Transcription
(2020) 18:84Ong et al. Hum Resour en AccessCASE STUDYStrengthening the clinical laboratoryworkforce in Cambodia: a case studyof a mixed‑method in‑service training programto improve laboratory quality managementsystem oversightSiew Kim Ong1†, Grant T. Donovan2†, Nayah Ndefru2, Sophanna Song1, Chhayheng Leang1, Sophat Sek1,Michael Noble4 and Lucy A. Perrone2,3*AbstractBackground: Laboratory diagnostic testing service delivery and compliance with international standards for laboratory quality are directly influenced by laboratory workforce competency. Many hospital laboratories in constrainedresource settings such as Cambodia struggle to cope with the training needs of laboratory professionals in an environment of competing healthcare development priorities. Resource-limited countries need an adaptable and effective approach to provide laboratory professionals with job-specific quality oversight training to ensure the accuracy,timeliness, and reliability of diagnostic services.Case presentation: Here, we describe the results of an in-service training and mentoring program conducted withthe Cambodia Ministry of Health at 12 tertiary-level hospital laboratories to drive improvements in laboratory quality management systems toward ISO 15189 accreditation, which demonstrated significant progress between baseline and outcome audits in a concurrent study. This case study describes the program, and evaluates how the fourprimary activities, including actionable gap assessments and planning, centralized and in situ training curriculum,in-person mentoring, and remote tele-mentoring via video communication technologies, contributed towards qualityimprovement in the participating laboratories. We evaluated participant responses to Likert scale and free responsequestions from program and training evaluation surveys, and we used thematic analysis to develop a model of bestpractices within the program’s four primary activities to inform future training approaches. Of these activities, participants agreed most highly that in-person visits and planning based on gap assessments contributed to their learningand ability to improve laboratory operations. Tele-mentoring was rated lowest by participants, who were critical ofexcessive group dialogue and distraction during web-conferencing; however, feedback suggests both in-person andremote mentoring contribute to continuing education, accountability to action, and peer collaboration and problemsolving to improve workforce efforts toward improved quality management systems.*Correspondence: perronel@uw.edu†Siew Kim Ong and Grant T. Donovan contributed equally to the writingof this manuscript3Department of Laboratory Medicine, School of Medicine, Universityof Washington, Seattle, WA, USAFull list of author information is available at the end of the article The Author(s) 2020. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, whichpermits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to theoriginal author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images orother third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit lineto the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutoryregulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of thislicence, visit http://creat iveco mmons .org/licen ses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creat iveco mmons .org/publi cdoma in/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Ong et al. Hum Resour Health(2020) 18:84Page 2 of 9Conclusions: We recommend here a package of in-service training activities for laboratory quality managementsystem improvement initiatives in resource constrained settings that includes needs-based curricula and personalizedaction plans for participants; interactive and on-site training workshops; and in-person mentoring, complementedwith well managed and regular tele-mentoring that focuses on knowledge retention, accountability to goals, and collaborative problem solving. Our model presents an adaptable approach to human resource development for qualityimprovement in medical laboratories.Keywords: Laboratory quality management systems, Laboratory in-service training, Training methodology,Laboratory mentoring, Laboratory tele-mentoringBackgroundLaboratory-based diagnostic testing plays a critical rolein clinical decision-making and public health and accurate laboratory data are essential for informed decisionmaking [1–3]. Laboratory errors caused by poor qualitymanagement practices can lead to patient harm and aloss of trust by clinicians, resulting in the decreased useof diagnostic testing data for clinician decision-makingand a cycle of poor quality, as often observed in resourcelimited countries [4]. For the last 20 years, a significantinternational effort has been underway to assure a cultureof quality and competence in laboratory testing throughthe implementation of laboratory quality managementsystems (LQMS) aligned with the