Transcription
S Sileno, S Beji,M D’Agostino et al.3:1miRNAs in psoriasis andcardiovascular riskR49–R68REVIEWmicroRNAs involved in psoriasis andcardiovascular diseasesSara Sileno1,*, Sara Beji1,*, Marco D’Agostino1,*, Alessandra Carassiti1, Guido Melillo2 and Alessandra Magenta31IstitutoDermopatico dell’Immacolata, IDI-IRCCS, Experimental Immunology Laboratory, Via Monti di Creta, Rome, Italyof Cardiology, IDI-IRCCS, Via Monti di Creta, Rome, Italy3Institute of Translational Pharmacology (IFT), National Research Council of Italy (CNR), Via Fosso del Cavaliere, Rome, Italy2UnitCorrespondence should be addressed to A Magenta: ale.magenta@gmail.com*(S Sileno, S Beji and M D’Agostino contributed equally to this work)AbstractPsoriasis is a chronic inflammatory disease involving the skin. Both genetic andenvironmental factors play a pathogenic role in psoriasis and contribute to the severityof the disease. Psoriasis, in fact, has been associated with different comorbidities suchas diabetes, metabolic syndrome, gastrointestinal or kidney diseases, cardiovasculardisease (CVD), and cerebrovascular diseases (CeVD). Indeed, life expectancy in severepsoriasis is reduced by up to 5 years due to CVD and CeVD. Moreover, patients with severepsoriasis have a higher prevalence of traditional cardiovascular (CV) risk factors, includingdyslipidemia, diabetes, smoking, and hypertension. Further, systemic inflammationis associated with oxidative stress increase and induces endothelial damage andatherosclerosis progression. Different miRNA have been already described in psoriasis,both in the skin tissues and in the blood flow, to play a role in the progression of disease. Inthis review, we will summarize and discuss the most important miRNAs that play a role inpsoriasis and are also linked to CVD.Key Wordsff psoriasisff microRNAsff cardiovascular diseasesIntroductionPsoriasis is a complex and chronic inflammatory diseaseaffecting 2–3% of the world’s population (1). The etiologyof psoriasis is complex, and still debated, as the disorderis caused by the interaction among multiple genes, theimmune system and environmental factors (2, 3).From a dermatological point of view, psoriasisis characterized by hyperproliferative epidermis andcutaneous lymphocytic infiltration that can also involvejoints causing a form of arthritis, known as psoriaticarthritis (PsA) (3).A prominent role is played by the increased risk inthese patients of major adverse cardiovascular events:this evidence has received increasing attention in the lasthttps://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2021 The authorsPublished by Bioscientifica Ltddecades (4, 5). This finding cannot be explained only onthe basis of high prevalence of traditional cardiovascularrisk factors seen in psoriatic patients (6); additional andindependent factors such as the systemic inflammationassociated with psoriasis, the presence of psoriasis-relatedcomorbidities (7, 8) and the atherogenic side-effects ofsystemic therapies for psoriasis have also been reported (9).Atherosclerosis and inflammation inpsoriatic patientsAmple research work has demonstrated that inflammationis a key driver of atherosclerosis.This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
