Transcription
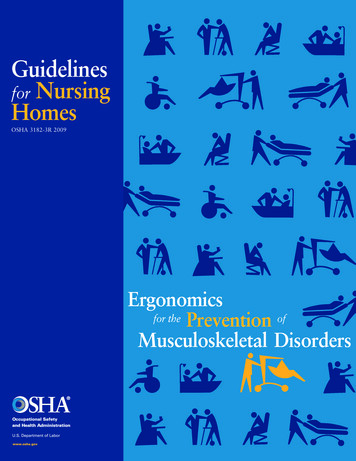
Guidelinesfor NursingHomesOSHA 3182-3R 2009Ergonomicsfor the Prevention ofMusculoskeletal Disorders
Guidelines for Nursing HomesErgonomics for the Preventionof Musculoskeletal DisordersU.S. Department of LaborElaine L. Chao, SecretaryOccupational Safety and Health AdministrationJohn L. Henshaw, Assistant SecretaryOSHA 3182-3R 2009Guidelines for Nursing Homes1
2Guidelines for Nursing Homes
Table of Contents5Executive Summary7SECTION I:Introduction9SECTION II:A Process for Protecting Workers99101010111112Provide Management SupportInvolve EmployeesIdentify ProblemsImplement SolutionsAddress Reports of InjuriesProvide TrainingEvaluate Ergonomics EffortsSECTION III:Identifying Problems and Implementing Solutions for ResidentLifting and Repositioning12Identifying Problems for Resident Lifting and Repositioning Figure 1. Transfer to and from: Bed to Chair, Chair to Toilet,Chair to Chair, or Car to Chair17 Figure 2. Lateral Transfer to and from: Bed to Stretcher, Trolley Figure 3. Transfer to and from: Chair to Stretcher Figure 4. Reposition in Bed: Side-to-Side, Up in Bed Figure 5. Reposition in Chair: Wheelchair and Dependency Chair Figure 6. Transfer a Patient Up From the FloorImplementing Solutions for Resident Lifting and Repositioning Transfer from Sitting to Standing Position Resident Lifting Repositioning in Chair Ambulation Lateral Transfer; Repositioning Lateral Transfer in Sitting Position Transfer from Sitting to Standing Position Weighing Transfer from Sitting to Standing Position; Ambulation Repositioning Bathtub, Shower, and Toileting ActivitiesGuidelines for Nursing Homes3
Table of Contents27SECTION IV:Identifying Problems and Implementing Solutions forActivities Other than Resident Lifting and Repositioning31 Storage and Transfer of Food, Supplies, and Medications Mobile Medical Equipment Working with Liquids in Housekeeping Working with Liquids in Kitchens Hand Tools Linen Carts Handling Bags Reaching into Sink Loading or Unloading Laundry Cleaning Rooms (Wet Method) Cleaning Rooms (Electrical)SECTION V:Training31313133Nursing Assistants and Other Workers at Risk of InjuryTraining for Charge Nurses and SupervisorsTraining for Designated Program ManagersSECTION VI:Additional Sources of Information35364ReferencesAppendix: A Nursing Home Case StudyGuidelines for Nursing Homes
Executive SummaryThese guidelines providerecommendations for nursing homeemployers to help reduce the numberand severity of work-related musculoskeletal disorders (MSDs) in theirfacilities. MSDs include conditionssuch as low back pain, sciatica,rotator cuff injuries, epicondylitis,and carpal tunnel syndrome. Therecommendations in these guidelinesare based on a review of existingpractices and programs, State OSHAprograms, as well as availablescientific information, and reflectcomments received from representativesof trade and professional associations,labor organizations, the medicalcommunity, individual firms,and other interested parties. OSHAthanks the many organizationsand individuals involved for theirthoughtful comments, suggestions,and assistance.More remains to be learned aboutthe relationship between workplaceactivities and the development ofMSDs. However, OSHA believesthat the experiences of many nursinghomes provide a basis for takingaction to better protect workers.As the understanding of these injuriesdevelops and information andtechnology improve, the recommendations made in this document maybe modified.Although these guidelines aredesigned specifically for nursinghomes, OSHA hopes that employerswith similar work environments, suchas assisted living centers, homes forthe disabled, homes for the aged,and hospitals will also find thisinformation useful.OSHA also recognizes that smallemployers, in particular, may nothave the need for as comprehensive aprogram as would result fromimplementation of every action andstrategy described in these guidelines.Additionally, OSHA realizes thatmany small employers may needassistance in implementing anappropriate ergonomics program.That is why we emphasize theavailability of the free OSHAconsultation service for smalleremployers. The consultation service isindependent of OSHA’s enforcementactivity and will be making specialefforts to provide help to the nursinghome industry.These guidelines are advisory innature and informational in content.They are not a new standard orregulation and do not create any newOSHA duties. Under the OSH Act,the extent of an employer’s obligationto address ergonomic hazards isgoverned by the general duty clause,29 U.S.C. 654(a)(1).Guidelines for Nursing Homes5
