Transcription
Louisiana Hospital EmergencyPreparedness and ResponseAugust 2007Louisiana Hospital Emergency Preparedness and Response PlanDesignated Regional CoordinatorsEmergency Operations PlanWORKING DRAFT 8/17/071
Table Of ContentsI.Introduction and BackgroundII.Louisiana Hospital Emergency Preparedness and ResponseA. Infrastructurei. NIMS Complianceii. Regional structuresiii. State and federal InterfaceB. Critical Initiativesi. Communicationii. Patient Movement Processiii. Medical Queue for Mass Evacuationiv. Emergency Codesv. Special Needs ShelteringIII.Individual Hospital ResponseAppendicesAppendix A – Map of Louisiana Planning RegionsAppendix B – Designated Regional CoordinatorsAppendix C– Hospitals by Region and TypeAppendix D – Louisiana Emergency Support Function 8 – Healthand Medical Incident Command StructureAppendix E– Emergency Patient Transfer ProcessAppendix F - NIMS Compliance (to be developed)Appendix G - Interim Patient Tracking SystemAppendix H- Emergency Support Function 8 Hospital EmergencyPreparedness and Response for HurricanesAppendix I – Hospital CEO ChecklistAppendix J - Medical Institutional Evacuation PlanLouisiana Hospital Emergency Preparedness and ResponseI. Introduction and BackgroundAs in other parts of the nation, Louisiana is susceptible to disasters, both natural andman-made, that could exceed the resources of any individual hospital. A disaster couldresult from incidents generating an overwhelming number of patients, from a smallernumber of patients whose specialized medical requirements exceed the resources ofthe impacted facility (e.g., hazmat injuries, pulmonary, trauma surgery, etc.), or fromincidents such as building or plant problems resulting in the need for partial or completehospital evacuation.WORKING DRAFT 8/17/072
Impact of 2005 Hurricane SeasonHurricane Season 2005 was the most active and deadly in our nation’s history.Louisiana was hit by one tropical storm and four hurricanes: Cindy, Dennis, Katrina andRita. All of Louisiana’s coastal areas were impacted. As the result of HurricanesKatrina and Rita 58 hospitals were evacuated (19 remain closed to this date). Thatevacuation involved the transportation of more than 15,000 hospital patients, staff, andvisitors. All state and local resources were impacted. Federal support via the NationalDisaster Medical System was required. More than 1200 individuals lost their lives as aresult of the storms.With federal funding provided through the Health Resources Services Administration(HRSA) Hospital Bioterrorism Grant Program, Louisiana established an infrastructure tofacilitate:o Development of a plan of action in response to the identified needso Upgrade the ability of hospitals and other healthcare entities to respond tobiological events, ando Development a multi-tiered systems in which local health care entities areprepared to triage, treat, stabilize and refer multiple casualties to identifiedcenters for care.Individual hospitals developed inter-hospital plans to upgrade resources required tosupport an emergency response.II. Hospital Emergency Preparedness and ResponseA. Infrastructurei.Adoption of National Incident Management System (NIMS)NIMS was developed as a comprehensive national approach to incident management,applicable at all jurisdictional levels and across functional disciplines, to further improvethe effectiveness of emergency response providers and incident managementorganizations across a full spectrum of potential incidents and hazard scenarios.Louisiana has adopted NIMS at all government departments and agencies as well as inthe private public partnership of health care providers networked through the LouisianaHospital Emergency Preparedness and Response (LHEPR).Further, LHERPencourages NIMS adoption by associations, partners, and suppliers.ii.Regional structuresTo facilitate the multi-layered response, nine (9) planning regions for private and publichospitals were identified. These regions correspond with those used by LouisianaDepartment of Health and Hospitals Office of Public Health.WORKING DRAFT 8/17/073
