Transcription
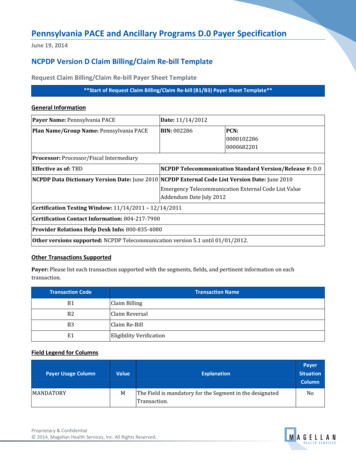
Pennsylvania PACE and Ancillary Programs D.0 Payer SpecificationJune 19, 2014NCPDP Version D Claim Billing/Claim Re-bill TemplateRequest Claim Billing/Claim Re-bill Payer Sheet Template**Start of Request Claim Billing/Claim Re-bill (B1/B3) Payer Sheet Template**General InformationPayer Name: Pennsylvania PACEDate: 11/14/2012Plan Name/Group Name: Pennsylvania PACEBIN: 002286PCN:00001022860000682201Processor: Processor/Fiscal IntermediaryEffective as of: TBDNCPDP Telecommunication Standard Version/Release #: D.0NCPDP Data Dictionary Version Date: June 2010 NCPDP External Code List Version Date: June 2010Emergency Telecommunication External Code List ValueAddendum Date July 2012Certification Testing Window: 11/14/2011 – 12/14/2011Certification Contact Information: 804-217-7900Provider Relations Help Desk Info: 800-835-4080Other versions supported: NCPDP Telecommunication version 5.1 until 01/01/2012.Other Transactions SupportedPayer: Please list each transaction supported with the segments, fields, and pertinent information on eachtransaction.Transaction CodeTransaction NameB1Claim BillingB2Claim ReversalB3Claim Re-BillE1Eligibility VerificationField Legend for ColumnsPayer Usage ColumnMANDATORYValueMExplanationThe Field is mandatory for the Segment in the designatedTransaction.Proprietary & Confidential 2014, Magellan Health Services, Inc. All Rights Reserved.PayerSituationColumnNo
Magellan Medicaid AdministrationPayer Usage ColumnPennsylvania PACE and Ancillary Programs D.0 Payer The Field has been designated with the situation of “Required”for the Segment in the designated Transaction.NoRW“Required when.” The situations designated have qualificationsfor usage (“Required if x,” “Not required if y”).YesREQUIREDQUALIFIED REQUIREMENTFields that are not used in the Claim Billing/Claim Re-bill transactions and those that do not have qualifiedrequirements (i.e., not used) for this payer are excluded from the template.Claim Billing/Claim Re-bill TransactionThe following lists the segments and fields in a Claim Billing or Claim Re-bill Transaction for the NCPDPTelecommunication Standard Implementation Guide Version D.Ø.Transaction Header Segment QuestionsThis Segment is always sentXSource of certification IDs required inSoftware Vendor/Certification ID (11ØAK) is Payer IssuedXTransaction Header SegmentField #Claim Billing/Claim Re-billIf Situational, Payer SituationCheckClaim Billing/Claim Re-billNCPDP Field NameValuePayerUsage1Ø1-A1 BIN NUMBERØØ2286M1Ø2-A2 VERSION/RELEASE NUMBERDØM1Ø3-A3 TRANSACTION CODE 1Ø4-A4 PROCESSOR CONTROLNUMBERTrOOP Claims: B1 BillingB2 ReversalB3 Re-billE1 EligibilityVerificationØØØØ1Ø2286Non-TrOOP Claims: Payer SituationMMIMPORTANT: USE THE CORRECTPCN: ØØØØ6822Ø1TrOOP claims include thefollowing programs: Non-TrOOP claims include: Proprietary & ConfidentialPACE, CRDP, SPBP1, andSPBP 2CF, SB, MSUD, PKU, PAP,AutoCAT, WCSFPage 2 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationTransaction Header SegmentField #Claim Billing/Claim Re-billNCPDP Field NameValue1 One Occurrence2 Two Occurrences3 Three Occurrences4 Four OccurrencesPayerUsage1Ø9-A9 TRANSACTION COUNT 2Ø2-B2 SERVICE PROVIDER IDQUALIFIERØ1 – National ProviderIdentifier (NPI)M2Ø1-B1 SERVICE PROVIDER IDNPIM4Ø1-D1 DATE OF SERVICEFormat CCYYMMDDM11Ø-AK SOFTWAREVENDOR/CERTIFICATION IDAssigned by Magellan HealthServicesClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentXInsurance SegmentSegment Identification (111-AM) “Ø4”Field #MMInsurance Segment QuestionsPayer SituationClaim Billing/Claim Re-billNCPDP Field NameValue3Ø2-C2 CARDHOLDER IDPayerUsageMPayer Situation PACE through PAP - 9 characterIDAutoCAT and WCSF # thatappears on the card.IMPORTANT: AutoCAT IDs MAYCONTAIN A DASH (-). THE DASHMUST BE INCLUDED.3Ø1-C1 GROUP ID PACECRDPADAPSPBPCFSBMSUDPKUPAPAUTOCATWCSFR Proprietary & ConfidentialPACE PACE/PACENETCRDP Chronic Renal DiseaseProgramADAP SpecialPharmaceutical BenefitsProgram SP1 cardholdersSPBP SpecialPharmaceutical BenefitsProgram SP2 cardholdersCF Cystic FibrosisSB Spina BifidaMSUD Maple Syrup UrineDiseasePKU PhenylketonuriaPage 3 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationInsurance SegmentSegment Identification (111-AM) “Ø4”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer Situation 3Ø6-C6 PATIENT RELATIONSHIP CODEWorkers’ Compensation SegmentQuestionsRPAP PA Patient AssistanceProgramAutoCAT Catastrophic LossBenefits Continuation FundWCSF Workers’ CompensationSecurity Fund1 CardholderClaim Billing/Claim Re-billIf Situational, Payer SituationCheckThis Segment is always sentThis Segment is situationalXWorkers’ Compensation SegmentSegment Identification (111-AM) “Ø6”Field #NCPDP Field Name434-DY DATE OF INJURY315-CF EMPLOYER NAMEIt is used when processing a Claim Billing forCatastrophic Loss Benefits Continuation Fund(AutoCAT) or Workers’ CompensationSecurity Fund (WCSF).Claim Billing/Claim Re-billValuePayerUsagePayer SituationMRWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.316-CG EMPLOYER STREET ADDRESSRWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.317-CH EMPLOYER CITY ADDRESSRWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.318-CI EMPLOYER STATE/PROVINCEADDRESSProprietary & ConfidentialRWImp Guide: Required if needed toprocess a claim/encounter for aPage 4 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationWorkers’ Compensation SegmentSegment Identification (111-AM) “Ø6”Field #NCPDP Field NameClaim Billing/Claim Re-billValuePayerUsagePayer Situationwork related injury or condition.Payer Requirement: Same as ImpGuide.319-CJ EMPLOYER ZIP/POSTAL ZONERWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.32Ø-CK EMPLOYER PHONE NUMBERRWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.327-CR CARRIER IDRWImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement: Same as ImpGuide.435-DZ CLAIM/REFERENCE IDMImp Guide: Required if needed toprocess a claim/encounter for awork related injury or condition.Payer Requirement:Enter the AutoCAT # or WCSF #that appears on the ID card in thisfield.IMPORTANT: AutoCAT IDs MAYCONTAIN A DASH (-). THE DASHMUST BE INCLUDED.117-TR BILLING ENTITY TYPEINDICATORØØ Provider SubmittedPay to ProviderRFor AutoCAT and WCSF, this willalways be ØØ.126-UAPatient Segment QuestionsCheckClaim Billing/Claim Re-billIf Situational, Payer SituationThis Segment is always sentThis Segment is situationalProprietary & ConfidentialXRequired for B1 and B3 transactions.Page 5 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationPatient SegmentSegment Identification (111-AM) “Ø1”FieldClaim Billing/Claim Re-billNCPDP Field NameValue3Ø4-C4 DATE OF BIRTH3Ø5-C5 PATIENT GENDER CODEPayerUsagePayer SituationR Ø Not Specified1 Male2 Female31Ø-CA PATIENT FIRST NAMERRImp Guide: Required when thepatient has a first name.Payer Requirement: Required forpatient name validation.311-CB PATIENT LAST NAMERImp Guide: Required when thepatient has a last name.Payer Requirement: Required forpatient name validation.384-4X PATIENT RESIDENCE