S Sileno, S Beji,M D’Agostino et al.Indeed, the risk of cardiovascular events is notsufficiently indexed by cholesterol and other traditionalrisk factors. High-sensitivity C-reactive protein (hsCRP)and interleukin-6 (IL6) levels, despite significantreductions in low-density lipoprotein cholesterol (LDL-C)obtainable with maximal medical therapy, are associatedwith 'residual inflammatory risk'. Control of inflammationhas increasingly become a viable pharmacologic targetfor primary and secondary prevention of atheroscleroticdisease (10).The inflammatory process seen in psoriasis sharesmany features with atherosclerosis including T helper1-mediated inflammation, alterations in angiogenesis, andendothelial dysfunction that may link the pathogenesisof psoriasis with the development of atherosclerosis andcardiovascular disease (CVD) (11).The typical histological features of the psoriatic plaquewith dermal inflammation and leucocyte infiltration aresimilar to those of the atherosclerotic plaque. The theoryof 'two plaques for one syndrome' has been hypothesizedgiven the similarities in the molecular mechanisms andpro-inflammatory cytokine profile found in psoriaticlesions and those of atherosclerotic ones, with acomparable inflammatory infiltrate of T cells, macrophagesand monocytes (9, 12).Both atherosclerosis and psoriasis are characterizedby immune system activation, involving T helper-1, Thelper-17, regulatory T cells and inflammatory cytokinessuch as INFG, IL2, TNF and IL17 (13). These mediatorsplay a key role in the development of psoriatic plaques,stimulating angiogenesis and keratinocyte proliferationand promote insulin resistance, metabolic abnormalitiesand endothelial dysfunction, which contribute toatherosclerotic plaque formation and progression (14,15). In support of this theory, large epidemiologic studieshave found increased rates of cardiovascular mortality,myocardial infarction (MI) (4, 5), atrial fibrillation andstroke (16) among patients with both mild and severepsoriasis. Recent comprehensive meta-analysis andcohort studies have confirmed that the association isstatistically significant (16). For a definitive evaluationof the association, more long-term prospective studieswill be needed.Psoriatic patients, therefore, appear to have a shorterlife expectancy, estimated as approximately 5 years (17).These subjects have increased prevalence of traditionalcardiovascular risk factors such as diabetes, hypertension,dyslipidemia, tobacco use and obesity (7, 8). Psoriasis, asalready pointed out and mainly if severe, appears to be anindependent risk factor for atherosclerotic CVD, as the riskhttps://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdmiRNAs in psoriasis andcardiovascular risk3:1R50persists even after adjusting for the traditional risk factors,probably due to the role that systemic inflammationplays in determining premature atherosclerosis in thesepatients (4, 5).The impact of psoriasis duration on aging andcardiovascular riskEstimation of cardiovascular risk based on the traditionalscore system has limitations in peculiar clinical contexts.These scores are known to underperform becausetraditional cardiovascular risk factors do not fully explainthe increased cardiovascular risk in patients with psoriasis.Consequently, cardiovascular risk is often underestimatedin these individuals (18).Although the relative risk of major adverse clinicalevents is greater for young patients with severe psoriasisvs old ones with mild disease, the greater populationprevalence of mild psoriasis translates into a greaterpopulation-attributable risk of mild psoriasis for bothMI and stroke. These findings emphasize that all patientswith psoriasis, rather than only young patients with severepsoriasis, should be educated regarding the increased riskof CVD.In addition, the risk of MI in psoriatic patientsaged between 30 and 40 years vs tose between 50 and 60years with a long history of psoriasis was compared (13).Attributable risk and excess risk calculated based on theadjusted relative risk of MI were much higher in the oldergroup being roughly 70-fold higher.Patients with psoriasis were more likely to havecoronary artery disease (CAD) as visualized on coronaryangiogram. This association was still evident after adjustingfor established cardiovascular risk factors, leading theauthors to conclude