Appendix A includes a map of the Louisiana Emergency Preparedness Responseregions.All hospitals “belong” to a region and have participated in the development of regionalplans. Hospitals have been asked to identify a point of contact, known as the HospitalEmergency Preparedness Coordinator.Leadership for Louisiana Hospital Emergency Preparedness and Response is providedthru hospital volunteers known as Designated Regional Coordinators (DRCs). Theprimary responsibilities for the DRCs are:o To serve as the liaison for hospitals with other health-related entities (i.e.Office of Pubic Health, Bureau of Emergency Medical Services) and onbehalf of hospitals with non-health related entities (i.e) Office of EmergencyPreparedness.o To support the patient transfer process during a declared state ofemergencyo To facilitate the identification of a medical evacuation queue during adeclared state of emergency.o To facilitate the development and implementation of regional and Interhospital emergency preparedness plans for designated regions in the Stateof Louisiana.o To lead the region’s process for development of, testing of, continuousimprovement of and management of regional hospital response toemergency situation:o To be the leader for the region during a statewide emergency in whichhospitals are tasked to respond.Appendix B provides a listing of FY 05-06 Designated Regional Coordinators.Louisiana’s hospitals provide various levels of care. A classification system of hospitalswas identified based on capabilities was identified. Hospitals serve voluntarily as one ofthree levels:o Designated Regional Hospitals (DRH) hospitals are larger acute care facilities withemergency room capabilities and many subspecialty services. They servevoluntarily and have agreed to provide additional capacity and resources in the initialemergency response of a mass casualty or event.o Tier 1 Hospitals: Hospitals with emergency department capabilities 24/7.o Tier 2 Hospitals: Hospitals that do not provide emergency room capabilities andare more single service in nature such as psychiatric, rehabilitation, and/or long termacute service.WORKING DRAFT 8/17/074
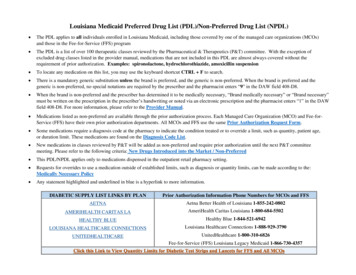
Appendix D provides a listing of Louisiana’s hospitals by region and level of service, andtheir Emergency Preparedness Coordinator.Most of Louisiana’s HRSA Hospital Bioterrorism Grant Program funds have beendirected to hospitals.Louisiana has received HRSA grant funds to improvecommunications, surge capacity, isolation capabilities, coordination, planning, training,and purchase pharmaceuticals, personal protective equipment, decontaminationequipment enhancing our emergency response capabilities.iii. State and Federal InterfaceThe Louisiana Department of Health and Hospitals, Office of Emergency Preparednessprovides coordination on behalf of the State of Louisiana and all other state agencies, tothe federal government through Emergency Support Function (ESF) 8 - Health andMedical Services, and the Louisiana Hospital Emergency Preparedness and Response.An Incident Command Structure for Emergency Support Function 8 – Health andMedical is included in Appendix E.NIMS Compliance will be addressed in Appendix F.B. Critical InitiativesSeveral critical initiatives have been developed by the Louisiana Hospital EmergencyPreparedness and Response to support emergency preparedness: Initiatives include:o Enhancing communication capabilities and interoperability for all hospitals; ando The development of a patient movement process to facilitate movement ofpatients during a declared state of emergency.o Identification of a process to establish a medical queue during a massevacuation.i. CommunicationEMSystemLouisiana hospitals implemented the emergency preparedness tool, EMSystemResource Tracking. Hospitals participating in the EMSystem have been asked to reportas needed:--- status of operations (open, limited, or closed)--- availability of beds by category (M/S, ICU, ped, psych, etc); and--- other resources that may be needed by hospitals in an emergency (blood products,fuel, pharmaceuticals, personnel, etc.)This data warehousing includes inventories of available resources against whichincoming data can be continuously compared, and that resources can be quicklyassessed and distributed.WORKING DRAFT 8/17/075