Proprietary & ConfidentialØ Not Specified1 Home2 Skilled NursingFacility. PART B ONLY3 Nursing Facility4 Assisted LivingFacility5 Custodial CareFacility. PART B ONLY6 Group Home7 Inpatient PsychiatricFacility8 Psychiatric Facility –Partial Hospitalization9 Intermediate CareFacility/MentallyRetarded1Ø ResidentialSubstance AbuseTreatment Facility11 Hospice12 PsychiatricResidential TreatmentFacility13 ComprehensiveInpatient RehabilitationFacility14 Homeless ShelterRImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement: Same as ImpGuide. Patient Residence 3 NursingFacility required when recipientis identified as a long-term careresident.Ø “Not Specified” will deny.Page 6 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim Segment QuestionsThis Segment is always sentXThis payer supports partial fillsXClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field Name455-EM PRESCRIPTION/SERVICEREFERENCE NUMBERQUALIFIERClaim Billing/Claim Re-billIf Situational, Payer SituationCheckValue1 Rx Billing4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBER436-E1 PRODUCT/SERVICE IDQUALIFIER 456-EN ASSOCIATEDPRESCRIPTION/SERVICEREFERENCE NUMBERMPayer SituationPayer Requirement: For TransactionCode of “B1,” in the Claim Segment,the Prescription/Service ReferenceNumber Qualifier (455-EM) is “1”(Rx Billing).M 4Ø7-D7 PRODUCT/SERVICE IDPayerUsageØ3 National DrugCode (NDC)ØØ Not SpecifiedMNDC for non-compoundclaims“Ø” for compoundclaimsMRWPayer Requirement: Use “ØØ” forcompounds.Required if the “completion”transaction in a partial fill(Dispensing Status [343-HD] “C”[Completed]).Required if the Dispensing Status(343-HD) “P” (Partial Fill) andthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide.457-EP ASSOCIATEDPRESCRIPTION/SERVICE DATERWImp Guide: Required if the“completion” transaction in a partialfill (Dispensing Status [343-HD] “C” [Completed]).Required if AssociatedPrescription/Service ReferenceNumber (456-EN) is used.Required if the Dispensing Status(343-HD) “P” (Partial Fill) andProprietary & ConfidentialPage 7 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsagePayer Situationthere are multiple occurrences ofpartial fills for this prescription.Payer Requirement: Same as ImpGuide.442-E7 QUANTITY DISPENSEDMetric Decimal Quantity4Ø3-D3 FILL NUMBER Ø Original dispensingRefill number – Numberof the replenishment4Ø5-D5 DAYS SUPPLY4Ø6-D6 COMPOUND CODERR 4Ø8-D8 DISPENSE AS WRITTEN(DAW)/PRODUCT SELECTION CODE Proprietary & ConfidentialR1 Not a Compound2 CompoundRØ No ProductSelection Indicated1 Substitution NotAllowed by Prescriber2 SubstitutionAllowed-PatientRequested ProductDispensed3 SubstitutionAllowed-PharmacistSelected ProductDispensed4 SubstitutionAllowed-Generic DrugNot in Stock5 SubstitutionAllowed-Brand DrugDispensed as a Generic6 Override7 Substitution NotAllowed-Brand DrugMandated by Law8 SubstitutionAllowed-Generic DrugNot Available inMarketplace9 SubstitutionRPACE Maximum of 30 whenprimary. Other program’s daysupply may differ. PACE, CRDP, AutoCAT, WCSFDAW 1 subject to M.E. processfor PACE. DAW 1 accepted forAutoCAT and WCSF.DAW 5 used only whensubmitted U&C is equal to orless than generic. DAW 5 notaccepted in lieu of a MedicalException for an A Rated brandproduct when PACE is primarypayer.Page 8 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsagePayer SituationAllowed By Prescriberbut Plan Requests Brand– Patient's PlanRequested BrandProduct To BeDispensed414-DE DATE PRESCRIPTIONWRITTEN415-DF NUMBER OF REFILLSAUTHORIZEDR Ø No refills authorized1-99 