Transcription
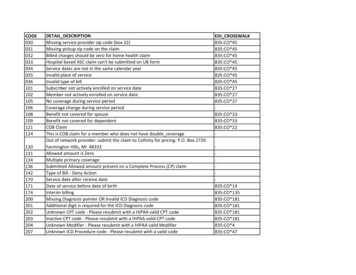
30131134136142170171174200201202203204207DETAIL DESCRIPTIONMissing service provider zip code (box 32)Missing pickup zip code on the claimBilled charges should be zero for home health claimHospital based ASC claim can't be submitted on UB formService dates are not in the same calendar yearInvalid place of serviceInvalid type of billSubscriber not actively enrolled on service dateMember not actively enrolled on service dateNo coverage during service periodCoverage change during service periodBenefit not covered for spouseBenefit not covered for dependentCOB ClaimThis is COB claim for a member who does not have double coverageOut of network provider: submit the claim to Cofinity for pricing. P.O. Box 2720Farmington Hills, MI 48333Allowed amount is ZeroMultiple primary coverageSubmitted Allowed amount present on a Complete Process (CP) claimType of Bill - Deny ActionService date after receive dateDate of service before date of birthInterim billingMissing Diagnosis pointer OR Invalid ICD Diagnosis codeAdditional digit is required for the ICD Diagnosis codeUnknown CPT code - Please resubmit with a HIPAA valid CPT codeInactive CPT code - Please resubmit with a HIPAA valid CPT codeUnknown Modifier - Please resubmit with a HIPAA valid ModifierUnknown ICD Procedure code - Please resubmit with a valid codeEDI 47
215Missing Admission source for the Revenue code submitted, for NONPPO provider -216217223231232233243244245270Invalid Value Codes for the Revenue codes submitted, for NONPPO providerHOST claim cannot be submitted with zero total chargesReferring provider NPI is missing in Ancillary claim.Current claim falls within the history claim date rangeCurrent claim falls outside the history claim date rangeUnknown Secondary ICD Diagnosis CodeInvalid Diagnosis CodeInvalid Secondary Diagnosis CodeInvalid Procedure codeAuthorization is required for this serviceNo proper auth has been obtain by provider or member, copayment amount incase oApplied benefit per authorized network-Applied benefits per authorized network. Missing auth network on line(s)Not enough money in the COB Savings to pay member obligationClaim submitted with ICD9 Diagnosis codes. Please re-submit claim with ICD10Diagnosis codes.Claim submitted with ICD10 Diagnosis codes. Please re-submit claim with ICD9Diagnosis codesUnlisted code - Please resubmit using a more specific code and/or a description ofcodePayment Reduced by Deductible AmountA copayment has been applied to this serviceA coinsurance has been applied to this serviceMember in HospiceReduced paid by percent allowed after out of pocket is metPayment adjusted based on modifier submittedAdditional digit is required for the Secondary ICD Diagnosis 35:CO*45-
8339340342343344345346348350351352357361362Family Deductible limit is metReduced paid by provider withholdReduced allowed by Subro amountNumber of visit per year exceed max, reduced visitsNumber of visits exceeded max, reduced visitsApplied copay balanceUnable to take balance copayThere is no paid amount after applied copay balanceRecalculated allowed amountReduced Amount BY MAX AllowedIndividual out of pocket limit for benefit year is metCopay has already been taken for this visit.Family lifetime max limit is metFamily out of pocket limit for benefit year is metIndividual lifetime out of pocket limit is metFamily lifetime out of pocket limit is metNumber of copayment met.Reduced number of copaysAlternate HHRG Code and anticipate payment is available. Check Report fordetailsIndividual Deductible limit is metExceeded max allowed amount for claimMember annual allowed amount exceeded maxAnnual allowed amount for ben cat exceeds max.Member lifetime allowed amount exceeded maxFamily annual allowed amount exceeded maxIndividual life max for benefit category exceeded maxFamily life max for benefit category exceededFamily annual allowed amount for benefit category exceeded maxMember age excludes benefit coverageStudent age limitation in this planMissing COBRA 5835:CO*B5-