Executive SummaryAn employer’s failure to implementthe guidelines is not a violation, orevidence of a violation, and may notbe used as evidence of a violation, ofthe general duty clause. Furthermore,the fact that OSHA has developedthis document is not evidence andmay not be used as evidence of anemployer’s obligations under thegeneral duty clause; the fact that ameasure is recommended in thisdocument but not adopted by anemployer is not evidence, and maynot be used as evidence, of aviolation of the general duty clause.In addition, the recommendationscontained herein should be adaptedto the needs and resources of eachindividual place of employment.Thus, implementation of the guidelines may differ from site to sitedepending on the circumstancesat each particular site.6Guidelines for Nursing HomesWhile specific measures maydiffer from site to site, OSHArecommends that: Manual lifting of residents beminimized in all cases andeliminated when feasible. Employers implement an effectiveergonomics process that: provides management support; involves employees; identifies problems; implements solutions; addresses reports of injuries; provides training; and evaluates ergonomics efforts.These guidelines elaborate onthese recommendations, and includeadditional information employerscan use to identify problems andtrain employees. Of particular valueare examples of solutions employerscan use to help reduce MSDs in theirworkplace. Recommended solutionsfor resident lifting and repositioningare found in Section III, whilerecommended solutions for otherergonomic concerns are in SectionIV. The appendix includes a casestudy describing the process onenursing home used to reduce MSDs.
SECTIONIIntroductionNursing homes that haveimplemented injury prevention effortsfocusing on resident lifting andrepositioning methods have achievedconsiderable success in reducingwork-related injuries and associatedworkers’ compensation costs. Providing a safer and more comfortablework environment has also resulted inadditional benefits for some facilities,including reduced staff turnover andassociated training and administrativecosts, reduced absenteeism, increasedproductivity, improved employeemorale, and increased residentcomfort. These guidelines providerecommendations for employers tohelp them reduce the number andseverity of work-related musculoskeletal disorders in their facilities usingmethods that have been found to besuccessful in the nursing homeenvironment.Providing care to nursing homeresidents is physically demandingwork. Nursing home residents oftenrequire assistance to walk, bathe, orperform other normal daily activities.In some cases residents are totallydependent upon caregivers formobility. Manual lifting and othertasks involving the repositioning ofresidents are associated with anincreased risk of pain and injury tocaregivers, particularly to the back (2,3). These tasks can entail high physicaldemands due to the large amountof weight involved, awkward posturesthat may result from leaning over abed or working in a confined area,shifting of weight that may occur if aresident loses balance or strengthwhile moving, and many otherfactors. The risk factors that workersin nursing homes face include: Force - the amount of physicaleffort required to perform a task(such as heavy lifting) or to maintain control of equipment or tools; Repetition - performing the samemotion or series of motions continually or frequently; and Awkward postures - assumingpositions that place stress on thebody, such as reaching aboveshoulder height, kneeling,squatting, leaning over a bed, ortwisting the torso while lifting (3).Wyandot County Nursing Home in UpperSandusky, Ohio, has implemented a policyof performing all assisted residenttransfers with mechanical lifts, and haspurchased electrically adjustable beds.According to Wyandot, no back injuriesfrom resident lifting have occurred in overfive years. The nursing home also reportedthat workers’ compensation costs havedeclined from an average of almost 140,000 per year to less than 4,000 peryear, reduced absenteeism and overtimehave resulted in annual savings ofapproximately 55,000, and a reduction incosts associated with staff turnover hassaved an additional 125,000 (1). (seeReference List)Guidelines for Nursing Homes7