that psoriasis is independentlyassociated with the presence of CAD (19). Finally, a strictcorrelation between the duration of psoriasis and theextension of CAD exists.microRNA involved in psoriasis and CVDmiRNAs are shortnon-coding RNAs that inhibit translation and/or inducedegradation of target messenger RNAs (mRNAs) (20).The following miRNAs (summarized in Table 1) are themost important miRNAs modulated in psoriasis that arealso involved in CVD.miR-200 familymiR-200 family is composed of five members (i.e. miR200a,miR-200b, miR-200c, miR-429 and miR-141). This miRNAfamily has been shown to be induced in lesional skin (LS) ofThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
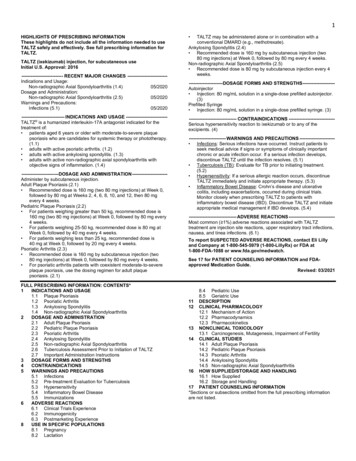
https://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdHumanHumanHumanHumanMouseHumanHumanHumanHuman, mouseHumanHuman, nMouseHumanHumanHumanLS vs NL, plasmaT cellsLS vs NLLS vs HS, plasmaAtherosclerotic plaqueCarotid plaque, plasmaPlasmaLS vs NLHeartSerumHeartAtherosclerotic plaque, plasmaAortasLS vs NSCardiomyocytesSerum of CADCardiomyocytesLS vs HSVSMCPlaqueHeart/PlasmaHeartSerumBloodPlasma of PsA vs emoral anLS vs NL, LS vs HS, plasmaECsCarotid plaques, atedModulationSIRT1, OD2; SPRY2RECK, knownUnknownRHOA; CDC42; NELFA/WHSC2MMP9UnknownABCA1; ABCG1; ZEB1ZEB1UnknownABCGA1; ABCG1UnknownUnknownUnknownUnknowneNOS; SIRT1; FOXO1; ZEB1eNOS; SIRT1; FOXO1; ZEB1ZEB1Targets3:1(Continued)(67, )(47)(48)(49)(36)(37, 38)(39)(40)(43)(45)(33, 25)(34)(29)(32)(21)(21)(22)(21)(23, 24)(25)(35)ReferencesmiRNAs in psoriasis andcardiovascular riskCardiac O2AtherosclerosisFamilial 200b, miR-141, -33a/bAtherosclerosisFamilial hypercholesterolemiamiR-133aPsoriasisMIAMI, unstable anginaCardiac hypertrophyAtherosclerosisThoracic aortic aneurysmmiR-135bPsoriasisMIAtherosclerosisCardiac osclerosisCardiac iRNAs modulated in psoriasis and CVD.miRNAs/ROS source or diseaseTable 1S Sileno, S Beji,M D’Agostino et al.R51This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
sAtherosclerosisCardiac hypertophymiR-378a*PsoriasismiR-9PsoriasisDeep vein thrombosisMSACSMICardiac iac hypertrophymiR-19aPsoriasisAtherosclerosisCardiac PsoriasisHFmiRNAs/ROS source or diseaseTable 1https://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdHumanMouseMouse, humanHumanMouseLS vs HS, hair rootsPlasma, atherosclerotic plaqueCardiomyocytesLS vs NL and vs HSAortic plaqueMouseMouseT umanMouseLS vs NLBloodCardiomyocytesLS vs NL and vs HSPBMCsValvular an, mouseMouseMouseLS vs NLVenous , humanMouseHumanKeratinocytes of LS vs NLLS vs HSHair SpeciesLS vs NLKeratynocites of LS vs NL and HSVSMCsPlaquesHeartSerum, LS vs HSPlasma of AMI with HF vs MIwithout HFTissue/organFERMT1, NUMBBAG1, MMP16(124)(129)(123, 124)(126)(127)(128)(131)(120)(120)(121)(122)(114, 116)(117)(118)(108)(111)(36, 100, 101)(102)(103)(36)(92)(93)(94, 95)(97)(96)(80, 81)(36)(80)(86)(87, 88)(89)(64, 75)(78)References3:1UpregulatedUpregulatedFERMT1, NUMBUnknownTLR4, IRAK1MCSF, RELBSUMO1MEK1, CYCLIN E1UnknownAPOC3CRISPLD2TNFHBP1ATROGIN1, MURF1, PDE5AIL17ADystrophinIGF1R; JAK2UnknownPDK1UnknownNFKB1ABCA1SDC2; OLR1FSTL1MyocardinVEGFUnknownUnknownIGF1; TLR8ABCG1; SIRPAMAPK1; KSR1; GRB2; IGF1RUnknownUnknownTargetsmiRNAs in psoriasis andcardiovascular pregulatedUpregulatedModulationS Sileno, S Beji,M D’Agostino et al.R52This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