364Performed service is not part of contract which will be paid under global fee co-365366This service is still within days after from range in this global fee contract,Global fee accumulator has been updated with a new event 394395396397398399406407410411414Remaining portion will not be paid, since this is max amount which can be coveredSubscriber enrolled in Cobra, will keep his or her ID.Billed charges paid by MemberPaid amount on the replacement claim is less than the backed-out claimSubmitted DRG not same as the Calculated DRGVoid ClaimStandard Medicaid Fee ScheduleFee schedule is not activePossible COBPossible COB - Multiple CoverageHCFA / Outpatient per case contract with providerUB per line item contract with providerPayment is fee schedule basedPercent billed contract with providerCapitation contract with providerGlobal fee contract with providerPayment Based on Per Diem RateInpatient Per admit contract with providerGrouper contract with providerDRG contract with provider requires DRG code be present on UB92 formHCFA payment by service code per day/claimAdd NDC AWP paymentCode not in Fee Schedule.Not paid because of capitation contractLower allowed amount by Rebundler percentageAllowed amount reduced because of multiple ASC surgery 5:CO*47835:CO*45835:CO*45835:CO*24835:CO*45
1512528529530531533538539540600601602604Additional charges have been applied.Paid by additional charges.Schedule amount exceed Billed amount; Pay billed amount.Additional charges charges will not be paid since the total allowable amount isgreater than bill amount.Zip code requires carrier and localityApplied Combined Par Network benefitsPreexisting conditionsAuthorization not foundAuthorization given to different memberAuthorization has been deniedDenied by RebundlerNew Line ItemDuplicate Line ItemAssistant Surgeon limit exceeded for this procedurereduced paid according to rebundler ruleRider Option selectedRider Option - Number of visits exceeds allowableReduced paid by discount amountAge is out of range for the given Primary DiagnosisGender is invalid for the given Primary Diagnosis.Age is out of range for the given codeGender code is invalid for the given CPTMODIFIER NOT CONSIDERED ELIGIBLE BY SIGNATURE CARE - PROV W/OStop Loss amount reachedClaim being denied over filing limitTotal charges not equal to total charges of line itemsManual overwriteManual PaymentManual DeniedInjectable/infusion/Pathology/Lab code requires prior approval by the *45835:OA*216835:CO*197
621623624Inappropriate Coding or Claim FormPrimary Carrier EOB Required or proof of termination of Primary carrierNot A Covered BenefitDenied - No Medical CoverageDenied - No Dental CoverageDenied - No Vision CoverageDuplicate ClaimEligibility Documentation Required (i.e., Birth Certificate, Marriage License,Divorce Decree)Exceeds filing limit - Can Not Bill PatientInvestigating Other Insurance For COB or MVA.Denied Incidental ProcedureInvalid/Deleted Diagnosis CodeInvalid/Deleted Procedure CodeMedical Records Must Be Submitted.Other Insurance Information RequiredPart of global code or Procedure is within the global period or procedureperformed by the same providerPrior/After UR Authorized DatesDenied - Over Plan Filing Limit625626627628629630631632633634Unlisted Procedure - Submit specific CPT/HCPCS or detailed description of servicerequired in comment field and Documentation of Medical NecessityNot A Billable Service By This ProviderAn established patient E/M code should have been used.Denied-Service Exceeds Plan LimitCharges Incurred After Term DateDuplicate Line ItemClaim Exceeds Authorized VisitsDenied -No UR Authorization/Authorization not approvedDiagnosis Does Not Match Authorized DiagnosisPenalty - No Out Of Network CO*197835:CO*197835:CO*197
1652653654655656657658659660661662Inappropriate Place Of Service BilledItemized Statement RequiredDenied Related To Workmans CompProvider Not Properly CredentialedPaid or Processed as SecondaryCharges Incurred Prior To Effective DateRequested Information ReceivedRequire Copy Of Operative ReportPending For Medicare Effective DateAge Is Out Of Range For Given CPTIncorrect Patient DemographicsRequire Attending Physicians Name-field 31 and/or NPI in field 24JDenied Requested Information Not ReceivedRequired Description of Primary's Remark CodesDenied-Exceeds allowed quantity or frequencyDenied-Submit to Community Mental Health. Inpatient behavioral services are acarve out for Medicaid beneficiaries.Allowable Applied to the DeductibleThis Is A PredeterminationDual eligible enrollee-Eligible for, not enrolled in d - Subsequent PT/OT/ST visits must be authorized by Navant 734/995-1969Submit Original Primary EOBMaximum Pay Amount. Patient Owes BalanceResubmit With Anesthesia Code/ModifierDenied-Present on Admission Indicator Required, information may be missing orinvalid.Exceeds Yearly Dental MaximumPrimary diagnosis code not recognized by this DRG Grouper. Please map diagnosisto the prev. versioDenied-Missing Multiple Surgical ModifierServices not provided by a designated or contracted :CO*4835:CO*164