IntroductionExcessive exposure to these riskfactors can result in a variety ofdisorders in affected workers (3, 5).These conditions are collectivelyreferred to as musculoskeletaldisorders, or MSDs. MSDs includeconditions such as low back pain,sciatica, rotator cuff injuries,epicondylitis, and carpal tunnelsyndrome (6). Early indications ofMSDs can include persistent pain,restriction of joint movement, or softtissue swelling (3, 7).While some MSDs develop gradually over time, others may resultfrom instantaneous events such as asingle heavy lift (3). Activities outsideof the workplace that involvesubstantial physical demands mayalso cause or contribute to MSDs (6).In addition, development of MSDsmay be related to genetic causes,gender, age, and other factors (5, 6).Finally, there is evidence that reportsof MSDs may be linked to certainpsychosocial factors such as jobdissatisfaction, monotonous work,and limited job control (5, 6). Theseguidelines address only physicalfactors in the workplace that arerelated to the development of MSDs.8Guidelines for Nursing HomesAfter implementing a program designedto eliminate manual lifting of residents,Schoellkopf Health Center in NiagaraFalls, New York, reported a downwardtrend in the number and severity ofinjuries, with lost workdays droppingfrom 364 to 52, light duty daysdropping from 253 to 25, and workers’compensation losses falling from 84,533 to 6,983 annually (4).At Citizens Memorial Health Care Facilityin Bolivar, Missouri, establishment of anergonomics component in the existingsafety and health program was reportedlyfollowed by a reduction in the number ofOSHA-recordable lifting-related injuries ofat least 45% during each of the next fouryears, when compared to the level ofinjuries prior to the ergonomics efforts.The number of lost workdays associatedwith lifting-related injuries was reportedto be at least 55% lower than levelsduring each of the previous four years.Citizens Memorial reported that thesereductions contributed to a direct savingsof approximately 150,000 in workers’compensation costs over a five yearperiod (8).
SECTIONIIA Process for Protecting WorkersThe number and severity ofinjuries resulting from physicaldemands in nursing homes — andassociated costs — can be substantially reduced (2, 9). Providing analternative to manual resident liftingis the primary goal of the ergonomicsprocess in the nursing home settingand of these guidelines. OSHArecommends that manual lifting ofresidents be minimized in all casesand eliminated when feasible. OSHAfurther recommends that employersdevelop a process for systematicallyaddressing ergonomics issues in theirfacilities, and incorporate thisprocess into an overall program torecognize and prevent occupationalsafety and health hazards.An effective process should betailored to the characteristics ofthe particular nursing home butOSHA generally recommends thefollowing steps:Provide Management SupportStrong support by managementcreates the best opportunity forsuccess. OSHA recommends thatemployers develop clear goals, assignresponsibilities to designated staffmembers to achieve those goals,provide necessary resources, andensure that assigned responsibilitiesare fulfilled. Providing a safe andhealthful workplace requires asustained effort, allocation ofresources, and frequent follow-upthat can only be achieved throughthe active support of management.Involve EmployeesEmployees are a vital source ofinformation about hazards in theirworkplace. Their involvement addsproblem-solving capabilities andhazard identification assistance,enhances worker motivation and jobsatisfaction, and leads to greateracceptance when changes are madein the workplace. Employees can: submit suggestions or concerns; discuss the workplace andwork methods; participate in the design ofwork, equipment, procedures,and training; evaluate equipment; respond to employee surveys; participate in task groups withresponsibility for ergonomics; and participate in developing the nursing home’s ergonomics process.Guidelines for Nursing Homes9
