occurrence per B2 transmissionØ1 NPINPINote: Reversal window is 9Ø days.Insurance Segment – MandatoryField #NCPDP Field Name111-AM Segment Identification3Ø2-C2 Cardholder IDClaim Segment – MandatoryField #NCPDP Field Name111-AM Segment Identification445-EM Prescription /Service ReferenceNumber Qualifier4Ø2-D2 Prescription/Service ReferenceNumber436-E1 Product/Service ID QualifierØ4 InsuranceID assigned to the cardholderØ7 Claim1 Rx BillingMMMMMMMMOMMMMMValue used on original claim submission20Payer Usage: M Mandatory, O Optional, R Required by ESI to expedite claim processing,"R" Repeating Field, RW Required when; required if “x”, not required if “y”R
NCPDP Version D.0 Payer SheetMedicaidField #NCPDP Field Name4Ø7-D7 Product/Service ID4Ø3-D3 Fill Number3Ø8-C8 Other Coverage CodeValuePayer UsageRRRValue used on original claim submissionCoordination of Benefits/Other Payments Segment – Situational(Will support only one transaction per transmission)Field #111-AM337-4C338-5CNCPDP Field NameSegment IdentificationCoordination of Benefits/OtherPayments CountOther Payer Coverage TypeValuePayer UsageØ5 COB/Other PaymentsMaximum count of 9MMMSection IV: Reversal Response Transaction (Out Bound)R
(800) 824-0898, or Express-Scripts.com Pharmacy Help Desk Info: (800) 824-0898 Other versions supported: N/A Note: All fields requiring alphanumeric data must be submitted in UPPER CASE. BIN/PCN Table . . * The Product/Service ID (4Ø7-D7) must contain a value of "Ø" and Product/Service ID Qualifier (436-E1) must contain a value of .