ntifica.com esPlasma of PsACarotid plaques: symptomatic vsasymptomaticDiabetic plaqueDiabetic uman, pigT egulatedDownregulated(137)(139)(141)KLF4OPG, edUpregulatedmiRNAs in psoriasis andcardiovascular riskAortic plaqueCarotid regulatedUpregulatedUpregulatedHumanHumanHumanLS vs HSPlasma of unstable CADCarotid: symptomatic rosis(132)S Sileno, S Beji,M D’Agostino et al. 2020 The authorsPublished by Bioscientifica Ltd3:1R53psoriatic patients compared to non-lesional (NL) one (21).Further, miR-200c is the only one also induced comparedto healthy skin subjects (HS). The entire miRNA familywas assayed in the bloodstream of psoriatic patients, andmiR-200c and miR-200a were upregulated significantlycompared to healthy subjects. The correlation analysiswith psoriasis area severity index (PASI) and the durationof disease showed that only miR-200c expression levelspositively correlated with both, indicating that miR200c could be considered as an inflammatory biomarkerfor this disease (21). Moreover, miR-200c correlated withdifferent determinants of cardiovascular risk, such asrelative wall thickness (RWT), left ventricular (LV) mass,and E/e’ parameter, a marker of diastolic dysfunction (21).Circulating miR-200a correlated only with LV mass andaugmentation index, a marker of stiffness, although notsignificantly (P 0.06).These data indicated that miR-200c increases inplaques and plasma of psoriatic patients and could beinvolved in the establishment of inflammation and CVDin psoriasis.In another study, it has been shown that theupregulation of miR-200a in CD4 T cells may induceimmune dysfunction through Th17/Treg cells and relevantcytokines (i.e. IL17 and IL23) levels in psoriasis vulgarispatients and positively correlates with PASI (22).miR-200c was upregulated in endothelial cells (ECs)upon oxidative stress exposure and is responsible forapoptosis, senescence (23), nitric oxide (NO) decrease andreactive oxygen species (ROS) increase, and all featuresassociated with endothelial dysfunction (24). In particular,miR-200c targets zinc finger E-box binding homoeobox 1(ZEB1) protein, inducing apoptosis and senescence of ECs(23) and disrupts the autoregulatory loop existing amongSirtuin1 (SIRT1), endothelial nitric oxide synthase (eNOS)and forkhead boxO1 (FOXO1), directly targeting all ofthem, causing NO decrease and ROS increase (24).It is well known that endothelial dysfunctionplays a key role in unstable plaques genesis. In keepingwith this, miR-200c was increased in carotid plaquesof atherosclerotic patients, and it is higher in unstableplaques vs stable plaques (25).miR-200c was found to be elevated in the plasma ofpatients with atherosclerosis, although the circulatinglevels did not discriminate between stable or unstableplaques. Interestingly, the plasma levels were decreasedafter carotid endarterectomy (CEA), and after 1 month, thelevels of miR-200c were increased in patients with unstableplaques, whereas 1 month after CEA miR-200c levels werestill low in patients with stable plaques, indicating thatThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
S Sileno, S Beji,M D’Agostino et al.increased levels of miR-200c are most probably associatedwith endothelial dysfunction and inflammation (25).Interestingly, miR-200c levels positively correlatedwith biomarkers of plaque instability such ascyclooxygenase-2 (COX2), IL6, monocyte chemoattractantprotein-1 (MCP1), metalloproteinase (MMP) 1, MMP9 andnegatively correlated with stability biomarkers (i.e. ZEB1,eNOS, FOXO1 and eNOS).Interestingly, miR-200c positively correlated with twoimportant miRNAs, miR-33a/b (see following paragraph),which have been linked to atherosclerosis progression(26) and are key players of cholesterol homeostasis, sincethey are key regulators of high-density lipoprotein (HDL)cholesterol synthesis (27).In conclusion, the miR-200 family is increased inpsoriasis skin, and among its members, miR-200c plasmalevels correlate with cardiovascular risk and inflammatorybiomarkers (Fig. 1).miR-33a/bmiR-33a and miR-33b share the same seed sequence andare embedded in introns of sterol regulatory elementbinding protein (SREBP)2 and SREBP1 genes, respectively(28). SREBP genes are important transcription factorsthat regulate lipid