663664665666No Secondary Consideration Until Primary's Request SatisfiedRequire Primary Carrier's EOBAdditional PaymentSplit Claim Needed for Non Covered Charges667668Denied-Require facility name and address where services were rendered, box 32 835:OA*16EOB and Claim Do Not Match835:CO*22Denied - The immunization must be billed with the immunization administrationcode.835:CO*234Forward claim to Psychcare 1-800-221-5487835:CO*16Denied-Submit claim to Beacon Health Options - PO Box 1854 Hicksville, NY 118021854835:CO*24Not Included In Case Rate835:CO*45Resubmit- illegible EOB835:CO*22Split Payment Due To Benefits835:CO*16Denied - Replacement/void claim received835:CO*18Require Copy of Birth Certificate835:CO*177Require eligibility verification form835:CO*177Send medical records to: PO Box 27476, Salt Lake City, UT 84127-0476, fax866/503-8239835:OA*133Submit Claim to Occupational Eyewear Network at 3824 Thirteen Mile Rd, Warren,MI 48092- ATTN:Total835:CO*24Claim not submitted with contracted TIN/ NPI/ payee information835:CO*16Paid per settlement835:CO*177Service line pending fee schedule/pricer update. Payment to be adjusted when feeavailable.835:CO*16Non-Network/InActive Provider/Non-contracted Physician835:OA*242Denied by Medical Director after Review835:CO*45Covered In Contracted Case Rate835:CO*45Per primary carrier EOB, This is a provider write-off835:CO*45Denied-Exceeds annual maximum benefit 35:CO*16
ssion of a claim under review or previously denied by TC3/CHANGEHEALTH CARESubmit Claim to Cofinity for PricingDx code not listed in the Emergency Transport Diagnosis Code DatabaseNot a THC Enrollee/Incorrect Member/ClaimantResubmit with a THC referralResubmit with Prenatal DatesINVALID PLACE OF SERVICENot covered by Medicaid/ MedicareService includedPreviously paidCharges are covered under a capitation agreementService is not authorized on the referral or authorizationPayment applied to plan deductibleNumber of visit exceeds annual allowableAdjust Allowed amount to amount per visit max.Claim exceeds days since accident (EOB)Claim exceed EOB max pay amountPayment is according EOB formulaBenefit reduced by plan deductibleMissing accident date for accident related claimClaim had been paid at header levelThis visit has been paid.Minimum % OF billed applied.Exceed maximum allowed time for pended claim - DeniedApplied Header level Add-on AmountApplied iCES editsDenied based on iCES editsApplied percent reduction as per ICESDenied based on pricing reductionBenefit Payment Copay Order (Deductible/Copay)Benefit Payment Copay Order CO*18835:CO*216-
91191291300L00V00Z01G01Z02I02J02Z03Z04ZChange description later - PCP logicPay according to Professional general contractPay according to PCP contractNo errors foundNo errors found For hss ProfessionalPricer - No errorsGROUPER - CODE IS INVALID, OR NOT VALID FOR SERVICE DATEPricer - No available APC/fee schedule rateNo HIPPS code on claimNo HIPPS code on the claimPricer - Invalid HCPCS codePricer - Invalid payment statusNot Covered Under OPPS835:CO*204-07Q08Z09Z10ZNo DRG weights/rates (for Illinois Medicaid, Nebraska Medicaid, New York Legacy,and Ohio Medicaid also see Chapter 5 of EASYGroup¿ DRG Pricer User Guide)Pricer - Invalid modifier for pricingPricer - Packaged servicePricer - Line item denial or rejection from ACE/ write off835:CO*97-13Z16H21Q22P23P24Q27G28Z35ZPricer - ZIP code missing or invalid, for ambulance fee schedule service onlyConflicting birthweight as derived from diagnosis codes or birthweight in gramsconflicts with birthweight diagnosis codesPresent on Admission Indicator Required/InvalidDenial claimInvalid service date, from-thru dates,or admission dateNon-covered claim (Kentucky Medicaid, Virginia Medicaid, and MedicareInpatient)Invalid or no Treatment Authorization codeNo available extended fee schedule rateThis is a quality measurement code used for reporting purposes only.-
7E08E09E10E11E12E13E14E15E16Incorrect billing of Automated Multi-Channel Chemistry (AMCC) ESRDrelated tests. Invalid or Missing Required Claims Data835:CO*16Invalid billing of therapy servicesNewborn claims that do not contain an UB-04 Value Code of 54 with the birthweight in the UB-04 Value Amount field will be issued this Pricer Return Code.Closed or inactive rate recordAuthorization Class does not matchAuthorization - LOS does not matchAuthorization - unit exceededCopayment paid per service dayVisit falls before the event period.Misrepresentation of DiagnosisFailure by referring provider to comply with investigative requestsFailure by rendering provider to comply with investigative requestsDenied - Unbundled Service/Exclusive or Incidental Relationship.Deliberate performance of unwarranted servicesBilling for services/supplies not providedMisrepresentation of services/supplies providedTreatment is not in accordance with standard of careNo documentation in medical record of services billed, medical record does notsupport billed service.Auto insurance primaryPrimary payment exceeds allowableHCPCS Code RequiredTHC primary carrierDenied- NDC Code Required in HCFA box 24 or in UB service line area per MSABulletin 10-26Denied-Invalid/ missing or incorrect ModifierDenied- NDC is invalid for the billed service 835:OA*4835:OA*206
