Transcription
2022 Evidenceof CoverageRegister on our website to choose to receive plancommunications by email or online.NYC Medicare Advantage Plus (PPO)City of New YorkFor questions, please call Member Services: 1-833-325-1191 (TTY: 711)Monday through Friday, 8 a.m. to 9 p.m. ET, except holidayswww.empireblue.com/nyc-ma-plus5168300 517676MUSENMUB GRS EOC Covers (NON UNICARE) 2021 MA REV
EVIDENCE OF COVERAGEJanuary 1, 2022 – December 31, 2022Your Group-Sponsored Medicare Health Benefits and Services as a Member of NYCMedicare Advantage Plus (PPO)This booklet gives you the details about your Medicare health care coverage fromJanuary 1, 2022 – December 31, 2022. It explains how to get coverage for health care servicesyou need. This is an important legal document. Please keep it in a safe place.Member Services:For help or information, please call Member Services or go to your plan website:www.empireblue.com/nyc-ma-plus.Call toll free 1-833-325-1191 (TTY: 711), Monday through Friday, 8 a.m. to 9 p.m. ET, exceptholidays.This plan, NYC Medicare Advantage Plus (PPO), is offered by Empire BlueCross BlueShieldRetiree Solutions. When this Evidence of Coverage says “we,” “us” or “our,” it means EmpireBlueCross BlueShield Retiree Solutions. When it says “the plan,” “our plan” or “your plan,” itmeans NYC Medicare Advantage Plus (PPO). When it says “you” or “your” it means you, or yourcovered spouse, or domestic partner, and/or covered dependent(s).Our plan has free language interpreter services available to answer questions fromnon-English speaking members. Please call the Member Services number listed above torequest interpreter services.This document may be available in alternate formats. Please call the Member Services numberlisted above for additional information.OMB Approval 0938-1051 (Expires: February 29, 2024)Y0114 22 129813 I C 001 CTYONY 06/23/2021517970MUSENMUB 001 CTYONY
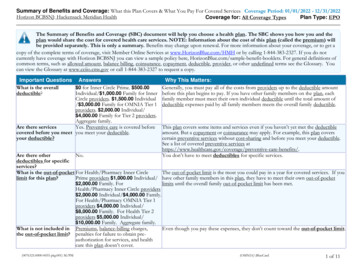
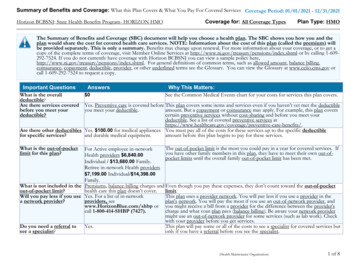
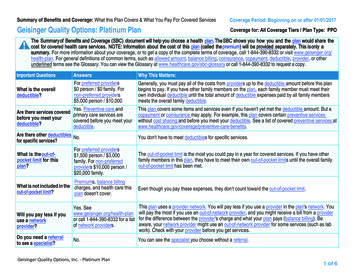
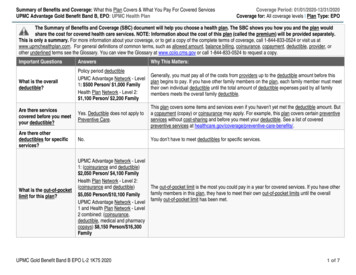
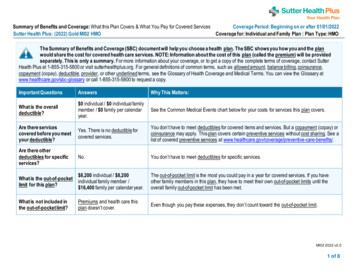
YOUR BENEFITS CHARTIn addition to your medical benefits, this chart includes information on supplementalbenefits, services and discountsLook for the apple!It shows a preventive service.2022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)1
Your 2022 Medical Benefits ChartNYC Medicare Advantage Plus PlanCity of New YorkCovered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkDoctor and hospital choiceYou may go to doctors, specialists, and hospitals in or out of thenetwork. You do not need a referral.Prior authorization*Benefit categories that include services that require priorauthorization are marked with an asterisk (*). Additionalinformation can be found on the last page of the medicalbenefits chart.Annual deductible The deductible applies to covered services as notedwithin each category below, prior to the copay orcoinsurance, if any, being applied. 253Combined in-network and out-of-networkInpatient servicesInpatient hospital care*Includes inpatient acute, inpatient rehabilitation, long-term carehospitals, and other types of inpatient hospital services.Inpatient hospital care starts the day you are formally admittedto the hospital with a doctor’s order. The day before you aredischarged is your last inpatient day.Covered services include but are not limited to: Semi-private room (or a private room if medicallynecessary) Meals, including special diets Regular nursing services Costs of special care units (such as intensive or coronarycare units) Drugs and medications Lab testsFor Medicarecovered hospitalstays:For Medicarecovered hospitalstays: 300 copay peradmissionDeductible doesnot apply. 300 copay peradmissionDeductible doesnot apply.The inpatienthospital out-ofpocket maximum is 750 per yearcombined withinpatient mentalhealth care andcombined innetwork and out-ofnetwork.The inpatienthospital out-ofpocket maximum is 750 per yearcombined withinpatient mentalhealth care andcombined innetwork and out-ofnetwork. X-rays and other radiology servicesY0114 22 3000419 I C 06/24/20212022 Custom PPO Plan 0P HCSPP500X12 MEALP56 C-TRPCity of New York2022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)07/28/20212