International Organization for Standardization (ISO) ISO 15189 standard formedical laboratories [5]. This standard specifies requirements for quality and competence for medical laboratories globally; however, this standard is stringent andmany countries lack the resources and trained personnelto achieve and maintain ISO 15189 accreditation withoutassistance [6]. Meeting national diagnostic services andinternational accreditation goals requires a laboratoryworkforce capable of complex organizational management and technical excellence. In low-resource settings,medical laboratory personnel are often limited by theireducational and professional development opportunities and subsequent knowledge of the biological principles of diagnostic testing and quality assurance practicesrequired to carry out testing procedures with repeatableaccuracy [7].In 2016, the first joint external evaluation was conducted to measure Cambodia’s achievements towardsmeeting the International Health Regulations. Thisrevealed gaps in the areas of LQMS and workforce capacity, and additional investments in these areas were recommended to the Ministry of Health (MoH) [8]. TheInternational Training and Education Center for Health(I-TECH) supported the Cambodia MoH Bureau of Medical Laboratory Services (BMLS) to implement a mentored LQMS strengthening program for 12 national andprovincial hospital laboratories to improve quality management practices [9, 10]. The training and mentoringprogram presented in this case study began in July 2017and included a package of practice-based in situ LQMSeducation and training activities, on-site mentorship,and frequent remote tele-mentoring support to all 12laboratories. All technical assistance (TA) support wastailored towards improving each laboratory’s compliance with the ISO 15189 standard over the 2 years ofimplementation. Laboratory progress as a result of thisTA was benchmarked against the CamLQMS assessmenttool [a tool adapted from the WHO-AFRO StepwiseLaboratory Improvement Process Towards Accreditation (SLIPTA) tool and adopted in 2018 by the MoH asthe primary assessment tool for laboratories in Cambodia]. The CamLQMS audits measured significant facility-level progress, with the 12 participating laboratoriesimproving audit scores by an average percent differenceof 21% (SD 10%, Min 7%, Max 37%), demonstratingstrengthened capacity of laboratory personnel to implement LQMS in their facilities [11]. A moderately strongcorrelation between audit performance and attendancetime of laboratory personnel in remote mentoring activities suggested that remote mentoring could significantlycontribute to substantial progress [11]; however, furtherexamination of this correlation was warranted to betterunderstand the impact of each element of the trainingand mentoring program and elucidate best practices forfuture programs. This examination is the subject of thiscase study.Case presentationThis training and mentoring program was implementedthrough four primary activities with the objective to educate and mentor staff in the 12 participating laboratoriestowards implementing a LQMS in compliance with theISO 15189 standard. These included:1 Design and implementation of laboratory audits anddevelopment of action plans with laboratories;2 Development and implementation of a formal LQMScurriculum and practical application training in situ;3 In situ mentoring of laboratory staff;
Ong et al. Hum Resour Health(2020) 18:844 Remote training sessions and mentoring throughvideo conferencing technologies.Design and implementation of laboratory auditsand development of action plans with laboratoriesIn support of a MoH initiative to establish an improvednational regulatory process over laboratory quality performance, this program provided training for 12 laboratory staff from participating laboratories to becomeprofessional LQMS auditors. This auditor trainingprogram was conducted over a period of 4 weeks viatele-conferencing and focused on LQMS principles,emphasizing ISO 15189 requirements (four power-pointpresentations with Khmer translation) and practice (eachauditor trainee performed an audit independently usingthe CamLQMS checklist under the supervision of experienced auditors). The CamLQMS tool was utilized bythe audit team to conduct baseline and exit audits of eachlaboratory participating in the program. The elements ofthe CamLQMS checklist specified national standards forLQMS conformity based on ISO 15189 and the Clinicaland Laboratory Standard Institute (CLSI) QMS01-A4guideline [12]. The checklist was divided into 12 sections organized by laboratory practice area and each section containing a series of quantifiable “yes”, “no” or “notapplicable” questions to assess whether conformity wasachieved. Numerical scores were derived for each sectionas well as overall performance. Laboratory audits wereperformed by teams of 4–5, consisting of members fromI-TECH, the MoH-BMLS and at least one auditor