A Process for Protecting WorkersAn Identify ProblemsNursing homes can moresuccessfully recognize problems byestablishing systematic methods foridentifying ergonomics concerns intheir workplace. Information aboutwhere problems or potentialproblems may occur in nursinghomes can be obtained from avariety of sources, including OSHA300 and 301 injury and illnessinformation, reports of workers’compensation claims, accident andnear-miss investigation reports,insurance company reports,employee interviews, employeesurveys, and reviews and observationsof workplace conditions. Onceinformation is obtained, it can beused to identify and evaluate elementsof jobs that are associatedwith problems. Sections III and IVcontain further information onmethods for identifying ergonomicsconcerns in the nursing homeenvironment.Implement SolutionsWhen problems related toergonomics are identified, suitableoptions can then be selected andimplemented to eliminate hazards.Effective solutions usually involveworkplace modifications that10Guidelines for Nursing Homeseliminate hazards and improve thework environment. These changesusually include the use of equipment,work practices, or both. Whenchoosing methods for lifting andrepositioning residents, individualfactors should be taken into account.Such factors include the resident’srehabilitation plan, the need to restorethe resident’s functional abilities,medical contraindications, emergencysituations, and resident dignity andrights. Examples of solutions can befound in Sections III and IV.Address Reports of InjuriesEven in establishments witheffective safety and health programs,injuries and illnesses may occur.Work-related MSDs should bemanaged in the same manner andunder the same process as any otheroccupational injury or illness (10).Like many injuries and illnesses,employers and employees can benefitfrom early reporting of MSDs. Earlydiagnosis and intervention, includingalternative duty programs, areparticularly important in order tolimit the severity of injury, improvethe effectiveness of treatment,minimize the likelihood of disabilityor permanent damage, and reducethe amount of associated workers’compensation claims and costs.OSHA’s injury and illness recordingand reporting regulation (29 CFR1904) requires employers to keeprecords of work-related injuries andillnesses. These reports can help thenursing home identify problem areas
A Process for Protecting Workersand evaluate ergonomic efforts.Employees may not be discriminatedagainst for reporting a work-relatedinjury or illness. [29 U.S.C. 660(c)]Provide TrainingTraining is necessary to ensurethat employees and managers canrecognize potential ergonomics issuesin the workplace, and understandmeasures that are available tominimize the risk of injury. Ergonomics training can be integratedinto general training on performancerequirements and job practices.Effective training covers the problemsfound in each employee’s job. Moreinformation on training can be foundin Section V.Evaluate Ergonomics EffortsNursing homes should evaluatethe effectiveness of their ergonomicsefforts and follow-up on unresolvedproblems. Evaluation helps sustainthe effort to reduce injuries andillnesses, track whether or notergonomic solutions are working,identify new problems, and showareas where further improvement isneeded. Evaluation and follow-up arecentral to continuous improvementand long-term success. Once solutionsare introduced, OSHA recommendsthat employers ensure they areeffective. Various indicators (e.g.,OSHA 300 and 301 informationdata and workers’ compensationreports) can provide useful empiricaldata at this stage, as can other techniques such as employee interviews.For example, after introducing a newlift at a nursing home, the employershould follow-up by talking withemployees to ensure that the problemhas been adequately addressed. Inaddition, interviews provide amechanism for ensuring that thesolution is not only in place, but isbeing used properly. The same methodsthat are used to identify problems inmany cases can also be used forevaluation.Guidelines for Nursing Homes11