Hospitals and other health care entities may receive an initial alert from the Governor’sOffice of Homeland Security and Emergency Preparedness (GOHSEP) after identifyinga potential threat through the use of blast fax and email. GOHSEP will coordinate therelease of the alert with ESF 8 Incident Command.EMSystem also includes an alert and notification components allowing ESF 8 IncidentCommand structures to send request submission of specific information enablingcoordination of activities during an event. EMSystem is compatible with Health andHuman Services (HHS) Region VI enabling the federal government to oversee activitieson the state level.Communication SystemsThe State identified communication systems for redundancy:o Primary system- Internet emailo Secondary system – Telephone and faxo Tertiary system– Two-way radiosAll Tier 1 hospitals have at least one emergency two-way radio. A regional decision wasas to the selection of a two way radio.o Hospitals in Regions 2,3,4,5, and 9 – HEAR radioo Hospitals in Regions 1, 6,7,8 - 800 MHz radioThe Louisiana Department of Health and Hospitals Office of Emergency Preparedness,Designated Regional Coordinators and Designated Regional Hospitals are equippedwith 800 MHz radios for statewide communications.Ongoing DrillsState-wide Radio Check: Every Monday at 0830 hours, a statewide radio check iscompleted. The radio checks are conducted with a rotating responsibility between theDesignated Regional Coordinators at the state level.Regional Radio Checks: A radio check is conducted on a weekly basis among hospitalsin Region 7 (Shreveport area), Region 6 (Alexandria area) and Region 1 (New Orleans).Region 8 hospitals (Monroe area) conduct a radio check daily. Region 2 (Baton Rouge)hospitals conduct a radio check every month. The radio checks are conducted withrotating responsibility of coordinators within each region. By the fall of 2006, each of the9 regions will be conducting similar radio checks.Communication remains a challenge even with the best of plans. During HurricaneKatrina most communications in Region 1 and all communications were lost in Region 9due to many, many technical difficulties.Plans are underway to improve redundancy statewide.ii. Patient Movement ProcessWORKING DRAFT 8/17/076
The hospital plans for evacuation are developed as worse case” scenario conditions.The litigious environment, the Homeland Security hearings’ criticisms, the weakenedlevees, fragile infrastructure, the weakened response capabilities, and overburdenedstaff add to the indirect factors that may facilitate hospital evacuations regardless ofstructural ability to shelter-in-place.From a strategic perspective, Louisiana continues to support the strategy that patientsshould not be moved on a “maybe” event (prior to a storm) as it is not in the bestinterest of the patient to move critical care patients. Our federal partners support thestrategy of sheltering-in-place (SIP) provided it can be done so safely. Hospitals mustevaluate hardening structures and increasing supply assets so that unnecessarymovement of critical patients is minimized.In the event patient movement is required, the Louisiana Hospital EmergencyPreparedness and Response has facilitated the development of regional and statewidepatient movement processes.The patient movement process is implemented only when the state has declared a stateof emergency or as requested by the Louisiana Department of Health and HumanServices. The HRSA Hospital Emergency Preparedness and Response systemprovides the backbone of the regional and statewide patient movement processes.There are three components to the patient movement: resource availability, patienttransfer process (In-State and Out-of-State) and patient tracking.Resource AvailabilityWith