Transcription
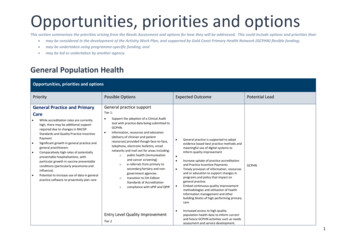
Opportunities, priorities and optionsThis section summarises the priorities arising from the Needs Assessment and options for how they will be addressed. This could include options and priorities that: may be considered in the development of the Activity Work Plan, and supported by Gold Coast Primary Health Network (GCPHN) flexible funding; may be undertaken using programme-specific funding; and may be led or undertaken by another agency.General Population HealthOpportunities, priorities and optionsPriorityPossible OptionsGeneral Practice and PrimaryCareGeneral practice support While accreditation rates are currentlyhigh, there may be additional supportrequired due to changes in RACGPStandards and Quality Practice IncentivePaymentSignificant growth in general practice andgeneral practitionersComparatively high rates of potentiallypreventable hospitalisations, withparticular growth in vaccine preventableconditions (particularly pneumonia andinfluenza)Potential to increase use of data in generalpractice software to proactively plan careExpected OutcomePotential LeadTier 1: Support the adoption of a Clinical Audittool with practice data being submitted toGCPHN.Information, resources and education(delivery of clinician and patientresources) provided though face-to-face,telephone, electronic bulletins, emailnetworks and mail out for areas including:opublic health (immunisationand cancer screening)oe-referrals from primary tosecondary/tertiary and nongovernment agenciesotransition to 5th EditionStandards of Accreditationocompliance with ePIP and QPIP.Entry Level Quality ImprovementTier 2 General practice is supported to adoptevidence based best practice methods andmeaningful use of digital systems toinform quality improvementIncrease uptake of practice accreditationand Practice Incentive PaymentsTimely provision of information, resourcesand or education to support changes inprograms and policy that impact ongeneral practice.Embed continuous quality improvementmethodologies and utilisation of healthinformation management and otherbuilding blocks of high performing primarycareGCPHNIncreased access to high qualitypopulation health data to inform currentand future GCPHN activities such as needsassessment and service development.1
Opportunities, priorities and optionsPriorityPossible Options Practices enrolled are provided withquarterly reports which includesoa practice profile andoanalysis of clinical dataidentifying key trends and areasfor improvementsSupport for effective data entry, datacleaning and quality assurance processesExpected Outcome Improved management of patient healthcare in general practiceReducing unnecessary referrals andadmissions to hospital.Potential LeadGCPHNContinuous quality improvement(CQI)Tier 3 Practice Support Supported implementation of continuousquality improvement methodologies usingpractice data to drive improvements andother building blocks of high performingprimary care Collection and use of clinical data toimprove the population’s health The General Practice determines priorityareas for improvement through review oftheir clinical data Development of an action plan utilising aCQI methodology through peer to peerconversations Develop tailored clinical audit reports todetermine baselines measures andmonitor improvement over time Review and monitor progress towardsachievements/improvements Access to decision support tools includingcycles of care through GCPHN website.Population health managementTier 4 Practice Support2
Opportunities, priorities and optionsPriorityPossible Options General Practice and PrimaryCare Clinical handover, particularly to generalpractice on discharge from hospitalsremains a significant issueComparatively high rates of potentiallypreventable hospitalisations, withparticular growth in vaccine preventableconditions (particularly pneumonia andinfluenzaAccess to Information about services andresources to support general practice inkey areas requiredPotential to increase use of data in generalpractice software to proactively plan careCurrent systems (including MBS paymentsand data) do not support population healthapproach and care-coordination Potential LeadCreate a single integrated healthcare system forthe Gold Coast by: Improving the coordination of care toensure consumers receive the right care atthe right place at the right time by theright person. Increasing the effectiveness and efficiencyof health services for consumers. Engaging and supporting clinicians tofacilitate improvements in our healthsystem.GCPHN with Gold Coast Health (GCH)Allocated Practice Support Officer tofacilitate improved comprehensive andpatient centred care planningDevelop person centred, goal orientatedcare plans that align with MBSrequirements.Provide education and training in the useof the care plans template which supportutilisation of systematic cycles of carerequiring recall and reminder wherenecessary to support improved patientmanagement.Provide regular data