Covered servicesInpatient hospital care (con’t) Necessary surgical and medical supplies Use of appliances, such as wheelchairs Operating and recovery room costs Physical therapy, occupational therapy, and speechlanguage therapy Inpatient substance abuse services Inpatient dialysis treatments (if you are admitted as aninpatient to a hospital for special care) Under certain conditions, the following types oftransplants are covered: corneal, kidney, kidneypancreatic, heart, liver, lung, heart/lung, bone marrow,stem cell, and intestinal/multivisceral.What you must pay for thesecovered servicesIn-NetworkOut-of-NetworkNo limit to thenumber of dayscovered by theplan.No limit to thenumber of dayscovered by theplan. 0 copay forMedicare-coveredphysician servicesreceived while aninpatient during aMedicare-coveredhospital stayDeductible doesnot apply. 0 copay forMedicare-coveredphysician servicesreceived while aninpatient during aMedicare-coveredhospital stayDeductible doesnot apply.If you need a transplant, we will arrange to have yourcase reviewed by a Medicare-approved transplant centerthat will decide whether you are a candidate for atransplant. Transplant providers may be local or outsideof the service area. If our in-network transplant servicesare outside the community pattern of care, you maychoose to go locally as long as the local transplantproviders are willing to accept the Original Medicarerate. If the plan provides transplant services at a locationoutside the pattern of care for transplants in yourcommunity and you choose to obtain transplants at thisdistant location, we will arrange or pay for appropriatelodging and transportation costs for you and acompanion. The reimbursement for transportation costsare while you and your companion are traveling to andfrom the medical providers for services related to thetransplant care. The plan defines the distant location asa location that is outside of the member’s service areaAND a minimum of 75 miles from the member’s home.Transportation and lodging costs will be reimbursed fortravel mileage and lodging consistent with current IRStravel mileage and lodging guidelines. Accommodationsfor lodging will be reimbursed at the lesser of: 1) billedcharges, or 2) 50 per day per covered person up to amaximum of 100 per day per covered personconsistent with IRS guidelines.If you receiveauthorizedinpatient care at anout-of-networkhospital after youremergencycondition isstabilized, yourcost is the costsharing you wouldpay at an innetwork hospital.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)3
Covered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkInpatient hospital care (con’t) Blood – including storage and administration. Coverageof whole blood, packed red cells, and all othercomponents of blood begins with the first pint. Physician servicesIn-network providers should notify us within one business dayof any planned, and if possible, unplanned admissions ortransfers, including to or from a hospital, skilled nursing facility,long term acute care hospital, or acute rehabilitation center.Note: To be an inpatient, your provider must write an order toadmit you formally as an inpatient of the hospital. Even if youstay in the hospital overnight, you might still be considered an“outpatient.” If you are not sure if you are an inpatient, youshould ask the hospital staff.You can also find more information in a Medicare fact sheetcalled “Are You a Hospital Inpatient or Outpatient? If You HaveMedicare – Ask!” This fact sheet is available on the Web ient-orOutpatient.pdf or by calling 1-800-MEDICARE (1-800-633-4227).TTY users call 1-877-486-2048. You can call these numbers forfree, 24 hours a day, 7 days a week.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)4
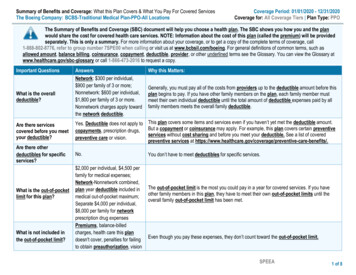