metabolism, and their bexpression (28).miR-33a was found to be higher in plasma of patientswith plaque psoriasis compared to controls and correlatedmiRNAs in psoriasis andcardiovascular risk3:1R54positively with plasma insulin and the homeostaticmodel assessment (HOMA)-insulin resistance index value.Moreover, psoriasis patients displayed greater carotidintima-media thickness (IMT) than controls (29).miR-33 are known to directly target the cholesteroltransporter ATP-binding cassette transporter A1 (ABCA1)and ATP-binding cassette transporter G1 (ABCG1), proteinsimplicated in the efflux of cholesterol from macrophagesto generate HDL (27). miR-33a/b also regulate fatty acidoxidation and insulin signaling (30, 31).Given their role in cholesterol and lipid metabolism,different studies evaluated miR-33 inhibition in animalstudies. miR-33 inhibition has been shown to raise plasmaHDL-cholesterol and to protect from atherosclerosis inmice (32). miR-33 inhibition in non-human primatesupregulates the hepatic expression of ABCA1, increasingplasma HDL-cholesterol levels and suppressing the plasmalevels of very-low-density lipoprotein (VLDL)-associatedtriglycerides (33).Interestingly, as aforementioned, miR-33a and miR33b were found to be increased in carotid atheroscleroticplaques, suggesting their role in advanced atherosclerosisin humans (26).In keeping with this, miR-33a/b were also foundto be upregulated in plasma of children with familialhypercholesterolemia, a disease that causes atherosclerosisin the pediatric age. miR-33a/b positively correlated withtotal cholesterol, LDL-cholesterol, apolipoprotein B,glycemia and CRP (34). Moreover, these miRNAs correlatedalso with miR-200c plasma levels, and the extracellularFigure 1miR-200c in psoriasis and CVD. miR-200c isupregulated by reactive oxygen species (ROS) andis responsible for apoptosis, senescence,endothelial dysfunction, ROS increase and nitricoxide decrease, all features associated withatherosclerosis. Indeed, miR-200c increases incarotid plaques and plasma of atheroscleroticpatients vs healthy subjects and positivelycorrelates with plaque instability biomarkers (i.e.MCP1, IL6, COX2, MMP1, MMP9 and miR-33) andnegatively with stability biomarkers (i.e. SIRT1,FOXO1, eNOS and ZEB1). ROS modulation,endothelial dysfunction, cardiac remodeling andinflammation are also associated with psoriasis.Iin keeping with this, miR-200c is increased in LSvs NL and vs HS, and in plasma of psoriaticpatients. miR-200c correlates with PASI and theduration of disease and with determinants of CVD(i.e. LV mass, E/e’ and RWT) in psoriatic patients.https://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
S Sileno, S Beji,M D’Agostino et al.release of miR-200c was mediated by miR-33 since theoverexpression of miR-33a/b in vitro in different cells(i.e. ECs, hepatic cells and embryonic kidney cells) wasmediated by a ZEB1-decrease mechanism (35).The latter is a transcriptional inhibitor of miR-200c;hence, ZEB1-decrease causes an increase of both intracellularand extracellular miR-200c expression levels (35).A positive correlation between miR-200c and miR-33a/bwas also found in the plasma and plaques of atheroscleroticpatients as mentioned previously (25) (Fig. 2).Thus, a complex interplay among miRNAs ismost probably the basis of metabolic dysfunction andinflammation and oxidative stress increase in psoriaticpatients.miR-133amiR-133a was found to be downregulated in LS of psoriaticpatients compared to NS (36). miR-133a expression levelsincreased after treatment with biologics.Notably, miR-133a is muscle-specific miRNA, and it isinvolved in cardiac development and pathophysiology.Interestingly, miR-133a is downregulated in both theinfarcted area and the border zone both in humans, as wellas in experimental animals (37, 