reports to monitorimprovement in care management ofpatients.Links with Primary Sense in section belowIntegrated Care Alliance Expected OutcomeSupport the implementation of newintegrated models of care.Preliminary work to develop models ofcare have been completed for a range ofdisease conditions. Implementationrequirements are currently being scoped.A major body of work for GCPHN involvesthe implementation of a e-library solutionto enable all clinicians on the Gold Coastto review and utilise new pathways to careresulting from the re-design work.Primary SenseContinue refinement and implementation intrial practices of automated pseudonymiseddata extraction and analysis of the health profileof the entire practice population. This includesgenerating actionable optimal care reports andPrimary Sense will support general practices tomake timely decisions for better health care fortheir respective populations by: Integrating diagnosis, medications andpathology data from practice managementsystems and applying evidenced basedalgorithms.GCPHN with key stakeholders3
Opportunities, priorities and optionsPriorityGeneral Practice and PrimaryCare While categories 4 and 5 ED presentationshave remained stable, there has beenstrong growth in higher acuity categories,increasing demand on ED servicesAccess to Information about services andresources to support general practice inkey areas requiredPossible OptionsExpected Outcomemedication safety alerts for general practices,analysed population health data for the practiceto inform the service response and for GCPHNneeds assessment and other commissioningpurposes. Primary Sense: Highlights patients with complex andcomorbid conditions to targetproactive and coordinated care Highlights patients at risk ofhospitalisation for coordinated care(some cross over with group above) Highlights patients at risk of chronicdisease to target proactive healthassessment Highlights patients at risk ofpolypharmacy for medication review Alerts of patients at immediate riskfrom medication prescribing safetyissues Potential LeadIdentifying high risk groups for proactivecare.Relaying analysed de-identified patientinformation as data becomes available,enabling the practices to plan andcoordinate care in an efficient way sopatients get the right care at the righttime.Providing clinical audit functions e.g. preaccreditation data checks, and a riskstratified profile of the entire practicepatient population including high impactconditions, multi-morbidity andpolypharmacy profiles.Primary Sense will also enhance the level anddetail of service planning that GCPHN can dobased on historic and current pseudonymisedpatient level, practice level, and regional leveldata, enabling predictive modelling andtracking outcomes over time.Emergency AlternativesThis will involve promotion of after-hoursdoctor’s services, online and telephone servicesto improve awareness of options and helppeople make appropriate and informeddecisions. We anticipate this will assist toreduce the burden in Emergency departmentsby reducing the number of unnecessary orinappropriate presentations.Contribute to prevention of increasing numbersof Cat 4 and 5 presentations to EDGCPHN with GCHActivities include: Collateral development and distribution,including magnets, brochures and posters,to be distributed through general practiceand GCH emergency department. Online advertising, social media and radioadvertising Usual GCPHN and GCH publications Tonic advertising at pharmacy4
Opportunities, priorities and optionsPriorityPossible Options Continue refinement and implementation intrial practices of automated pseudonymiseddata extraction and analysis of the health profileof the entire practice population. This includesgenerating actionable optimal care reports andmedication safety alerts for general practices,analysed population health data for the practiceto inform the service response and for GCPHNneeds assessment and other commissioningpurposes. Primary Sense: Highlights patients with complex andcomorbid conditions to targetproactive and coordinated care Highlights patients at risk ofhospitalisation for coordinated care(some cross over with group above) Highlights patients at risk of chronicdisease to target proactive healthassessment Highlights patients at risk ofpolypharmacy for medication review Alerts of patients at immediate riskfrom medication prescribing safetyissues Access to Information about services andresources to support general practice inkey areas requiredPotential LeadPrimary Sense will support general practices tomake timely decisions for better health care fortheir respective populations by: Integrating diagnosis, medications andpathology data from practice managementsystems and applying evidenced basedalgorithms. Identifying high risk groups for proactivecare. Relaying analysed de-identified patientinformation as data becomes available,enabling the practices to plan andcoordinate care in an efficient way sopatients get the right care at the righttime. Providing