Authorized Refillnumber – with 99 beingas needed, refillsunlimitedRImp Guide: Required if necessary forplan benefit administration.Payer Requirement: Same as ImpGuide. PACE, CRDP, SPBP, and allother Pennsylvania Department ofAging administered plans use aninternal counter that limits refills tomaximum of 5 although prescribermay authorize more.Note: Value of “99” is not acceptablefor any PDA-administeredprograms.419-DJ PRESCRIPTION ORIGIN CODE354-NX SUBMISSION CLARIFICATIONCODE COUNT Ø Not Known1 Written2 Telephone3 Electronic4 Facsimile5 PharmacyMaximum count of 3.RImp Guide: Required if necessary forplan benefit administration.Payer Requirement: Value of “Ø” willdeny as Invalid. All other codes areaccepted.RW*** Imp Guide: Required if SubmissionClarification Code (42Ø-DK) is used.Payer Requirement: Required ifSubmission Clarification Code (42ØDK) is used.42Ø-DK SUBMISSION CLARIFICATIONCODEProprietary & Confidential 1 No Override2 Other Override3 Vacation Supply4 Lost Prescription5 Therapy Change6 Starter Dose7 Medically Necessary8 Process CompoundFor ApprovedRWImp Guide: Required if clarification isneeded and value submitted isgreater than zero (Ø).Payer Requirement: Required whenneeded to provide additionalinformation for coverage purposes.NOTE: SPBP1 providers: See SPBP1Provider Agreement Section I.N.Value #8 may be used for multiPage 9 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValue Proprietary & ConfidentialIngredients9 Encounters1Ø Meets PlanLimitations11 Certification on File12 DME ReplacementIndicator13 Payer-RecognizedEmergency/DisasterAssistance Request14 Long-Term CareLeave of Absence15 Long-Term CareReplacementMedication16 Long-Term CareEmergency box (kit) orautomated dispensingmachine17 Long-Term CareEmergency supplyremainder18 Long-Term CarePatient Admit/ReadmitIndicator2Ø 34ØB21 LTC dispensing: 14days or less notapplicable – Fourteenday or less dispensing isnot applicable due toCMS exclusion and/ormanufacturer packagingmay not be broken orspecial dispensingmethodology (i.e.,vacation supply, leave ofabsence, ebox, spitterdose). Medicationquantities are dispensedas billed22 LTC dispensing: 7PayerUsagePayer Situationingredient compounds.Value #3 accepted only for SpecialPharmaceutical Benefits Programcardholders.Value #20 MUST be entered whensubmitting a drug purchasedunder Section 340B of the PublicHealth Service Act.Other values accepted, but editedONLY for data integrity, i.e. noillegal characters, etc.Page 10 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValue Proprietary & ConfidentialPayerUsagePayer Situationdays – Pharmacydispenses medication in7 day supplies23 LTC dispensing: 4days – Pharmacydispenses medication in4 day supplies24 LTC dispensing: 3days – Pharmacydispenses medication in3 day supplies25 LTC dispensing: 2days – Pharmacydispenses medication in2 day supplies26 LTC dispensing: 1day – Pharmacy orremote (multiple shifts)dispenses medication in1 day supplies27 LTC dispensing: 43 days – Pharmacydispenses medication in4 day, then 3 daysupplies28 LTC dispensing: 23 days – Pharmacydispenses medication in2 day, then 2 day, then 3day supplies29 LTC dispensing:daily and 3-dayweekend – Pharmacy orremote dispensed dailyduring the week andcombines multiple daysdispensing forweekends30 LTC dispensing:Per shift dispensing –Remote dispensing pershift (multiple medPage 11 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValue 3Ø8-C8 OTHER COVERAGE CODE Proprietary & ConfidentialPayerUsagePayer Situationpasses)31 LTC dispensing:Per