38).On the other hand, miR-133a levels in serum increasedsignificantly in patients with acute myocardial infarctionmiRNAs in psoriasis andcardiovascular risk3:1R55(AMI) or with unstable angina pectoris, and circulationincrease of miR-133a positively correlates with theinfarcted area (39).Indeed, miR-133a decrease is involved in cardiachypertrophy, and its overexpression inhibits hypertrophy(40). Moreover, miR-133a increase plays a major role inpreventing cardiac fibrosis in chronic heart failure (HF)(41), and its increase in adult cardiac progenitor cells (CPCs)improves cardiac function, decreasing fibrosis and increasingcardiomyocyte proliferation and vascularization (42).miR133a was found to be downregulated in plasma andin atherosclerotic plaques, and its decrease in vascular smoothmuscle cells (VSMCs) results in the inhibition of proliferationand in the induction of apoptosis via MMP9 (43).miR-133a has been shown to inhibit the osteogenicdifferentiation of VSMCs; therefore, its decrease inducesarterial calcification (44).Finally, miR-133a is also decreased in thoracic aorticaneurysms (TAA), and its decrease negatively correlateswith aortic diameters (45).Thus, miR-133a decrease in psoriasis could be involvedin the onset of different CVD.miR-135bmiR-135b was upregulated in LS compared to NS (46),and after treatment with biologics, miR-135b wasFigure 2miR-200c and miR-33 interplay in psoriasis andCVD. miR-200c and miR-33 positively correlate inplasma and plaques of atherosclerotic patients. Amolecular mechanism among miR-33a/b andmiR-200c increase does exist. Indeed, theoverexpression of miR-33a/b in vitro in differentcells (i.e. ECs, hepatic cells and embryonic kidneycells) causes the intracellular and extracellularincrease of miR-200c via a ZEB1-decreasemechanism. ZEB1, in fact, is a direct target of bothmiR-33 and miR-200c and a transcriptionalinhibitor of miR-200c. Hence, a ZEB1-decreasecauses upregulation of both intracellular andextracellular miR-200c expression levels. Anincrease of miR-200c in skin plaques and plasmaof psoriatic patients was also observed, and itpositively correlates with PASI index anddeterminants of CVD risk (RWT, E/e’ and LV mass).Interestingly, miR-33a was found to beupregulated in the plasma of psoriatic patientsand positively correlates with HOMA-insulinresistance index and cIMT. Therefore, a possiblelink in psoriasis could also exist among miR-33and miR-200c, contributing to the increase of CVDin these patients.https://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/02/2022 12:56:03AMvia free access
S Sileno, S Beji,M D’Agostino et al.downregulated, significantly returning to those levelsdetected in NS (36).After treatment with biologics, miR-135b levelswere associated with both PASI improvement and localinflammatory response decrease (36).Interestingly, in MI, miR-135b is downregulated,and its overexpression attenuates pyroptosis, a caspase1-dependent proinflammatory programmed cell death.Thus, miR-135b plays a protective role in MI (47).Moreover, miR-135b was found to be upregulated insera of atherosclerotic subjects with CAD compared tohealthy control subjects. Interestingly, miR-135b directlytargets myocyte enhancer factor 2C (MEF2C), whichplays an important role in promoting ECs and VSMCsproliferation and migration (48).Further, miR-135b is decreased in cardiac hypertrophy,and its overexpression is attenuated in an animal modelof hypertrophy by targeting L-type calcium channelCACNA1C, a protein involved in cardiac hypertrophysignaling (49).miR-135b upregulation in psoriasis resembles themodulation in atherosclerosis, whereas it is modulated inCVD differently.miR-21miR-21 was significantly upregulated in LS of patientswith psoriasis compared to healthy skin (50), and narrowband UV phototherapy