trainee.Baseline audits were conducted in 2017 and identifiedareas of LQMS performance that were commonly lowbetween the 12 participating laboratories. These resultswere discussed during a workshop with management andtechnical staff from the 12 laboratories in February 2018and action plans developed. Program mentors trainedparticipants to develop SMART (specific, measurable,achievable, realistic, and timely) [13] goals and actionplans to address the gaps identified in the audits. Participants developed action plans collaboratively with peers,presenting implementation strategies and soliciting feedback from peer laboratories and quality improvement(QI) specialists. Following a 12-month period of laboratory-based QI work, staff training, and mentoring, auditswere conducted again in 2019 to measure progress.Development and implementation of a formal LQMScurriculum and practical application training in situInformation obtained during the audit process informedthe development of a competency-based training curriculum for laboratory managers, quality assurance officers(QAOs), and other QI personnel in the laboratory, withPage 3 of 9training sessions implemented from resulting series of“off-site” and in situ workshops between February 2018and April 2019. Four off-site workshops were conductedin Phnom Penh and were primarily focused on deliveringLQMS and organizational leadership and managementtheory. These workshops used adult-learning strategies toengage participation and discussion, including dynamicsimulation, experiential learning, peer collaboration, andtransformative learning through problem solving. In situsessions were designed for staff to apply LQMS theoryusing hands-on skills. Each training session included acombination of formal lectures by quality experts, peerdiscussion, case presentation and reflection, and experiential practice [14]. All training sessions were conductedin English and translated into Khmer by QI mentors orprofessional translators to ensure comprehension amongnon-English speaking participants. In addition, a limitedparticipant study tour to ISO 15189 accredited laboratories in Singapore was provided as an advanced learningopportunity for high performing laboratories, whichmotivated healthy competition among participants tocomplete action plan items to attend.In situ mentoring of laboratory staffA team of four Cambodian QI mentors conducted regular site visits to laboratories for individual consultationswith each visit designed to guide, support, and engageparticipants in QI efforts by: Providing one-on-one follow-up training with laboratories; Ensuring accountability of laboratory managementand quality assurance personnel to action plans; Providing on-site technical guidance and collaboration to identify and resolve problems.Mentors were dispatched a minimum of four times toeach laboratory with laboratory specific TA and mentoring following workshops.Remote training sessions and mentoring through videoconferencing technologiesThe program’s tele-mentoring approach was modeled onsuccessful clinical mentoring programs such as ProjectECHO and used a similar “hub and spoke” structuredformat to advance knowledge and skills of laboratorystaff [15]. Zoom (Zoom Video Communications, Inc.,San Jose, California), a web-based video conferencing tool, was selected specifically for its low technical complexity, accessibility in low bandwidth settings,ability to connect multiple participants, video-recording and archiving features, and its screen sharing andremote desktop access functions. Mentors used Zoom
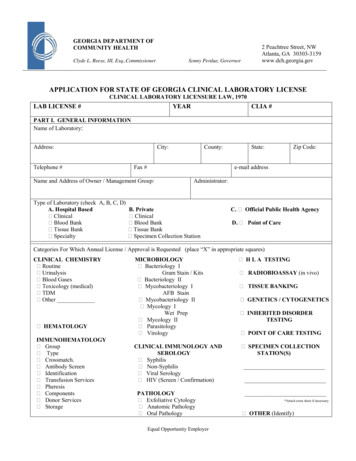
Ong et al. Hum Resour Health(2020) 18:84Page 4 of 9to connect with laboratory managers and QAOs duringweekly group trainings to reinforce formal training andto support ongoing action plans with troubleshootingassistance. Small group and individual meetings betweenmentors and participants were also conducted on an asneeded basis. SMS communications were also utilized byQI mentors to connect with staff and answer questionsin an ad hoc and individualized manner. Group SMSforums were established to advance group discussionbetween weekly Zoom sessions and enabled real-time enmasse communication.Evaluation methodologyWe used Likert scale survey responses to quantitativelyassess participant ratings of the program’s primary activities on a scale of 1–5, then used qualitative observationand participant feedback to develop and present a modelof best practices related to the program’s methodology,specifically identifying factors within the four primaryprogram activities that likely facilitated or hindered theprogram’s success. Quantitative and qualitative data toassess best practices were collected primarily through aprogram evaluation survey, which assessed participantfeedback after the program’s implementation with acombination of Likert scale and free response questions;these surveys were dispersed via email link to an onlinesurvey