Transcription
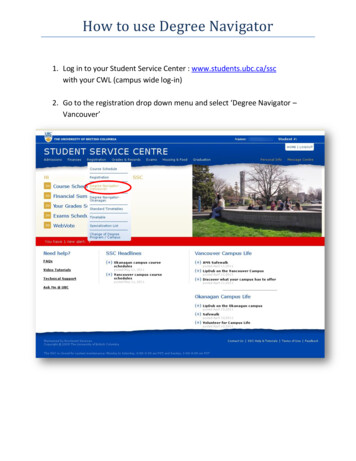
Recovery Support Navigator (RSN)and Recovery Coach (RC)Provider TrainingRegistration and Billing for MBHPJune 20181
Objectives Overview of billing codes and modifier requirement used byBeacon Verifying Member eligibility Accessing ProviderConnect Claim submissions Contact information Resources and supports for Members Questions2
Overview of Billing Codes and ModifierRequirementRecovery Support Navigator(RSN)Recovery Coach(RC)HCPCS CodeH2015H2016ModifierHFHMPlace of serviceSame as CSPSame as CSPBilling structure15-minute unit fee for serviceDaily case ratePrior authorizationNoneNoneRegistrationparameters180 units over 90 days90 units over 90 days3
Other Information The Recovery Support Navigator and Recovery Coachperformance specifications and medical necessity criteria canbe found on our websites, www.masspartnership.com orhttps://provider.beaconhs.com. The MBHP Benefit Service Grid on www.masspartnership.com,or the provider manuals on www.beaconhealthoptions.com areuseful tools for billing questions such as acceptable place-ofservice codes, covered diagnoses, etc.4
Verifying Member Eligibility5
MassHealth Eligibility Verification System Per the provider contracts, Beacon providers are required toverify Member eligibility on every date of service. Member eligibility is verified through the MassHealth EligibilityVerification System (EVS), accessed through the MassHealthVirtual Gateway, www.mass.gov (search for “virtual gatewaylogin”). Once logged in to the Virtual Gateway, providers can accessthe Provider Online Service Center (POSC), where EVS islocated. Beacon providers receive a data collection form in the NewProvider Welcome Packet. That form must be filled out andmailed/faxed to MassHealth to establish login credentials.6
MassHealth Virtual Gateway7
Provider Online Service Center (POSC)8
MassHealth EVSFinding Member EligibilityInformation: Click on “Manage Members” Then “Eligibility” Then “Verify Member Eligibility”9
MassHealth EVS (continued)Search criteria: MMIS/SSN/ orName and DOB One month maximumdate range Unable to searchfuture dates10
MassHealth EVS (continued) Click on“Eligibility”11
MassHealth EVS (continued) Click on“Date Range” toexpand information Look for MBHP,BMCHP, Fallon,NHP, or SWHto confirm eligibility12
Accessing ProviderConnect13
ProviderConnect RegistrationProviders who do not have access or need additional access to log on toProviderConnect can register with this interactive form.14
Accessing ProviderConnecthttps://www.masspartnership.com15
Logging into ProviderConnectProviders can havemultiple log ins fordifferent staff.16
Registration Procedures17
RSN and RC Member Registration Requests MBHP is informed of a person beginning treatment via acomputer application called ProviderConnect. Providers complete and submit a request form online. All initial requests for RSN services should be for 180 unitsover a 90-day period (1 unit 15 minutes). All initial requests for RC services should be for 90 units over a90-day period (1 unit 1 day). Subsequent or additional requests beyond the initial registrationwill be reviewed by MBHP staff and may require additional clinicalreview.18
All MBHP Members Require Registration There is a 14-day window for submitting a registration request. Up to 7 days before service start date Up to 7 days after service start date19
Authorization RequestOnce you are logged into ProviderConnect, click “Enter an Authorization Request.”20
Disclaimer21
Search a Member22
Member Demographics23
Select Service Address24
RSN/RC Request25
RSN/RC Request (continued)26
RSN/RC Request (continued)27
Behavioral Diagnosis28
Behavioral Diagnosis (continued)Enter a diagnosis code.29
Medical Diagnosis30
Social Elements Impacting Diagnosis31
Submit Request32
Registration Approval33
After 90 Days/180 Units, Submit a Concurrent Request There is a 14-day window to submit a concurrent request. Up to 7 days before Up to 7 days after Tailor the size of the request to meet the ongoing needs of theMember.34
Concurrent Request35
Concurrent Request (continued)36
Concurrent Request (continued)37
Concurrent Request (continued)Use the narrative box for any additional information, then clicksubmit.38
Concurrent Clinical Questions for RSN Is the Member participating in services? How frequently are you engaging with the Member? Have you integrated any other therapeutic or community-basedcare into the Member’s care plan? If so, what supports haveyou put into place? Does the Member have a Recovery Coach? If yes, are youcoordinating care with him/her? If the Member has an opiate use disorder, have you providededucation about the potential benefits of medication-assistedtreatment? If the Member is willing, has the Member been referred?39
Concurrent Clinical Questions for RSN (continued) Has the Member relapsed since starting services? If yes,describe actions taken and if additional services have beenconsidered? Is the Member actively addressing components of his/her careplan and making adjustments as needed? Describe the Member’s living environment. In addition, there are narrative boxes to include a treatmentplan, the Member’s progress towards goals, and a dischargeplan.40