med passdispensing – Remotedispensing per medpass32 LTC dispensing:PRN on demand –Remote dispensing ondemand as needed33 LTC dispensing: 7day or less cycle nototherwise represented34 LTC dispensing: 14days dispensing –Pharmacy dispensesmedication in 14 daysupplies35 LTC dispensing: 8–14 day dispensingmethod not listed above– 8–14-Day dispensingcycle not otherwiserepresented36 LTC dispensing:dispensed outside shortcycle – Claim wasoriginally submitted to apayer other thanMedicare Part D andwas subsequentlydetermined to be Part D.Ø Not Specified bypatient1 No other coverage2 Other coverageexists-paymentcollected3 Other CoverageBilled – claim notcovered4 Other coverageRWImp Guide: Required if needed byreceiver, to communicate asummation of other coverageinformation that has been collectedfrom other payers.Required for Coordination ofBenefits.Payer Requirement: Same as ImpGuide.Page 12 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValuePayerUsagePayer Situationexists-payment notcollected429-DT SPECIAL PACKAGINGINDICATOR Proprietary & ConfidentialØ Not Specified1 Not Unit Dose –Indicates the product isnot being dispensed inspecial unit dosepackaging.2 Manufacturer UnitDose – A code used toindicate a distinct doseas determined by themanufacturer.3 Pharmacy Unit Dose– Used to indicate whenthe pharmacy hasdispensed the drug in aunit of use packagewhich was “loaded” atthe pharmacy – notpurchased from themanufacturer as a unitdose.4 Pharmacy Unit DosePatient CompliancePackaging – Unit doseblister, strip or otherpackaging designed incompliance-promptingformats that help peopletake their medicationsproperly.5 Pharmacy Multidrug PatientCompliance Packaging –Packaging that maycontain drugs frommultiple manufacturerscombined to ensurecompliance and safeadministration6 Remote Device UnitPage 13 of 68Revision Date: June 20, 2014June 19, 2014
Magellan Medicaid AdministrationPennsylvania PACE and Ancillary Programs D.0 Payer SpecificationClaim SegmentSegment Identification (111-AM) “Ø7”Field #Claim Billing/Claim Re-billNCPDP Field NameValue 6ØØ-28 UNIT OF MEASURE PayerUsagePayer SituationDose– Drug is dispensedat the facility, via aremote device, in a unitof use package7 Remote DeviceMulti‐drug Compliance– Drug is dispensed atthe facility, via a remotedevice, with packagingthat may contain drugsfrom multiplemanufacturerscombined to ensurecompliance and safeadministration8 Manufacturer Unit ofUse Package (not unitdose) – Drug isdispensed by pharmacyin originalmanufacturer’s packageand relabeled for use.Applicable in long termcare claims only (asdefined in theTelecommunicationEditorial Document).EA EachGM GramsML MillilitersRWImp Guide: Required if necessary forstate/federal/regulatory agencyprograms.Required if this field could result indifferent coverage, pricing, orpatient financial responsibility.Payer Requirement: Same as ImpGuide. Required for all claimsubmissions.418-DI LEVEL OF SERVICEProprietary & Confidential Ø Not Specified1 Patient consultation2 Home delivery3 Emergency4 24-hour serviceRWImp Guide: Required if this fieldcould result in different coverage,pricing, or patient financialresponsibility.Payer Requirement:Page 14 of 68Revision Date: June 20, 2014June 19, 2014
Jun 19, 2014 · Provider Relations Help Desk Info: 800-835-4080 Other versions supported: NCPDP Telecommunication version 5.1 until 01/01/2012. Other Transactions Supported Payer: Please list each transaction supported with the segments, fields, and pertinent information on each transaction. Transaction