SECTIONIIIA Identifying Problems and Implementing Solutionsfor Resident Lifting and RepositioningIdentifying Problemsfor Resident Liftingand RepositioningAssessing the potential for workto injure employees in nursing homesis complex because typical nursinghome operations involve the repeatedlifting and repositioning of theresidents. Resident lifting andrepositioning tasks can be variable,dynamic, and unpredictable innature. In addition, factors such asresident dignity, safety, and medicalcontraindications should be takeninto account. As a result, specifictechniques are used for assessingresident lifting and repositioningtasks that are not appropriate forassessing the potential for injuryassociated with other nursinghome activities.An analysis of any resident liftingand repositioning task involves anassessment of the needs and abilitiesof the resident involved. Thisassessment allows staff members toaccount for resident characteristicswhile determining the safest methodsfor performing the task, within thecontext of a care plan that providesfor appropriate care and services forthe resident. Such assessmentstypically consider the resident’ssafety, dignity and other rights, aswell as the need to maintain orrestore a resident’s functional abilities.12Guidelines for Nursing HomesThe resident assessment shouldinclude examination of factorssuch as: the level of assistance the residentrequires; the size and weight of the resident; the ability and willingness ofthe resident to understand andcooperate; and any medical conditions that mayinfluence the choice of methodsfor lifting or repositioning.These factors are criticallyimportant in determiningappropriate methods for lifting andrepositioning a resident. The sizeand weight of the resident will, insome situations, determine whichequipment is needed and how manycaregivers are required to provideassistance. The physical and mentalabilities of the resident also play animportant role in selectingappropriate solutions. For example,a resident who is able and willing topartially support their own weightmay be able to move from his or herbed to a chair using a standing assistdevice, while a mechanical sling liftmay be more appropriate for thoseresidents who are unable to supporttheir own weight. Other factorsrelated to a resident’s condition mayneed to be taken into account aswell. For instance, a resident whohas recently undergone hipreplacement surgery may requirespecialized equipment for assistancein order to avoid placing stress onthe affected area.A number of protocols have beendeveloped for systematically examiningresident needs and abilities and/or
Identifying Problems and Implementing Solutionsfor Resident Lifting and RepositioningFIGURE 1 Transfer to and from: Bed to Chair, Chair to Toilet, Chair to Chair, or Car to ChairCan patientbear weight?FullyCaregiver assistance not needed;stand by for safety as needed.PartiallyIs the patientcooperative?YesNoNoIs the patientcooperative?NoStand and pivot technique using a gait/transfer belt(1 caregiver) -or- powered standing assist lift(1 caregiver)Use full body sling lift and2 caregivers.YesDoes thepatient haveupper extremitystrength? For seated transfer aid, must have chair with arms thatrecess or are removable. For full body sling lift, select a lift that was specificallydesigned to access a patient from the car (if the car isthe starting or ending destination). If partial weight bearing, transfer toward stronger side. Toileting slings are available for toileting. Bathing mesh slings are available for bathing.NoYesSeated transfer aid; may use gait/transfer belt until thepatient is proficient in completing transfer independently.FIGURE 2Source: The Patient Safety Center of Inquiry (Tampa, FL).Veterans Health Administration & Department of Defense.October 2001.Lateral Transfer to and from: Bed to Stretcher, TrolleyCaregiver assistance not needed;stand by for safety as needed.YesIf patient is 100 pounds:Use a lateral sliding aid and 2 caregivers.Can patient assist?Partially AbleNot At All Able Surfaces should be even for lateral patient moves. For patients with Stage III or IV pressure ulcers, caremust be taken to avoid shearing force.Source: The Patient Safety Center of Inquiry (Tampa, FL). VeteransHealth Administration & Department of Defense. October 2001.If patient is 100-200 pounds:Use a lateral sliding aid -or- a friction reducingdevice and 2 caregivers.If patient is 200 pounds: Use a lateral sliding aidand 3 caregivers -or- a friction-reducing device orlateral transfer device and 2 caregivers -ora mechanical lateral transfer device.Guidelines for Nursing Homes13