platform. The survey consisted of five statementsregarding the program’s activities to improve LQMS systems in participating laboratories, which participantswere prompted to rate their agreement with on a scale of1–5 ranging from strongly disagree to strongly agree andexplain their answers with written feedback. Participantsconsisted of laboratory managers, QAOs, and other quality assurance staff.Additional qualitative data were collected from trainingspecific, paper-based evaluations, which were carried outimmediately after each individual training and expandedto include other training participants such as hospital andlaboratory directors Post-training evaluations includedopen-ended prompts for feedback, which were recordedin a master spreadsheet by project staff, who translatedcomments from Khmer to English where necessary forqualitative analysis.To analyze survey data, mean Likert scale ratings andresponse frequencies of each response were calculatedto comparatively assess how well each program activity was perceived to contribute to QI within participantlaboratories. Participant feedback was analyzed by acombination of inductive and deductive analysis. Prior toanalysis of participant feedback, we compiled a hypothesized model of best practices within each of the primaryprogram activities that contributed to program outcomesaccording to observation. We then analyzed feedbackfrom surveys to corroborate and expand on this initial setof themes, categorizing text from participant commentsinto the relevant themes and inductively identifying new,previously unidentified themes recurring within the text.Using spreadsheets to organize and filter participantcomments, each response was sorted according to theevaluation source and activity in question, then categorized into themes. Occurrence frequencies of each themewere tallied, analyzed, and then summarized.ResultsOut of a total of 28 participants who were sent the program evaluation survey, 27 (96%) responded. Resultsdemonstrated that participants agreed most highly thatin-person mentoring and CamLQMS audits were valuable (means 4.56 and 4.52, respectively), receiving thehighest frequencies of “strongly agree” ratings and thehighest mean ratings (Table 1). Conversely, participantsagreed least with the statement that Zoom-based training and question/answer sessions were valuable to QI(mean 3.44). Participants agreed moderately, however,with the statement that the overall program structurewas effective in their laboratories’ improvement processes (mean 4.11).Table 1 Frequency distributions, total responses, and mean ratings of program evaluation survey responsesSurvey categoryFrequency (no.) of responses counted12345StronglydisagreeDisagreeNeither agreenor disagreeAgreeStronglyagreeTotal responsesMean ratingCamLQMS action planning was valuable0001314274.52Formal training was valuable001197274.22In-person mentoring was valuable0001215274.56Zoom call check-ins were valuable324162273.44Overall program structure was effective102168274.11
Ong et al. Hum Resour Health(2020) 18:84Page 5 of 9Observations and qualitative analysis uncovered 23themes regarding best practices, 21 of which were supported by participant feedback. We analyzed 239 individual comments from training evaluations and anadditional 39 textual responses from program evaluationsurveys. Responses from participants were brief, rangingfrom 1–68 words in length (median 13). From these,we identified 147 instances of positive feedback and 99instances of constructive critique for improvement, fromwhich 123 comments either corroborated best practicethemes or introduced novel themes according to theassociated primary activity supported (Fig. 1).Best practices of laboratory assessments and actionplanningParticipant feedback indicated the “useful” role of theCamLQMS assessments in their QI progress, which provided a clear entry point for the continuous QI cycle, enabling participants to identify gaps and develop SMARTaction plans to address deficiencies. As one participantsummarized: “Plans action results follow-up—Thoseprocess [sic] help to improve my lab quality”. Although notcorroborated by participant feedback, we also observeda clear benefit to participants from immediate feedbackand corrective action by auditors during audits, and fromauditors engaging the attention of both hospital leadership and government stakeholders.The audit training program as well was observed tosuccessfully engage selected laboratory staff in the auditprocess while supporting the MoH initiative to provide trained personnel for regulatory LQMS oversightand auditing. While a separate study would be requiredto compile and analyze feedback from these additionaltrainings, improved audit training is a recommended bestpractice to assure quality metrics.Best practices of in situ training58 comments indicated improved learning due to practical training sessions, 22 of which referred to specificcurriculum such as