clinical audit functions e.g. preaccreditation data checks, and a riskstratified profile of the entire practicepatient population including high impactconditions, multi-morbidity andpolypharmacy profiles.GCPHN with key stakeholdersAdvertising through GCUH screens in foyerand emergency waiting areas.Primary SenseGeneral Practice and PrimaryCareExpected OutcomeAccess to information andresourcesGCPHN will continue to host, develop the I.T.infrastructure, update and market the existingweb portal featuring: Localised referral guidelines and templatesfor Gold Coast Health, updated to reflectthe Clinical Prioritisation Criteria protocolsintroduced in Queensland Review and update of existing referraltemplates to ensure they align to currentevidence and GCH systems and protocolsPrimary Sense will also enhance the level anddetail of service planning that GCPHN can dobased on historic and current pseudonymisedpatient level, practice level, and regional leveldata, enabling predictive modelling andtracking outcomes over time. Achieving increased access tocontemporary evidence-based resourcesand localised service and referralinformation.Increase direct links to local serviceprovider information in health topic areasand information and resources publishedonline to support appropriate, timelyreferrals and agreed service pathways.GCPHN with GCH5
Opportunities, priorities and optionsPriorityPossible Options Expected OutcomePotential LeadOther clinical and service navigationsupport information including theemerging new models of careProfessional resourcesPatient facing resourcesA detailed local service directory.In addition, other software options as well asthe structure of the current HealthyGC websitewill be reviewed and compared to ensure theservice continues to function in the mosteffective and efficient way.Work cooperatively with the National HealthService Directory to ensure effectiveinformation sharing.This activity links closely with practice supportactivities and other program activities.Cancer High rates of melanoma across the region.Higher rates of colorectal cancer and breastcancer but lower rates of screeningcompared to national rates.Low community awareness of eligibility forscreening in Gold Coast region, men inparticular.Public Awareness - CancerPublic awareness campaigns promotingscreening and skin checks through usualcommunication channels including informationand resources on the website “HealthyGC”,GCPHN publications, social and traditionalmedia, targeting particular hot spot areas.General practice support – helpdesk Increase in awareness and uptake ofscreening services for breast, bowel andcervical screening.Increased skin cancer and prostate cancercheck.GCPHNGCPHNHelp desk support to general practice to supportgeneral enquiries including access to resourcesfor cancer.General Practice Support – QualityImprovementImmunisationQuality improvement activities (tier 3) ingeneral practice support to include preventionas potential focus area including recall andreminder of potentially eligible patients forscreening options through Health Assessmentsand skin checks.GCPHNPublic Awareness – ImmunisationGCPHN6
Opportunities, priorities and optionsPriority Lower rates of children fully immunised inthe Gold Coast particularly hinterland,Surfers Paradise and MudgeerabaTallebudgera.Lower rates of HPV vaccination in GoldCoast compared to the national figure.Higher rates of hospitalisation forpneumonia and influenza in Gold Coastcompared to the national figure.Possible OptionsExpected OutcomePublic awareness campaigns promoting earlychildhood, HPV and influenza vaccinationsthrough usual communications channelsincluding information and resources on thewebsite “HealthyGC”, GCPHN publications,social and traditional media, targeting particularhot spot areas. Potential LeadIncrease in awareness and uptake ofvaccinations.General practice support – helpdeskGCPHNHelp desk support to general practice to supportgeneral enquiries including access to resourcesfor immunisation.General Practice Support – QualityImprovementQuality improvement activities (tier 3) ingeneral practice support to include preventionas potential focus area including recall /reminder of potentially eligible patients forvaccinationsPersistent Pain High rates of musculoskeletal conditions inGold Coast North and CoolangattaAgeing population means moremusculoskeletal conditions projectedPain management frequently focusses onmedicationHigh levels of opioid dispensing acrossregion, particularly SouthportNeed for more awareness and support forprevention and self-managementFocus on multidisciplinary and coordinatedcareChronic DiseaseContinuation of Persistent PainProgramTurning Pain Into Gain program has thefollowing service components: Patient self-management educationprogram Individual patient assessment includingsupport to navigate service providers andrecommendations to patient’s GP Access to additional allied health serviceswhere required GP and allied health services education Peer-to-peer support group lead byprevious participants Refresher workshops for participants at 6months, 9 months and 12 months’ postprogramEvaluation using validated toolsIntegrated Care AllianceContractor Improved self-management of painReduced use of pain medicationReduced hospital presentationsCreate a single integrated healthcare system forthe Gold Coast by:GCPHN with GCH7