Covered servicesInpatient mental health care*Covered services include mental health care services thatrequire a hospital stay in a psychiatric hospital or thepsychiatric unit of a general hospital.In-network providers should notify us within one business dayof any planned, and if possible unplanned admissions ortransfers, including to or from a hospital, skilled nursing facility,long term acute care hospital, or acute rehabilitation center.What you must pay for thesecovered servicesIn-NetworkOut-of-NetworkFor Medicarecovered hospitalstays:For Medicarecovered hospitalstays: 300 copay peradmissionDeductible doesnot apply. 300 copay peradmissionDeductible doesnot apply.The inpatientmental health careout-of-pocketmaximum is 750per year combinedwith inpatienthospital care andcombined innetwork and out-ofnetwork.The inpatientmental health careout-of-pocketmaximum is 750per year combinedwith inpatienthospital care andcombined innetwork and out-ofnetwork.No limit to thenumber of dayscovered by theplan.No limit to thenumber of dayscovered by theplan. 0 copay forMedicare-coveredphysician servicesreceived while aninpatient during aMedicare-coveredhospital stayDeductible doesnot apply. 0 copay forMedicare-coveredphysician servicesreceived while aninpatient during aMedicare-coveredhospital stayDeductible doesnot apply.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)5
Covered servicesSkilled nursing facility (SNF) care*Inpatient skilled nursing facility (SNF) coverage is limited to 100days each benefit period. A “benefit period” begins on the firstday you go to a Medicare-covered inpatient hospital or a SNF.The benefit period ends when you have not been an inpatient atany hospital or SNF for 60 days in a row.Covered services include but are not limited to: Semi-private room (or a private room if medicallynecessary) Meals, including special diets Skilled nursing services Physical therapy, occupational therapy, and speechlanguage therapy Drugs administered to you as part of your plan of care(this includes substances that are naturally present inthe body, such as blood clotting factors) Blood – including storage and administration. Coverageof whole blood, packed red cells, and all othercomponents of blood begins with the first pint. Medical and surgical supplies ordinarily provided bySNFs Laboratory tests ordinarily provided by SNFs X-rays and other radiology services ordinarily providedby SNFs Use of appliances such as wheelchairs ordinarilyprovided by SNFs Physician/Practitioner servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkFor Medicarecovered SNF stays:For Medicarecovered SNF stays: 0 copayfor days 1-100per benefit periodDeductible doesnot apply. 0 copayfor days 1-100per benefit periodDeductible doesnot apply.No prior hospitalstay required.No prior hospitalstay required.Generally, you will receive your SNF care from plan facilities.However, under certain conditions listed below, you may beable to pay in-network cost-sharing for a facility that isn’t a planprovider, if the facility accepts our plan’s amounts for payment. A nursing home or continuing care retirementcommunity where you were living right before you wentto the hospital (as long as it provides skilled nursingfacility care) A SNF where your spouse is living at the time you leavethe hospitalY0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)6
Covered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkSkilled nursing facility (SNF) care (con’t)In-network providers should notify us within one business dayof any planned, and if possible unplanned admissions ortransfers, including to or from a hospital, skilled nursing facility,long term acute care hospital, or acute rehabilitation center.Inpatient services covered when the hospital or SNF days arenot covered or are no longer covered*If you have exhausted your inpatient benefits or if the inpatientstay is not reasonable and necessary, we will not cover yourinpatient stay. However, in some cases, we will cover certainservices you receive while you are in the hospital or a skillednursing facility (SNF).After your SNF day limits areused up, this plan will still pay for coveredphysician services and other medicalservices outlined in this benefits chart atthe deductible and/or cost shareamounts indicated.Covered services include, but are not limited to: Physician services Diagnostic tests (like lab tests) X-ray, radium, and isotope therapy including technicianmaterials