respect to resource availability, the Designated Regional Coordinator (DRC) fromeach region serves to support the process by identifying available resources in his/herregion. Briefly, hospitals are asked to contact and work through the DesignatedRegional Coordinators to identify and/or request hospital-based resources available inregions throughout the state. DRCs “match” patient care needs with availableresources in the state and facilitate the arrangement of a hospital-to-hospital transfer.Hospitals report resources available on an as needed base, to Designated RegionalCoordinators through a resource tracking tool, EMSystems.EMSystem allowsLouisiana to maximize existing resources.Patient TransferIn- State Movement of PatientsPatient transfer includes the movement of patients from one region to another during adeclared state of emergency. Hospitals are encouraged to exhaust all local resourcesbefore requesting support through the statewide patient transfer process. TheAdministrator/Medical Director on call from the hospital that has patients that need to betransferred outside the region should contact their Designated Regional Coordinator.(See Appendix B for contact information for the HRSA DRCs. The transferring hospitalWORKING DRAFT 8/17/077
should have the specific information available regarding patient needs for their DRC.The “transferring” DRC will contact an “accepting” DRC with a referral request. The“accepting” DRC will contact hospitals in their region to identify available resources. Ifresources are not available, the accepting DRC will contact the HRSA Coordinator toadvise that another alternative region must be identified. An “accepting” hospital willcontact the transferring hospital regarding transfer resources. Transfer will be arrangedper procedures of the transferring and receiving hospitals.A copy of the Emergency Patient Transfer Process is included in Appendix E.Out-of-State Movement of PatientsIn the event institutional plans fail, state and federal assets will be required to assist withthe evacuation of medical institutions. Given the limited resources at the local and statelevels, federal support will be required to support a medical institution evacuation plan.Planning Assumptions: All hospitals are primarily responsible for their own disaster evacuation plans. Itis anticipated that hospitals will remain in control of all aspects of their facilityevacuation plans, and will use pre-identified resources for execution of their plan. It is also anticipated that unknown and uncontrollable variables may interruptand/or limit the facility’s ability to execute evacuation plans and that they mayrequest assistance. This plan identifies the timelines, decisions, and assets thatstate and federal coordinated assets bring to bear when this plan is executed.Specific plans for the medical evacuation of patients in Regions 1, 3, 4, 5 and 9 havebeen established and are available in Appendix J Medical Institutional EvacuationPlans.Patient TrackingAn interim patient tracking system has been established by the Louisiana HospitalAssociation (LHA) to facilitate the identification of patients moved during a declaredstate of emergency. LHA has established a website for data collection and a secondsite for patient query. The State of Louisiana will establish a more comprehensivepatient tracking system in the future. Hospitals may contact the Louisiana HospitalAssociation via email at evacuateme@yahoo.com.The LHA will store the patienttracking data in central repository accessible via the web at www.lhaonline.org.A copy of the LHA Patient Tracking System is included in Appendix G.iii. Medical Queue for Mass EvacuationConsistent with the State’s plan to support mass evacuation, Designated RegionalCoordinators assist in establishing a “medical queue” in cooperation with the regionalunified command staff.WORKING DRAFT 8/17/078