Opportunities, priorities and optionsPriority Better systems to support carecoordination.Referral pathways and care coordinationincluding self-management systems toidentify suspected at-risk patients.Need for greater focus on prevention, earlyidentification and self-management.High rates of smoking and harmful alcoholintake across the region.Chronic Disease Better systems to support carecoordination.Referral pathways and care coordinationincluding self-management systems toidentify suspected at-risk patients.Need for greater focus on prevention, earlyidentification and self-management.High rates of smoking and harmful alcoholintake across the region.Possible Options Support the implementation of newintegrated models of care.Preliminary work to develop models ofcare have been completed for a range ofdisease conditions. Implementationrequirements are currently being scoped.A major body of work for GCPHN involvesthe implementation of a e-library solutionto enable all clinicians on the Gold Coastto review and utilise new pathways to careresulting from the re-design work.Primary SenseContinue refinement and implementation intrial practices of automated pseudonymiseddata extraction and analysis of the health profileof the entire practice population. This includesgenerating actionable optimal care reports andmedication safety alerts for general practices,analysed population health data for the practiceto inform the service response and for GCPHNneeds assessment and other commissioningpurposes. Primary Sense: Highlights patients with complex andcomorbid conditions to targetproactive and coordinated care Highlights patients at risk ofhospitalisation for coordinated care(some cross over with group above) Highlights patients at risk of chronicdisease to target proactive healthassessment Highlights patients at risk ofpolypharmacy for medication review Alerts of patients at immediate riskfrom medication prescribing safetyissuesExpected Outcome Potential LeadImproving the coordination of care toensure consumers receive the right care atthe right place at the right time by theright person.Increasing the effectiveness and efficiencyof health services for consumers.Engaging and supporting clinicians tofacilitate improvements in our healthsystem.Primary Sense will support general practices tomake timely decisions for better health care fortheir respective populations by: Integrating diagnosis, medications andpathology data from practice managementsystems and applying evidenced basedalgorithms. Identifying high risk groups for proactivecare. Relaying analysed de-identified patientinformation as data becomes available,enabling the practices to plan andcoordinate care in an efficient way sopatients get the right care at the righttime. Providing clinical audit functions e.g. preaccreditation data checks, and a riskstratified profile of the entire practicepatient population including high impactconditions, multi-morbidity andpolypharmacy profiles. Primary Sense will also enhance the leveland detail of service planning that GCPHNcan do based on historic and currentpseudonymised patient level, practicelevel, and regional level data, enablingpredictive modelling and trackingoutcomes over time.GCPHN with key stakeholders8
Opportunities, priorities and optionsPriorityPossible OptionsChronic DiseaseAccess to information andresources Better systems to support carecoordination.Referral pathways and care coordinationincluding self-management systems toidentify suspected at-risk patients.Need for greater focus on prevention, earlyidentification and self-management.High rates of smoking and harmful alcoholintake across the region.GCPHN will continue to host, develop the I.T.infrastructure, update and market the existingweb portal featuring: Localised referral guidelines and templatesfor Gold Coast Health, updated to reflectthe Clinical Prioritisation Criteria protocolsintroduced in Queensland Review and update of existing referraltemplates to ensure they align to currentevidence and GCH systems and protocols Other clinical and service navigationsupport information including theemerging new models of care Professional resources Patient facing resources A detailed local service directory.Expected OutcomePotential LeadGCPHN with GCH Achieving increased access tocontemporary evidence-based resourcesand localised service and referralinformation.Increase direct links to local serviceprovider information in health topic areasand information and resources publishedonline to support appropriate, timelyreferrals and agreed service pathways.GCPHNGCPHNIn addition, other software options as well asthe structure of the current HealthyGC websitewill be reviewed and compared to ensure theservice continues to function in the mosteffective and efficient way.Work cooperatively with the National HealthService Directory to ensure effectiveinformation sharing.This activity links closely with practice supportactivities and other program activities.Population health managementUsing the learnings from previousComprehensive Over 75 Care Plan projectevaluation, support implementation ofcomprehensive proactive management ofcomplex and at-risk patients through a qualityimprovement model in general practice.9