and services Surgical dressings Splints, casts, and other devices used to reducefractures and dislocations Prosthetic and orthotic devices (other than dental) thatreplace all or part of an internal body organ (includingcontiguous tissue), or all or part of the function of apermanently inoperative or malfunctioning internal bodyorgan, including replacement or repairs of such devices Leg, arm, back and neck braces, trusses and artificiallegs, arms, and eyes including adjustments, repairs andreplacements required because of breakage, wear, loss,or a change in the patient's physical condition Physical therapy, occupational therapy, and speechlanguage therapyY0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)7
Covered servicesHome health agency care*Prior to receiving home health services, a doctor must certifythat you need home health services and will order home healthservices to be provided by a home health agency. You must behomebound, which means leaving home is a major effort.Covered services include, but are not limited to: Part-time or intermittent skilled nursing and homehealth aide services (to be covered under the homehealth care benefit, your skilled nursing and homehealth aide services combined must total fewer than 8hours per day and 35 hours per week) Physical therapy, occupational therapy, and speechlanguage therapy Medical and social services Medical equipment and suppliesWhat you must pay for thesecovered servicesIn-NetworkOut-of-Network 0 copay forMedicare-coveredhome health visitsDeductible doesnot apply. 0 copay forMedicare-coveredhome health visitsDeductible doesnot apply.Durable MedicalEquipment (DME)copay orcoinsurance, if any,may apply.Durable MedicalEquipment (DME)copay orcoinsurance, if any,may apply.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)8
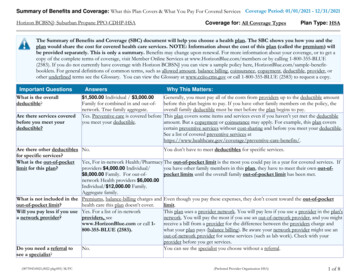
Covered servicesHospice careYou may receive care from any Medicare-certified hospiceprogram. You are eligible for the hospice benefit when yourdoctor and the hospice medical director have given you aterminal prognosis certifying that you’re terminally ill andhave six months or less to live if your illness runs its normalcourse. Your hospice doctor can be an in-network provider oran out-of-network provider.For hospice services and for services that are covered byMedicare Part A or B and are related to your terminalprognosis: Original Medicare (rather than this plan) will pay foryour hospice services and any Part A and Part B servicesrelated to your terminal prognosis. While you are in thehospice program, your hospice provider will bill Medicare forthe services that Original Medicare pays for.Services covered by Original Medicare include: Drugs for symptom control and pain relief Short-term respite care Home careWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkYou must receivecare from aMedicare-certifiedhospice.You must receivecare from aMedicare-certifiedhospice.When you enroll ina Medicarecertified hospiceprogram, yourhospice servicesand your Part A andB services are paidfor by OriginalMedicare, not thisplan.When you enroll ina Medicarecertified hospiceprogram, yourhospice servicesand your Part A andB services are paidfor by OriginalMedicare, not thisplan. 0 copay for theone time onlyhospiceconsultationDeductible doesnot apply. 0 copay for theone time onlyhospiceconsultationDeductible doesnot apply.Our plan covers hospice consultation services (one time only)for a terminally ill person who hasn’t elected the hospicebenefit.For services that are covered by Medicare Part A or B and arenot related to your terminal prognosis: If you neednonemergency, nonurgently needed services that are coveredunder Medicare Part A or B and that are not related to yourterminal prognosis, your cost for these services depends onwhether you use a provider in our plan’s network: If you obtain the covered services from an in-networkprovider, you only pay the plan cost-sharing amount forin-network services. If you obtain the covered services from an out-ofnetwork provider, you pay the plan cost-sharing forout-of-network services.For services that are covered by this plan but are not coveredby Medicare Part A or B: This plan will continue to cover plancovered services that are not covered under Part A or Bwhether or not they are related to your terminal prognosis.You pay your plan cost-sharing amount for these services.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)9