To facilitate evacuation, the Louisiana Department of Health and Hospitals and supportagencies have identified a system of triggers and actions to assist. Triggers andsupporting responses have been established based on “H-Hour” timeframes establishedby the Governor’s Office of Homeland Security and Emergency Preparedness. H-Hourhas been defined as H-Hour 0 24 hours prior to tropical storm force winds makinglandfallSee Appendix H for the Louisiana Hospital Emergency Preparedness andResponse: H - Hour ResponseAs hospitals request assistance to evacuate particular units or entire buildings, theregional unified command will work to identify the medical queue. This will list whichhospitals evacuate in order of priority. Evaluations will include weather conditions,flooding, structural condition of the facility, condition of patients, etc, and will becommunicated to those assisting with the transportation assets (DODT).TheDesignated Regional Coordinator is responsible for assuring that the process iscompleted and communicated to the ESF 8 incident command structure and impactedhospitals.iv. Emergency Code UniformityEmergency Code uniformity enables many individuals at multiple facilities to respondconsistently to emergencies, which ultimately enhances safety for patients, visitors, andstaff. Reasons for seeking uniformity include: With the current nursing and other healthcare professional’s shortage, manyorganizations share personnel. Having a consistent code system reduces theamount of information an employee must learn or re-lean and lessens theopportunity for confusion during emergent or disaster events. Communication among hospitals and other agencies in a specific geographicregion during an emergency can be enhanced when there is a commonlanguage (for instance, DASH, DASH II, MMRS, and other statewideagreements that involve different regions). Communication during statewide, regional, or local weapons of massdestruction (WMD) events will also be enhanced. The myriad of different systems using numbers, alpha codes, and color codescreates confusion, increases the likelihood of miscommunication, and potentialfor serious outcome to patient care.Code Recommendations:The following code designations for emergency identification in healthcare organizationsare recommended:WORKING DRAFT 8/17/079
CODE BLUECODE RED-Medical Emergency – Cardiac/Respiratory ArrestFireCODE GREYCODE BLACKCODE PINKCODE YELLOWCODE ORANGECODE WHITE-Severe WeatherBombInfant/Child AbductionDisaster – Mass CasualtyHazardous MaterialsSecurity Alert – Violence/HostageNote that while the above main colors remain constant, there is flexibility built into thesystem for individual hospital needs. Emergency code colors not stated may be usedby individual organizations to address specific facility or geographic concerns. The goalis to have a common set of base colors and for hospitals to customize them to meettheir needs albeit a response to these events is very similar hospital to hospital.v. Special Needs ShelteringThere is a growing vulnerable population in Louisiana. The vulnerable population isdefined as being medically dependent or those individuals with ongoing medical needsthat require support, but not hospitalization.Louisiana provides three types of shelters: General shelters, special needs sheltersand hospital-based shelters. These shelters provide a triage network of shelter care forvulnerable patients. Depending upon the acuity of the shelteree, potential sheltereescan be triaged to a general shelter; special needs shelter, or hospital shelter.Many hospitals in Louisiana signed a Memorandum of Understanding (MOU) in 2004 toprovide assistance for the state supported Special Needs Sheltering network. Hospitalsmay choose to provide:o direct sheltering or send personnel and supplies to state or local shelters.o operation of an In-Hospital Special Needs or General Shelter.o provide medical care to patients referred from a shelter (shelter referred) or selfreferred (walk-in) patients.It is important to note, that while hospitals signed the MOU to assist with sheltering,hospitals are not required to provide sheltering. Rather, given an incident each hospitalshould identify the best use of its existing resources be it inpatient acute services or forsheltering.WORKING DRAFT 8/17/0710