E17E18E19E20E21Denied- Electronic Referral Required, refer d.pdfInjection is covered under Medicare Part D. Contact Catamaran at 855-348-3231for direction on filinInjection pending Part D filing submissionDenied-No history of inpatient services or observation provided for TransitionalCare Management ServicesDenied - DOS is outside of the required 5:OA*96835:CO*16E34Denied- Date of visits and EDC required in field 19 or appropriate EDI loopDenied - Prenatal global billing must be rebilled as separate services and includeDOS and EDCDenied by Medicare/Primary InsurerMultiple procedure reduction of 50% applied per CMS guidelinesDenied- Services not supported by patient history or documentation.Denied- No additional payment, no cost sharing applied by Medicare/ primaryinsurerDenied-Awaiting eligibility determination from health insurance marketplace dueto non-payment of premium.Resubmission of a claim under review by TC3/CHANGE HEALTH CARESend medical records to:5720 Smetana Drive, Suite 400, Minnetonka, MN 55343.FAX: 952-949-3713Denied- Medicare is primary, EOB is required.Denied- Left against medical advice- not a covered benefitDenied-The requisition form was not signed by the ordering physician.Denied- Inappropriate use of Modifier -59. According to CCI data, there are notany CCI conflicts for this code.E35E40Denied - Does not meet inpatient hospital claim requirements for newbornsPayment requires submission of completed HRA- fax to 22835:CO*204835:CO*16835:OA*4
E41E42E44Denied - Diagnosis describes an external cause, or requires the ICD code for thefirst underlying disease, and should never be listed as the primary diagnosis for aprocedure.835:CO*146service or supply may be considered investigational and experimental835:CO*55Denied- Drug code requires name of drug, dosage, and NDC of the drug furnishedin comment 2Processed as Secondary Contractual Obligation or No Primary Member Obligation.Processed as secondary - capitated service - no additional paymentDenied- Psychotropic injectable carve-out drugs reimbursable by MDCHDenied-Send Itemized Statement to: Equian, 300 Union Blvd., Ste 200, Lakewood,CO 80228. Fax 800-435-2049Charges denied by Equian due to identification of clean claim issuesCharges Pended by Equian due to identification of clean claim issuesInformational- Paid in accordance to Equian recommendationClaim forwarded to Equian for forensic reviewDenied - Service included in Mendelson Bundle ProjectInformational - Paid in accordance to Mendelson Bundle ProjectInformational- Coordination of Benefits THC PrimaryInformational-Reduction of 25% applied per CMS guidelinesInformational-Multiple Endoscopy payment reductionDenied-Per the ICD-10-CM Excludes note guideline, diagnosis codes identify twoconditions that cannot be reported togetherDenied- Diagnosis and Modifier combination are inappropriateDenied- Principal procedure code is invalidDenied-Federal Health Care Programs are prohibited from paying for services byHHS-OIG excluded provider or physiciansDenied-ICD procedure code is non-coveredE63E64Informational - Processed as secondary, service not covered by primary carrier.D-Submitted to First Health for 1835:CO*181835:CO*181
E67Informational- The presence of modifier 54, 55, or 56 indicates that only the preop, intraoperative, or post-op portion of the global fee should be reimbursed.835:CO*59Denied - Discrepancy detected between the number of units on this claim line andthe difference between the Beginning DOS and the Ending DOS. Documentationdoes not support billed units.835:CO*16Denied-visit is the same day as a procedure with a status indicator of T or Swithout modifier 25835:OA*4E68E69E70Denied - The primary procedure code that is associated with this add-onprocedure code has received a denied status. Please review billing procedures.Denied - Check Refund Adjustment ClaimInformational- Paid in accordance to VARIS pdated 11/28/2017
Missing auth network on line(s) - 278 Not enough money in the COB Savings to pay member obligation - 286 Claim submitted with ICD9 Diagnosis codes. Please re-submit claim with ICD10 . 640 Charges Incurred Prior To Effective Date 835:CO*26 641 Requested Information Received 835:CO*45 642 Require Copy Of Operative Report 835:CO*16