Concurrent Clinical Questions for RC Is the Member participating in services? How frequently are you engaging with the Member? If there has been insufficient engagement with the Member,what is the plan for increasing engagement with the Member ifcontinued services are authorized? Have you integrated any other therapeutic or community-basedcare into the Member’s care plan? If so, what supports haveyou put into place? What are the Member’s current strengths? What are the Member’s current areas of growth/focus?41
Concurrent Clinical Questions for RC (continued) Is the Member actively addressing components of his/herwellness plan and making adjustments as needed? Has the Member relapsed since starting services? If yes,describe actions taken and if additional services have beenconsidered? Describe the Member’s living environment. In addition, there are narrative boxes to include a wellnessplan, the Member’s progress towards goals, and a dischargeplan.42
PC TipWhen filling out any of the authorization request forms, there isan option to save the request as a draft, so you can complete itlater. Use the Save Request as Draft button located in the upperright corner of each screen.Keep in mind, the saved draft has not been submitted to MBHP.You must remember to go back to it, complete the form, andsubmit it.43
Concurrent Request (continued)If the request requires additional review, you will see this message:44
RSN or RC Concurrent Requests When contacted by the designated RSN and RC Reviewer,Linda Plonowski-Bollea, it is important to contact the CareManager as soon as possible for MBHP to make a timelydetermination. Reluctance in contacting Linda Plonowski-Bollea can result inalternative decisions to the requests for additional coverage. When and if a review time has been scheduled, it is essential tobe available and on time for your appointment, with allnecessary concurrent review information.Linda Plonowski-Bollea can be contacted at (617) 790-4156.45
Claim Submission - MBHP46
Direct Claim Submission Provides ability to enter a claim directly into ProviderConnectportal without using special software Expedites processing of the claim and payment It is possible to submit paper claims.47
Direct Claim Submission (continued)To start a claim, click “Enter a Claim.”48
Direct Claim Submission (continued)49
Direct Claim Submission (continued)50
Direct Claim Submission (continued)51
Direct Claim Submission (continued)Enter the service code, then click “Add Service Line.”52
Direct Claim Submission (continued)Before you submit, if you want to add an EOB document to the claim,click “Upload File.”53
Summary Page54
Contract InformationEDI Helpdesk(ProviderConnect Technical Questions)Monday through Friday, 8 a.m. - 6 p.m. ETPhone: (888) 247-9311Email: e-supportservices@beaconhealthoptions.comMBHP Main Office and PCC Plan Hotline:1-800-495-0086 or (617) 790-4000Monday through Thursday 8:30 a.m. – 5 p.m.Friday 9:30 a.m. – 5 p.m.55
Additional Resources56
Additional Supports for Members Emergency Services Program (ESP) Care management Behavioral health services Outpatient Residential Rehabilitation Services (RRS) Structured Outpatient Addiction Program (SOAP) OTP/Medication for Addiction Treatment57
Description ofEmergency Services Program (ESP) The purpose of ESP is to respond rapidly, assess effectively,and deliver a course of treatment intended to promote recovery,ensure safety, and stabilize the crisis. Services allow a Member to receive medically necessaryservices in the community, or if medically necessary, in aninpatient or 24-hour diversionary level of care. ESP is for Members of all ages experiencing a behavioralhealth crisis. ESP is directly accessible to Members seeking behavioralhealth services on their own or referred by any other individualor resource. ESP is available 24 hours per day, 7 days per week, 365 daysper year. Services are community-based to bring treatment to Membersin crisis.58
Components ofEmergency Services Program (ESP) Crisis assessmentShort-term crisis counseling/interventionCrisis stabilizationDisposition and referralsStaffing disciplines Master’s, doctoral, RN-level clinicians Bachelor’s-level staff Certified Peer SpecialistTo locate an ESP in the Member’s area, call1-877-382-1609 and enter the zip code where the Member islocated.59
Care ManagementAn enhanced care management program offered to Memberswith complex medical, mental health, and/or substance usedisorders60
Massachusetts Behavioral Health Access(MABHA) Website Bed availability in “real time” Provider contact information and referral procedures Accepted insurances Level of care descriptions Accessible to the public Go to www.mabhaccess.com61
MABHA Website62
MABHA Website (continued)Select the service you are searching for from the gray toolbar orfrom the blue service boxes.63
Find an MBHP-Contracted ProviderGo to www.masspartnership.com PCC Plan Providers Find aProvider Find a Behavioral Health Provider64
When filling out any of the authorization request forms, there is an option to save the request as a draft, so you can complete it later. Use the Save Request as Draft button located in the upper right corner of each screen. Keep in mind, the saved draft has not been submitted to MBHP. You must remember to go back to it, complete the form, and