Covered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkHospice care (con’t)If you have Part D prescription drug coverage, some drugs maybe covered under your Part D benefit. Drugs are never coveredby both hospice and your Part D plan at the same time.Note: If you need non-hospice care (care that is not related toyour terminal prognosis), you should contact us to arrange theservices.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)10
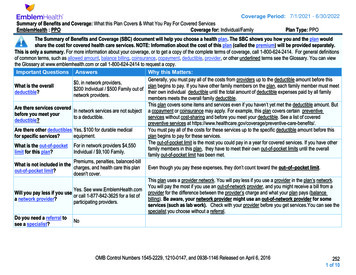
Covered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkOutpatient servicesPhysician services, including doctor’s office visits*Covered services include: Medically-necessary medical care or surgery servicesfurnished in a physician’s office, certified ambulatorysurgical center, hospital outpatient department, or anyother location Consultation, diagnosis, and treatment by a specialist Retail health clinics Basic hearing and balance exams performed by yourPrimary Care Physician or specialist, if your doctororders it to see if you need medical treatment Telehealth services for some physician or mental healthservices can be found in the section of this benefit charttitled, Video doctor visits. Some telehealth services including consultation,diagnosis, and treatment by a physician or practitionerfor patients in certain rural areas or other locationsapproved by Medicare Telehealth services for monthly end-stage renal diseaserelated visits for home dialysis members in a hospitalbased or critical access hospital-based renal dialysiscenter, renal dialysis facility, or the member’s home Telehealth services to diagnose, evaluate, or treatsymptoms of a stroke, regardless of your location Telehealth services for members with a substance usedisorder or co-occurring mental health disorder,regardless of their location Virtual check-ins (for example, by phone or video chat)with your doctor for 5-10 minutes if:o You’re not a new patient and 0 copay per visitto an in-networkPrimary CarePhysician (PCP) forMedicare-coveredservicesDeductible applies. 0 copay per visitto an out-ofnetwork PrimaryCare Physician(PCP) for Medicarecovered servicesDeductible applies. 15 copay per visitto an in-networkspecialist forMedicare-coveredservicesDeductible applies. 15 copay per visitto an out-ofnetwork specialistfor Medicarecovered servicesDeductible applies. 0 copay per visitto an in-networkretail health clinicfor Medicarecovered servicesDeductible applies. 0 copay per visitto an out-ofnetwork retailhealth clinic forMedicare-coveredservicesDeductible applies. 0 copay forMedicare-coveredallergy testingDeductible applies. 0 copay forMedicare-coveredallergy testingDeductible applies. 0 copay forMedicare-coveredallergy injectionsDeductible applies. 0 copay forMedicare-coveredallergy injectionsDeductible applies.See antigen costshare in Part Bdrug section.See antigen costshare in Part B drugsection.o The check-in isn’t related to an office visit in thepast 7 days ando The check-in doesn’t lead to an office visit within24 hours or the soonest available appointmentY0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)11
Covered servicesWhat you must pay for thesecovered servicesIn-NetworkOut-of-NetworkPhysician services, including doctor’s office visits (con’t) Evaluation of video and/or images you send to yourdoctor, and interpretation and follow-up by your doctorwithin 24 hours if:o You’re not a new patient ando The evaluation isn’t related to an office visit inthe past 7 days ando The evaluation doesn’t lead to an office visitwithin 24 hours or the soonest availableappointment Consultation your doctor has with other doctors byphone, internet, or electronic health record Second opinion by another in-network provider prior tosurgery Physician services rendered in the home Outpatient hospital services Non–routine dental care (covered services are limited tosurgery of the jaw or related structures, setting fracturesof the jaw or facial bones, extraction of teeth to preparethe jaw for radiation treatments of neoplastic cancerdisease, or services that would be covered whenprovided by a physician) Allergy testing and allergy injectionsChiropractic services We cover only manual manipulation of the spine tocorrect subluxation. 15 copay for eachMedicare-coveredvisitDeductible applies. 15 copay for eachMedicare-coveredvisitDeductible applies.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)12