Opportunities, priorities and optionsPriorityPossible OptionsExpected OutcomePotential Lead GCPHN with partnersGeneral Practice Support – QualityImprovement Aged Care High numbers of preventable hospitaladmissions for older adults are recordedfor Chronic Obstructive Pulmonary Disease(COPD), urinary tract infections, angina andheart failureLack of established clinical coordinationtools and processes that result infragmentation of the local health system inpatient centred care –management and problematic after-hoursmanagementLow use of advanced care directives,plans and deficits in confidence andcapacity of staff to provide adequateand/or quality palliative care.Over 80% of residents in residential agedcare presenting with increasing complexityof care, including dementiabehaviour management, mental health,palliative and end of life care.Limited uptake of existing Education,training and resources to RACF’s, GPs andhealth care professionals in earlyidentification and management ofPalliative Care – End of Life.Limited capacity to provide a coordinatedand sustained coverage for palliative andend of life care within RACF’s out of hours.Quality improvement activities (tier 3) ingeneral practice support to include preventionas a potential focus area including recall andreminder of potentially eligible patients forhealth checks and referral to lifestylemodification programs.Enhanced Primary Care In RACFs Engage RACF staff to “champion” andsupport GPs to drive comprehensivemultidisciplinary care planning includingcompletion and use of advance careplanning utilising evidenced basedpathways and resources (including MyHealth Record).Embedding RACGP Silver Book guidelinesby providing access to a simplified cycle ofcare and decision support tools aligned tothe guidelinesProvision of education and training tosupport General Practitioners and RACFClinical Nurses and other RACF staff on: Qld End of Life Care planning andadvanced care planning. ISBAR clinical communication tool Use of My Health Record Development of strong partnerships withcommunity palliative care supports andservices and GPsImplementation and adoption of clinicalguidelines and protocols focused on keybest practices for generalist primarypalliative care within RACFsEngagement of RACF staff in training toincrease role appropriate competence inprimary palliative care skillsEnhanced clinical competency ofprofessionals within RACF in primarypalliative care managementIncreased awareness of palliative careclinical management and its integrationinto patient centred careDecrease in avoidable admissions toemergency departmentIncrease the number of Advance CarePlans and uploads to My Health Record.After hours advice and supportProvide a point of contact for RACF clinical staffto communicate with expert clinical staff toprovide advice and guidance to facilitate analternative to hospital transfer for acute,subacute and outpatient services and tofacilitate early and proactive planning oftransfers between GCHHS and RACFs.Gold Coast Health / other contractorDementia advice and support10
Opportunities, priorities and optionsPriorityPossible OptionsExpected OutcomePotential LeadExplore opportunities to build capacity in thesector to deliver improved care particularly forpeople with increasing complexity of careneeds, specifically behaviour management forpeople with dementia.Mental Health and wellbeing forRACF residentsExplore opportunities to build capacity in thesector to deliver improved mental health andwellness services in RACFs.Palliative Care ooooMaintaining the role of GPs incoordinating care for palliative patients isimportant to clinicians, consumers andcarers but this is difficult because:Some GPs and other primary careproviders may not regularly providepalliative care, influencing levels ofknowledge and confidenceLow levels of uptake and awareness ofexisting palliative care-related trainingand information resourcesCare coordination involving a person’sdifferent care providers and family isseen as important but can be difficultdue to funding arrangements and lackof dedicated resources to operationallysupportGPs experience challenges in makingpalliative care-related attendancesparticularly in the after-hours perioddue a range of factors including MBSpayments, capacity, limited access toinformation on currenttreatment/medications. For RACFsthere are also issues with accessingfacilities, coordination with onsitePrimary