management review and equipmentvalidation as being helpful. Additionally, peer learningand collaboration was remarked highly by participants,who often requested more peer learning activities whereparticipants of different labs could share ideas and experiences, learning from each other and collaborating totroubleshoot and solve practical QI challenges. “Everyparticipant should raise, share, [sic] talk about experience”, as one participant suggested.Participants expressed considerable preference forin situ training activities, mentioning specifically thepractical and experiential learning as important forparticipant improvement: “This on-site lab training isso important, because we can practice directly and getnew experience and skill”. One of the key benefits to theLaboratory audits and action plan development1. Audits identify systemgaps to focus actions onurgent needs first (4)2. Audits provide immediatefeedback for laboratories toact on (0)3. Audits engage laboratoryleadership and governmentstakeholders (0)4. Participant action plansdrive improvement (3)5. Training auditors fromlaboratories prepareslaboratories and buildsnational capacity (0)Formal LQMS curriculum and in-situ trainingIn-situ mentoring of laboratory staff1. Provides focusedknowledge through needsbased training (22)2. Promotes peer learningthrough collaboration andexperience sharing (14)3. Emphasizes on-sitelearning with hands onexperience (15)4. Motivates with aninteractive and dynamicadult learning strategy (11)5. Provides advancedlearning opportunities (2)6. Motivates throughemphasis on patient careand safety(1)7. Best when conducted inlocal language (20)1. Visits purposefullycomplement and build onformal training (2)2. Promotes participantaccountability to goals andaction plans (2)3. Promotes in-personcollaboration to identify andsolve problems (7)4. Builds mentor/menteeprofessional relationship (1)5. Facilitates engagementof leadership and Ministryof Health (1)Remote tele-mentoring1. Complements formalcurriculum (3)2. Regular check-inspromote accountability andengagement (1)3. Promotes continued peerlearning and collaboration (5)4. Regular availability forquestions and feedback (2)5. Cost-effective alternativeto on-site visits (1)6. Best when conducted inlocal language (1)7. Group tele-mentoring isbest when well structured tomanage time and preventdistraction (5)8. Requires adequateinternet connectivity andtechnical capacity oflaboratories (1)Outcomes:Improvedknowledge ofqualityimprovementand capacityfor qualitymanagementImprovedcompliance toISO 15189standardsImprovedqualityFig. 1 Model of best practice themes and the relationship of program activities to program outcomes. Numbers in parenthesis represent thenumber of participant comments that support each best practice theory.
Ong et al. Hum Resour Health(2020) 18:84in situ method was the advanced training and improvement opportunity that it gave to higher performing laboratories, which had the opportunity to present theirown quality management systems for critical observation by their peer participants from other laboratories.Lower performing laboratories, meanwhile, were able tolearn from the best practices of their peers. This practiceaddressed the need to match training content to benefitall ranges of participant experience. Participants werealso able to acquire practical skills through direct handson participation during the experience. “I think practiceis better than theory”, one participant suggested.Finally, although our trainers strived to conduct alltraining in the local language wherever possible as a bestpractice, feedback from participants expressed strongcritique for translators when information was not translated clearly enough. It was apparent that the trainingcurriculum required further strengthening to meet thelanguage needs of participants.Best practices of in situ mentoringParticipant feedback indicated strong value for faceto-face in situ mentoring and appreciated follow-upprovided regarding QI plans and holding participantsaccountable. Participants appreciated the problem-solving suggestions of mentors, identifying and discussingproblems on-site with participants and collaborating toovercome challenges to improvement. One participantcommented: “Mentor can see real situation in my lab andcan suggest and help initiate my lab team to do something according to the gap.” Participants also suggestedthat face-to-face visits from mentors served to improvethe professional mentor–mentee working relationship,and further comments remarked that mentor visits hadhelped engage other important stakeholders such ashospital directors and MoH regulators in laboratory QI.One participant addressed both factors, stating “Regularperiodic visits from trainers is important because it makesan important connection between the training instituteand the laboratory staff. An in-person trainer visit is alsoimportant to increase the credibility of the laboratory