Covered servicesAcupuncture for chronic low back pain*Covered services include:Up to 12 visits in 90 days are covered for Medicarebeneficiaries under the following circumstances:What you must pay for thesecovered servicesIn-NetworkOut-of-Network 15 copay for eachMedicare-coveredvisitDeductible applies. 15 copay for eachMedicare-coveredvisitDeductible applies.For the purpose of this benefit, chronic low back pain is definedas: Lasting 12 weeks or longer; Nonspecific, in that it has no identifiable systemic cause(i.e., not associated with metastatic, inflammatory,infectious, etc. disease); Not associated with surgery; and Not associated with pregnancy.An additional eight sessions will be covered for those patientsdemonstrating an improvement. No more than 20 acupuncturetreatments may be administered annually.Treatment must be discontinued if the patient is not improvingor is regressing.Provider Requirements:Physicians (as defined in 1861(r)(1) of the Social Security Act(the Act) may furnish acupuncture in accordance withapplicable state requirements.Physician assistances (PAs), nurse practitioners (NPs)/clinicalnurse specialists (CNSs) (as identified in 1861(aa)(5) of the Act),and auxiliary personnel may furnish acupuncture if they meetall applicable state requirements and have: A masters or doctoral level degree in acupuncture orOriental Medicine from a school accredited by theAccreditation Commission on Acupuncture and OrientalMedicine (ACAOM); and, A current, full, active, and unrestricted license topractice acupuncture in a State, Territory, orCommonwealth (i.e. Puerto Rico) of the United Sates, orDistrict of Columbia.Auxiliary personnel furnishing acupuncture must be under theappropriate level of supervision of a physician, PA, or NP/CNSrequired by our regulations at 42 CFR §§ 410.26 and 410.27.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)13
Covered servicesPodiatry services*Covered services include: Diagnosis and the medical or surgical treatment ofinjuries and disease of the feet (such as hammer toe orheel spurs) in an office setting Medicare-covered routine foot care for members withcertain medical conditions affecting the lower limbs A foot exam covered every six months for people withdiabetic peripheral neuropathy and loss of protectivesensationsWhat you must pay for thesecovered servicesIn-NetworkOut-of-Network 15 copay for eachMedicare-coveredvisitDeductible applies. 15 copay for eachMedicare-coveredvisitDeductible applies.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)14
Covered servicesOutpatient mental health care, including partialhospitalization services*Covered services include: Mental health services provided by a state-licensedpsychiatrist or doctor, clinical psychologist, clinicalsocial worker, clinical nurse specialist, nursepractitioner, physician assistant, or other Medicarequalified mental health care professional as allowedunder applicable state laws“Partial hospitalization” is a structured program of activepsychiatric treatment provided as a hospital outpatient servicethat is more intense than the care received in your doctor’s ortherapist’s office and is an alternative to inpatienthospitalization.What you must pay for thesecovered servicesIn-NetworkOut-of-Network 15 copay for eachMedicare-coveredprofessionalindividual therapyvisitDeductible applies. 15 copay for eachMedicare-coveredprofessionalindividual therapyvisitDeductible applies. 15 copay for eachMedicare-coveredprofessional grouptherapy visitDeductible applies. 15 copay for eachMedicare-coveredprofessional grouptherapy visitDeductible applies. 