treatment decreased its expressionin skin biopsies derived from psoriatic patients (51).Moreover, a specific single nucleotide polymorphism in3'UTR of integrin alpha-M (ITGAM) is associated with abinding site improvement for miR-21 that can manifestan aberrant function of innate immune cells, resulting inhigher risk insurgence of psoriasis in women (52). Otherdata suggest that miR-21 upregulation could increasethe inflammatory process, by suppressing the apoptosispathway in dermal T-cells of psoriatic patients (53). Arecent study has shown that the interaction betweenmiR-21 and lncRNA maternally expressed gene3 (MEG3)can influence the apoptotic axis in human psoriatickeratinocytes (54).miR-21 inhibition was able to reduce psoriaticphenotype in a mouse model of psoriasis (55).miR-21 has been widely studied in CVD. miR-21 wasshown to be upregulated by oxidative stress in rat VSMCs.Its upregulation was found to be protective from apoptosissince programmed cell death 4 (PDCD4) is a direct target ofmiR-21 (56). PDCD4, in fact, is a pro-apoptotic protein thatinhibits the activity of the transcription factor AP-1 (57).https://vb.bioscientifica.com https://doi.org/10.1530/VB-21-0007 2020 The authorsPublished by Bioscientifica LtdmiRNAs in psoriasis andcardiovascular risk3:1R56The latter is a signaling molecule, which determines cellfate based on extracellular stimuli, including ROS.Interestingly, miR-21 is upregulated by shear stress andalso protects ECs from apoptosis, increasing eNOS and NOproduction (58).miR-21 upregulation also occurs in atheroscleroticplaques, decreasing the function of superoxide dismutase-2(SOD2) antioxidant enzyme and targeting a negativeregulator of the branching morphogenesis, sproutyhomolog 2 (SPRY2). This, in turn, leads to the activation ofERK/MAP kinase provoking ROS increase and angiogenicprogenitor cell (APC) migratory defects (59).Moreover, miR-21 expression is increased in myocardialtissue and plasma of patients with aortic stenosis (60),in a mouse model of cardiac hypertrophy induced byaortic banding, and in neonatal rat cardiomyocytesafter stimulation with hypertrophic agents (61); miR21 upregulation in cardiac hypertrophic growth causedSPRY2 downregulation, enhancing the formation ofvarious cellular protrusions and gap junction remodeling,enhancing conduction velocity (62).miR-21 circulating levels have been also usedas excellent biomarkers for the diagnosis of heartdysfunction (63).In conclusion, miR-21 increase in psoriasis could be apossible link to CVDs such as atherosclerosis and cardiachypertrophy.miR-22miR-22 circulating expression levels were significantlydownregulated in the blood of patients affected bypsoriasis vulgaris compared to healthy subjects (64). Inaddition, plasma levels of miR-22 were evaluated in PsAand ankylosing spondylitis, two chronic inflammatoryrheumatic disorders. miR-22 circulating expressionwas found to be markedly lower in PsA subjects than inankylosing spondylitis patients (65).Psoriasis is widely regarded as a classical autoimmunedisease. Interestingly, it has been shown that miR-22 levelsare upregulated in the spleen and spinal cords of mice thatdeveloped autoimmune encephalomyelitis, and its highexpression in inflammatory Th17 cells could protect micefrom autoimmunity (66).miR-22 also plays a pivotal role in CVD. miR-22 is apro-hypertrophic miRNA, and in fact, miR-22 levels wereincreased in cardiomyocyte hypertrophy and in differentca
non-coding RNAs that inhibit translation and/or induce degradation of target messenger RNAs (mRNAs) (20). The following miRNAs (summarized in Table 1) are the most important miRNAs modulated in psoriasis that are also involved in CVD. miR-200 family miR-200 family is composed of five members (i.e. miR200a, miR-200b, miR-200c, miR-429 and miR-141).