staffto the laboratory director.” When mentors visit laboratories, MoH personnel and laboratory directors are invitedto meet with mentors and QAO to discuss current andpast improvement efforts, garnering support for laboratory improvement efforts; this engagement of leadershipis critical.Best practices of tele‑mentoringA concurrent study of audit results found a significantcorrelation between participation time spent in Zoomtele-conferencing and laboratory QI [11]; however, participants in our study ranked Zoom tele-conferencingPage 6 of 9lower than all other program activities. Participants werecritical of large group tele-conferencing activities in particular, stating “too much talk with a lot of peoples [sic],difficult to take experience”, “talk for everything”, and “participants not [sic] pay attention during zoom call.” Thisfeedback suggests that improved facilitation structureand efficiency of video conferencing may be a best practice to improve the learning experience of participants, solong as the opportunity for peer learning is not sacrificed.Another concern observed and heard from participants throughout the program, though surprisingly onlyaddressed once through written feedback, is the challenge of unstable internet connections, which oftendecreased meeting productivity. In some locations,user desktop computers lacked a camera or webcam,which inhibited interactive participation. Assessing andimproving technical capacity and internet connectivityshould therefore be a necessary component of telementor program planning. Despite these challenges, participants noted improved knowledge from tele-mentoringsessions, appreciated regular feedback from mentors, andagain praised the ability to collaborate with both peersand mentors, sharing experience and knowledge. Participants further praised the real-time access to QI mentors being able to ask questions and receive a responseimmediately, which was an important best practice ofthe mentors, who set regular open hours for participantsto call for guidance. Training in the local language wasonce again a strong request from participants, and onecomment noted the cost effectiveness of tele-mentoring,saving participants time and money required for travel.In addition to participant feedback, several strategies toaddress these challenges are recommended (Table 2).DiscussionAs demonstrated by measurable improvements in CamLQMS audit scores at the 12 laboratories, this training and mentoring approach made a positive impactin Cambodia and correlates with similar reports in theregion [11, 16]. We found evidence that regular laboratory mentoring, supported by needs-based training andinter-laboratory collaboration enhances laboratory QIwhen it emphasizes actionable needs-based planning,peer learning in a practical and supportive environment,and collaborative problem solving. It was evident in theimplementation of our program that customizing thementoring and training program for the local environment is more effective than a preconceived one size fitsall approach, and that taking an adaptive approach toteaching practice-based skills is critical for rapid QI [17].Our program was designed specifically to utilizepeer learning among a set of other dynamic, hands-on,and interactive adult-learning strategies implemented
Laboratories should ensure access to a desktop computer withsound, microphone, and webcamAcquire and use quality headphones with built in microphonewhenever possibleUse smartphone (personal or institution-based) if necessaryLack of appropriate computer hardware or equipment such asa microphone and webcam reduces ability of attendees toparticipateAssess hardware capacity (audio-visual functionality) of participantsAddress access barriers: identify funding or resources for equipment, provide phone/data cards for participantsAssess participant technical challenges prior to meeting andprovide guidance or resourcesProvide list of common troubleshooting suggestions prior tomeetingIn cases of regular electrical shortages, check with national electricity supply board or monitor public notifications for potentialoutagesIdentify a stable internet connectionEnsure that a back-up internet and/or power connection isavailableUse a mobile phone if it is a better option and does not incurextra costs on participantsTest connectivity prior to meetingUnstable internet or electricity resulted in frequent droppedparticipants and interruptionRecommended strategies for facilitatorsDo not assume competence; provide initial training on how toeffectively use video conference platformEstablish ground rules and group norms such as
ples of diagnostic testing and quality assurance practices required to carry out testing procedures with repeatable accuracy [7]. In 2016, the rst joint external evaluation was con-ducted to measure Cambodia's achievements towards meeting the International Health Regulations. is revealed gaps in the areas of LQMS and workforce capac-