Health Palliative CareProject:Support for general practice to deliver palliativecare services Web based platform providing generalpractitioners with easy access to localisedinformation and existing evidence basedresources Care coordination with specialist palliativecare services and other members of MDTincluding optimum business processes (e.g.MBS item numbers) Training and education Trialling a GP Palliative Care Network forRACF’s which will support GPs interested inproviding quality palliative care, acceptingtransfer of care from other GPs, etc. Ifsuccessful, this approach will be extendingacross the district Developing shared care palliative caremodels with GPs providing most of the care,supported by ready access to specialists asneeded Ongoing educational opportunities for GPsprovided by the GCH Palliative Care Servicethrough annual in-service programs aboutsymptom management and medication, anduse of Program in the Experience of theGCPHN through Greater Choices for At HomePalliative Care with Gold Coast Health and otherkey stakeholders Improved practical advice and support forfamilies Improved awareness by health,community and aged care providersregarding family access to bereavementsupport.11
Opportunities, priorities and optionsPriority nursing staff and communication withdeputising services.Fatigue and burnout for families supportingloved ones at home is a significant issue,particularly those with limited practical andsocial supportThere is low uptake, awareness andconfidence reported for advance careplanning amongst both service providers andcommunity members.Effectiveness of local palliative care servicesin an inpatient setting typically exceedspatient outcome benchmarks, but achievingsimilar outcomes in the community setting ischallenging due to limited resourcing.Limited funding is available to supportcommunity services to provide after-hours inhome care, offer respite nursing support orpurchase appropriate equipment to enablepalliative care to be provide in a patient’shome (including residents of RACFs)Families report difficulty with understandingand navigating the palliative journey of lovedones including equipment requirementsPossible OptionsExpected OutcomePalliative Approach (PEPA). This provides GPswith an opportunity to work in palliative careunits. Strengthening the approaches used by GPsto advance care planning and exploring waysto involve practice nurses in advance careplanning and ongoing care Providing education to community andhospital pharmacists about current palliativecare medications, dosing regimens and sideeffects. Increased network of volunteers tosupport palliative care patients and theircarersIncreased knowledge and uptake ofAdvance Care Plan (ACP)Improved health, community and agedcare provider understanding of end-of-lifecare, and appropriate referrals to specialistpalliative care Commission suitable service provider to recruit,train, manage and provide ongoing support tovolunteers to support palliative patients andcarers with appropriate tasks and activities.The generalist healthcare workforcesupported and mentored to increasecapacity, knowledge and skills Community Awareness andEducation Workforce better equipped to support anageing populationImproved public understanding of end-oflife and palliative careIncreased uptake of ACPPalliative Care Volunteers Network Potential LeadModest media campaign and leveragingcommunity engagement opportunities toencourage people to talk more openly aboutdying, death and bereavement, and to makeplans for the end of life inclusive of AdvanceCare Plans.Enhanced Primary Care System navigation for people requiringpalliative care and primary care providerssupporting them with a focus on proactivecoordinated care.Agreed pathways developed andevaluated that provides triage,consultancy, clinical support, and advicefor patients, carers , clinical staff and GPs,so patient care can be delivered in thefacility where appropriate, and transfer tohospital is avoided.12
Opportunities, priorities and optionsPriorityPossible Options Expected OutcomePotential LeadTraining and education forimplementation of clinical carecoordination to GPs and MDSDevelop a regional palliative patientcentered management strategy andprocess that can be implementedregionallyIn consultation with local partners developa quality improvement system to bettersupport general practitioners ensuringcoordinated care for their palliative andend of life patientsDedicated support for GP practicesincluding services to enhance palliativecare co-ordination and to develop andimplement comprehensive proactive careplans.13
Primary Mental Health Care (including Suicide Prevention)Opportunities, priorities and optionsPriorityPossible OptionsExpected Outcome
the Gold Coast particularly h interland, Surfers Paradise and Mudgeeraba - Tallebudgera. Lower rates of HPV vaccination in Gold Coast compared to the national figure. Higher rates of hospitalisation for pneumonia and influenza in Gold Coast compared to the national figure.