Identifying Problems and Implementing Solutionsfor Resident Lifting and Repositioningfor recommending procedures andequipment to be used for performinglifting and repositioning tasks. Thefollowing are some examples: The Resident Assessment Instrument,published by the Centers forMedicare and Medicaid Services(CMS), provides a structured,standardized approach for assessingresident capabilities and needsthat results in a care plan for eachresident. Caregivers can use thisinformation to help them determinethe appropriate method for liftingor repositioning residents. Manynursing homes use this system tocomply with CMS requirementsfor nursing homes. Employerscan access this information fromwww.cms.hhs.gov/medicaid/mds20/. Patient Care Ergonomics ResourceGuide: Safe Patient Handling andMovement is published by thePatient Safety Center of Inquiry,Veterans Health Administration andthe Department of Defense. Thisdocument provides flow charts(shown here in Figures 1-6) thataddress relevant resident assessmentfactors and recommends solutionsfor resident lifting and repositioningproblems. This material is oneexample of an assessment tool thathas been used successfully. Employerscan access this information fromwww.patientsafetycenter.com.Nursing home operators mayfind another tool or develop anassessment tool that works better intheir facilities. Appendix A of the SettlementAgreement between OSHA andBeverly Enterprises, entitled Lift14Guidelines for Nursing HomesProgram Policy and Guide,recommends solutions for residentlifting and repositioning problems,based on the CMS classificationsystem. (A rating of “4” indicatesa totally dependent resident; a “3”rating indicates residents that needextensive assistance; a “2/1”rating indicates residents that needonly limited assistance/generalsupervision. Residents rated “0”are independent.) Employers canaccess this information fromwww.osha.gov.The nursing home operator shoulduse an assessment tool which isappropriate for the conditions in anindividual nursing home. The specialneeds of bariatric (excessively heavy)residents may require additionalfocus. Assistive devices must becapable of handling the heavierweight involved, and modification ofwork practices may be necessary.A number of individuals in nursinghomes can contribute to residentassessment and the determination ofappropriate methods for assisting intransfer or repositioning. Interdisciplinaryteams such as staff nurses,certified nursing assistants, nursingsupervisors, physical therapists,physicians, and the resident or his/herrepresentative may all be involved. Ofcritical importance is the involvementof employees directly responsible forresident care and assistance, as theneeds and abilities of residents mayvary considerably over a short periodof time, and the employees responsiblefor providing assistance are in thebest position to be aware of andaccommodate such changes.
Identifying Problems and Implementing Solutionsfor Resident Lifting and RepositioningFIGURE 3 Transfer to and from: Chair to StretcherIs the patientcooperative?Use full-body sling lift and2 or more caregivers.NoYesCaregiver assistance not needed;stand by for safety as needed.FullyCan the patientbear weight?NoIf exam table/stretcher can be positionedto a low level, use a non-poweredstand-assist aid. If not, use a full-body sling lift.Use full-body sling lift and2 or more caregivers.Comments:High/low exam tables and stretchers would be ideal.Source: The Patient Safety Center of Inquiry (Tampa, FL).Veterans Health Administration & Department of Defense.October 2001.FIGURE 4 Reposition in Bed: Side-to-Side, Up in BedFullyCaregiver assistance notneeded; patient may/maynot use positioning aid.If patient is 200 pounds:Use a friction-reducing deviceand at least 3 caregivers.Can Patientassist?NoPartiallyAbleEncourage patientto assist using apositioning aid or cues.If patient is 200 pounds:Use a friction-reducing deviceand 2-3 caregivers.Use full-body sling lift -orfriction-reducing device and 2 ormore caregivers. This is not a one person task - DO NOT PULL FROM HEAD OF BED. When pulling a patient up in bed, the bed should be flat or Trendelenburgposition to aid in gravity, with the side rail down. For patient with Stage III or IV pressure ulcers, care should be taken toavoid shearing force. The height of the bed should be appropriate for staff safety (at the elbows). If the patient can assist when repositioning “up in bed”, ask the patient toflex the knees and push on the count of three.Source: The Patient Safety Center of Inquiry (Tampa, FL). VeteransHealth Administration & Department of Defense. October 2001.Guidelines for Nursing Homes15