A process to reimburse hospitals for sheltering expenses has been developed by theDepartment of Health and Hospitals and the Federal Emergency Management Agency(FEMA).The Louisiana Hospital Association has agreed to assist hospitals insubmission of the appropriate documentation. Specific information related to FEMAreimbursement for sheltering expenses can be found at the Louisiana HospitalAssociation website: www.lhaonline.org.III. Maintenance of Individual Hospital’s Disaster ProgramThis document addresses the relationships between and among hospitals and isintended to augment, not replace, each facility's disaster plan. This document does notreplace but rather supplements the rules and procedures governing interaction withother organizations during a disaster (e.g., law enforcement agencies, the localemergency medical services, local public health department, fire departments,American Red Cross, etc).A checklist for the Hospital CEO has been identified and is attached as Appendix I.WORKING DRAFT 8/17/0711
WORKING DRAFT 8/17/0712
WORKING DRAFT 8/17/0713
Appendix ALouisiana Hospital Emergency Preparedness and ResponsePlanning RegionsWORKING DRAFT 8/17/0714
Appendix BDesignated Regional CoordinatorsFY 06-07DESIGNATED REGIONAL COORDINATORSREGION1COORDINATORNorris YarbroughFACILITYOFFICEOchsner Foundation HospitalE-MAILnyarbrough@ochsner.org1Cynthia MatherneMetropolitan Hospital Council504-842-3772504-837-11711Frank FolinoTouro Infirmary504-897-7990folinof@touro.com2Allyn Whaley-MartinOur Lady of the Lake RMC225-765-8329awhaley@ololrmc.com2Ruth TurmanEarl K. Long225-358-1320rturma@lsuhsc.edu2Connie DeLeoBaton Rouge e EdelenEarl K. Long225-358-1108wedele@lsuhsc.edu3Percy MoselyTerrebonne General Med Ctr985-873-4271percy.mosely@tgmc.com4Anjanette HebertLafayette General Med Ctr337-289-7441ahebert@lgmc.comLiz HarmonHRSA Region 4 & 5337-570-4230lizharmonadrc@bellsouth.net5Mark SevernsLake Charles Memorial Hosp.337-436-6111mseverns@lcmh.com5Lee WillefordCHRISTUS St. Patrick of 5WORKING DRAFT 8/17/0715micdav22@yahoo.com
REGIONCOORDINATORFACILITYOFFICEE-MAIL6Mary TarverCHRISTUS St. Frances Knox AndressLSUHSC-Shreveport318- 813-3311wandr1@lsuhsc.edu8Mike BrameSt. Francis Medical Center318-327-4971bramem@stfran.com8Sheila MasonFranklin Medical Center318-435-9411smason@fmc-cares.com9Keith PeekSlidell Memorial Hospital985-649-85289Karen MoiseSt Tammany Parish Hospital985-898-4087peekk@smhplus.org;keith peek@yahoo.comkmoise@stph.orgDHHRosanne HAAsha GreenLHA225-928-0026agreen@lhaonline.orgLHAMarcia FriesLHA225-928-0026mfries@lhaonline.orgLHATatsy JeterLHA225-928-0026pjeter@lhaonline.orgLHAKendra ta ORKING DRAFT 8/17/0716
Appendix CHospitals by Type and Region(Updated TYBehavioral Hospital ofKenner (Located insideKenner Regional)Children's HospitalTYPELICBEDSHOSPITALCOORDINATORPsychT-2Gary ChaneyAcutew/ERT-1Lisa MirandaCommunity CareHospitalPsychT-2Paul B. KavanaughJeffersonEast Jefferson GeneralHospitalDRHT-1Linda Daigle1OrleansHealthwestRehabilitation HospitalRehabT-2Paul McCannRachel Kancewick1OrleansKindred Hospital - NewOrleansLTACT-2David Boyd1JeffersonT-2Stephanie T. Wells,CPA1OrleansLouisiana SpecialityLTACHospital (formerlySolara Hospital)LSU-Medical Center of LouisianaDRH1OrleansMedical Center of Louisiana-UniversityCathi Fontenot,Laurie Smith, BobSigilitoLaurie Smith1OrleansNew Orleans Adolescent Hospital1OrleansOchsner Baptist Medical CenterWORKING DRAFT 8/17/07T-2Shelby PriceEric YancovichWayne Hill17TITLEHRSA Emer PrepCoord/AdministratorHRSA Emer PrepCoord/PlantOper/SafetyHRSA Emer PrepCoord/President/CEOHRSADRC/DRHRep/Asst AdminHRSA Emer PrepCoord/CEOHRSA Emer PrepCoord/Director ofTherapyHRSA Emer PrepCoord/Dir QualityMgmtHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA EmerPrep CoordHRSA Emer PrepCoorHRSA Emer PrepCoord/AdministratorHRSA Emer igle@ejhospital.com504-433-5551hrhceo@i-55.com; hrhrehab@i-55.com504-894-7649david ahc.com504-903-0283lsmith1@lsuhsc.edu; 7-5998eyancovich@ochsner.org;whill@ochsner.org