15 copay for eachMedicare-coveredprofessional partialhospitalization visitDeductible applies. 15 copay for eachMedicare-coveredprofessional partialhospitalization visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility individualtherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility individualtherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility grouptherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility grouptherapy visitDeductible applies. 0 copay for eachMedicare-coveredpartialhospitalizationfacility visitDeductible applies. 0 copay for eachMedicare-coveredpartialhospitalizationfacility visitDeductible applies.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)15
Covered servicesOutpatient substance abuse services, including partialhospitalization services*“Partial hospitalization” is a structured program of activepsychiatric treatment provided as a hospital outpatient servicethat is more intense than the care received in your doctor’s ortherapist’s office and is an alternative to inpatienthospitalization.What you must pay for thesecovered servicesIn-NetworkOut-of-Network 15 copay for eachMedicare-coveredprofessionalindividual therapyvisitDeductible applies. 15 copay for eachMedicare-coveredprofessionalindividual therapyvisitDeductible applies. 15 copay for eachMedicare-coveredprofessional grouptherapy visitDeductible applies. 15 copay for eachMedicare-coveredprofessional grouptherapy visitDeductible applies. 15 copay for eachMedicare-coveredprofessional partialhospitalization visitDeductible applies. 15 copay for eachMedicare-coveredprofessional partialhospitalization visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility individualtherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility individualtherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility grouptherapy visitDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility grouptherapy visitDeductible applies. 0 copay for eachMedicare-coveredpartialhospitalizationfacility visitDeductible applies. 0 copay for eachMedicare-coveredpartialhospitalizationfacility visitDeductible applies.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)16
Covered servicesOutpatient surgery, including services provided at hospitaloutpatient facilities and ambulatory surgical centers*Facilities where surgical procedures are performed and thepatient is released the same day.Note: If you are having surgery in a hospital, you should checkwith your provider about whether you will be an inpatient oroutpatient. Unless the provider writes an order to admit you asan inpatient to the hospital, you are an outpatient and pay thecost-sharing amounts for outpatient surgery. Even if you stay inthe hospital overnight, you might still be considered an“outpatient.”You can also find more information in a Medicare fact sheetcalled “Are You a Hospital Inpatient or Outpatient? If You HaveMedicare – Ask!” This fact sheet is available on the Web ient-orOutpatient.pdf or by calling 1-800-MEDICARE (1-800-633-4227).TTY users call 1-877-486-2048. You can call these numbers forfree, 24 hours a day, 7 days a week.What you must pay for thesecovered servicesIn-NetworkOut-of-Network 0 copay for eachMedicare-coveredoutpatient hospitalfacility orambulatorysurgical center visitfor surgeryDeductible applies. 0 copay for eachMedicare-coveredoutpatient hospitalfacility orambulatorysurgical center visitfor surgeryDeductible applies. 0 copay for eachMedicare-coveredoutpatientobservation roomvisitDeductible applies. 0 copay for eachMedicare-coveredoutpatientobservation roomvisitDeductible applies.Y0114 22 3000419 I C 06/24/20212022 Evidence of Coverage for NYC Medicare Advantage Plus (PPO)17
Covered servicesOutpatient hospital observation, non-surgical*Observation services are hospital outpatient services given todetermine if you need to be admitted as an inpatient or can bedischarged.For outpatient hospital observation services to be covered, theymust meet the Medicare criteria and be considered reasonableand necessary. Observation services are covered only whenprovided by the order of a physician or another individualauthorized by state licensure law and hospital staf
Jan 1, 2022