Identifying Problems and Implementing Solutionsfor Resident Lifting and RepositioningFIGURE 5 Repostition in Chair: Wheelchair and Dependency ChairCan patientassist?Caregiver assistance not needed;stand by for safety as needed.FullyPartiallyNoIf patient has upper extremity strength inboth arms, have patient lift up whilecaregiver pushes knees to reposition.Does chairrecline?If patient lacks sensation, cues maybe needed to remind Patient to reposition.YesRecline chair and use a friction-reducingdevice and 2 caregivers.NoIs patientcooperative?Use full-body sling lift -or- non-poweredstand-assist aid and 1 to 2 caregivers.YesNoComments: This is not a one person task: DO NOT PULL FROM BEHIND CHAIR. Take full advantage of chair functions, e.g., chair that reclines, or use ofarm rest of chair to facilitate repositioning. Make sure the chair wheels are locked.Use full-body sling lift and2 or more caregivers.Source: The Patient Safety Center of Inquiry (Tampa, FL). Veterans Health Administration & Department of Defense. October 2001.FIGURE 6 Transfer a Patient Up From the FloorWas patientinjured?YesWas theinjury minor?Depends on type and severity of injury(follow Standard Operating Procedures).NoYesNo1Is patientindependent?Comments:Use full-body sling that goes all the way down to thefloor (most of the newer models are capable of this).1Modifications made with concurrence of Dr. AudreyNelson at Veterans Administration Hospital, Tampa,Florida.YesCaregiver assistance notneeded; stand by forsafety as needed.Source: The Patient Safety Center of Inquiry (Tampa, FL).Veterans Health Administration & Department of Defense. October 2001.16Guidelines for Nursing HomesNoFull-body sling lift needed with2 or more caregivers.
Identifying Problems and Implementing Solutionsfor Resident Lifting and RepositioningImplementing Solutionsfor Resident Liftingand RepositioningThe recommended solutionspresented in the following pages arenot intended to be an exhaustive list,nor does OSHA expect that all ofthem will be used in any givenfacility. The information represents arange of available options that afacility can consider using. Many ofthe solutions are simple, commonsense modifications to equipment orprocedures that do not requiresubstantial time or resources toimplement. Others may require moresignificant efforts. The integration ofvarious solutions into the nursinghome is a strategic decision that, ifcarefully planned and executed, willlead to long-term benefits. Equipment must meet applicable regulations regarding equipment design anduse, such as the restraint regulationsfrom the Centers for Medicare andMedicaid. In addition, administratorsshould follow any manufacturers’recommendations and review guidelines, such as the FDA Hospital BedSafety Workgroup Guidelines, tohelp ensure patient safety. Management should also be cognizant ofseveral factors that might restrict theapplication of certain measures, suchas residents’ rehabilitation plans, theneed for restoration of functionalabilities, other medical contraindications, emergency conditions,and residents’ dignity and rights.The procurement of equipmentand the selection of an equipmentsupplier are important considerationswhen implementing solutions.Employers should establish closeworking relationships with equipmentsuppliers. Such working relationshipshelp with obtaining training foremployees, modifying the equipmentfor special circumstances, andprocuring parts and service whenneeded. Employers will want to pa
successful in the nursing home environment. Providing care to nursing home residents is physically demanding work. Nursing home residents often require assistance to walk, bathe, or perform other normal daily activities. In some cases residents are totally dependent upon caregivers for mobility. Manual lifting and other tasks involving the .