Executive Officer1OrleansOchsner MedicalCenterDRHDRHNorris YarbroughMelissa Mitchell1JeffersonOchsner MedicalCenter-KennerAcutew/ERT-1Eric YancovichRobin Wallace1JeffersonOchsner MedicalCenter-West BankAcutew/ERT-1Eric YancovichFrank Urbeso1JeffersonOmega HospitalAcute/LTDT-210Debbie Schenck1OrleansPsychT-224Daniel Aguillard1JeffersonEvelyn NottingJeffersonPsych(FWF)PsychT-21Psychiatric PavilionNew Orleans LLCRiver Oaks Child andAdolescent HospitalRiver Oaks HospitalT-2Evelyn Notting1JeffersonSelect SpecialtyHospitalLTACT-2Robert Baker1OrleansSpecialty Hospital of New Orleans(reopened 9/18/06)T-2Irving Sawyers, Jr.1OrleansSt. John's RehabilationHospitalRehab(FWF)T-2Robert S. Rotolo1OrleansTouro InfirmaryT-1Frank Folino1OrleansT-2Frank Folino1OrleansTouro RehabilitationCenterTulane UniversityHospital and ClinicAcutew/ERRehab(FWF)Acutew/ERT-1Natasha WellsWORKING DRAFT 8/17/0718HRSADRC/DRH RepHRSA EmerPrep CoordHRSA Emer PrepCoord/Director ofFacilitiesHRSA Emer PrepCoord/Mgr ofPlant OperationsHRSA Emer PrepCoord/Director dnessHRSA Emer PrepCoor/CEOHRSA Emer PrepCoordHRSA Emer PrepCoordHRSA Emer PrepCoord/SafetyOfficerHRSA Emer PrepCoord/CEOHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA Emer PrepCoordHRSA Emer PrepCoordHRSA Emer ony@hcahealthcare.comrsrotolo@aol.com
1JeffersonTulane-LakesideHospitalWest JeffersonMedical CenterAcuteT-2Anita Lindsey1JeffersonDRHDRHMitch Leckelt2EBRBaton Rouge GeneralMedical Center BluebonnetAcutew/ERT-1105Connie Deleo2EBRBaton Rouge GeneralMedical Center - MidCityDRHDRH343Cindy Munn2EBRBehavioral Hospital ofBaton RougePsychT-224Angie Maxwell2EBRBenton RehabilitationHospitalRehabT-213Amanda Pace2EBRRehabT-2142EBRBethesda RehabililtationHospitalCypress PsychiatricHospitalPsych(FWF)T-230Dr. TheresaSpeightKenneth O'Rourke2EastFelicianaEastFelicianaEastern LouisianaMental Health SystemFeliciana ForensicFacilityPsychT-2337Sylvia BrinsonPsychT-2235Teresa J. Palmer2EBRGreater Baton RougeSurgical HospitalAcuteT-210Bradley Devillier2EastFelicianaGulf States LTAC ofFelicianaLTACT-216Wayne Dodge2EBRHealthsouthRehabilitation Hospitalof Baton RougeRehabT-280Murry R. Harmon2WORKING DRAFT 8/17/0719HRSA Emer PrepCoordHRSADRC/DRHRep/Asst AdminHRSADRC/InfectionControlCoordinatorHRSA Emer PrepCoordHRSA Emer PrepCoord/AdministratorHRSA Emer PrepCoordAdministrator/ComplianceOfficerHRSA Emer PrepCoordHRSA Emer PrepCoord/AdministratorHRSA Emer PrepCoord/SafetyHRSA Emer PrepCoord/SafetyCoordHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA Emer PrepCoord/AdministratorHRSA Emer th.comjrodriguez@powerhousemgt.com
2EBRLane Memorial HospitalAcutew/ERT-1137Michelle Stevens2EBRDRHWayne Edelen, Jr.EBRDRHT-21612LSU-Earl K. LongMedical CenterOceans BehavioralHospital of Baton Rouge18Debbie Tullier2EBROchsner MedicalCenter-Baton RougeT-1201Steven Miller2EBRPointeCoupeeAcutew/ERDRHT-17192Our Lady of the LakeRMCPointe Coupee GeneralHospital25Allyn WhaleyMartin, CPHRMChad Olinde2AscensionPrevost censionPromise Hospital@AscensionT-254Steve McQueen,RPh, CCS2EBR2EBR2Iberville2EBRAcutew/ERDRHLTACPromise SpecialtyHospital of BR @ BRGeneralPromise SpecialtyHospital of BR @OschnerRiver West MedicalCenterLTAC(FWF)T-228M. Bryan DayLTAC(FWF)T-229M. Bryan DayAcutew/ERT-180R.L. DownsSAGE RehabilitationInstituteRehabT-242Jason RisleyWORKING DRAFT 8/17/0720HRSA Emer PrepCoord/ERDirectorHRSADRC/DRH RepHRSA EmerPrepCoord/AdministratorHRSA Emer PrepCoord/PlantOperationsDirectorHRSADRC/DRH RepHRSA Emer PrepCoord/DirImaging/SafetyHRSA Emer PrepCoordHRSA Emer PrepCoord/AdministratorHRSA Emer PrepCoord/Administrator ClinicalSupport ServicesHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA Emer PrepCoord/ChiefExecutive OfficerHRSA Emer PrepCoord/ChiefExecutive 8-1108wedele@lsuhsc.edu
The Louisiana Department of Health and Hospitals, Office of Emergency Preparedness provides coordination on behalf of the State of Louisiana and all other state agencies, to the federal government through Emergency Support Function (ESF) 8 - Health and Medical Services, and the Louisiana Hospital Emergency Preparedness and Response.