Transcription
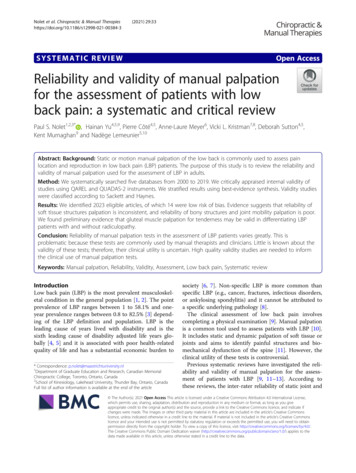
Nolet et al. Chiropractic & Manual 3(2021) 29:33SYSTEMATIC REVIEWOpen AccessReliability and validity of manual palpationfor the assessment of patients with lowback pain: a systematic and critical reviewPaul S. Nolet1,2,3* , Hainan Yu4,5,9, Pierre Côté4,5, Anne-Laure Meyer6, Vicki L. Kristman7,8, Deborah Sutton4,5,Kent Murnaghan9 and Nadège Lemeunier5,10Abstract: Background: Static or motion manual palpation of the low back is commonly used to assess painlocation and reproduction in low back pain (LBP) patients. The purpose of this study is to review the reliability andvalidity of manual palpation used for the assessment of LBP in adults.Method: We systematically searched five databases from 2000 to 2019. We critically appraised internal validity ofstudies using QAREL and QUADAS-2 instruments. We stratified results using best-evidence synthesis. Validity studieswere classified according to Sackett and Haynes.Results: We identified 2023 eligible articles, of which 14 were low risk of bias. Evidence suggests that reliability ofsoft tissue structures palpation is inconsistent, and reliability of bony structures and joint mobility palpation is poor.We found preliminary evidence that gluteal muscle palpation for tenderness may be valid in differentiating LBPpatients with and without radiculopathy.Conclusion: Reliability of manual palpation tests in the assessment of LBP patients varies greatly. This isproblematic because these tests are commonly used by manual therapists and clinicians. Little is known about thevalidity of these tests; therefore, their clinical utility is uncertain. High quality validity studies are needed to informthe clinical use of manual palpation tests.Keywords: Manual palpation, Reliability, Validity, Assessment, Low back pain, Systematic reviewIntroductionLow back pain (LBP) is the most prevalent musculoskeletal condition in the general population [1, 2]. The pointprevalence of LBP ranges between 1 to 58.1% and oneyear prevalence ranges between 0.8 to 82.5% [3] depending of the LBP definition and population. LBP is theleading cause of years lived with disability and is thesixth leading cause of disability adjusted life years globally [4, 5] and it is associated with poor health-relatedquality of life and has a substantial economic burden to* Correspondence: p.nolet@maastrichtuniversity.nl1Department of Graduate Education and Research, Canadian MemorialChiropractic College, Toronto, Ontario, Canada2School of Kinesiology, Lakehead University, Thunder Bay, Ontario, CanadaFull list of author information is available at the end of the articlesociety [6, 7]. Non-specific LBP is more common thanspecific LBP (e.g., cancer, fractures, infectious disorders,or ankylosing spondylitis) and it cannot be attributed toa specific underlying pathology [8].The clinical assessment of low back pain involvescompleting a physical examination [9]. Manual palpationis a common tool used to assess patients with LBP [10].It includes static and dynamic palpation of soft tissue orjoints and aims to identify painful structures and biomechanical dysfunction of the spine [11]. However, theclinical utility of these tests is controversial.Previous systematic reviews have investigated the reliability and validity of manual palpation for the assessment of patients with LBP [9, 11–13]. According tothese reviews, the inter-rater reliability of static joint and The Author(s). 2021 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License,which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you giveappropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate ifchanges were made. The images or other third party material in this article are included in the article's Creative Commonslicence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commonslicence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtainpermission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.The Creative Commons Public Domain Dedication waiver ) applies to thedata made available in this article, unless otherwise stated in a credit line to the data.
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33soft-tissue palpation to locate pain is poor (kappa (k) 0.40), and the inter-rater reliability of static palpation forsoft tissue changes (e.g., tension) is inconsistent [9, 11,13]. Furthermore, one review reported that motion palpation may be valid in detecting decreased motion, orlack of end-play in the lumbar spine [12]. However, motion palpation may not be valid to detect aberrant motion of the sacroiliac joints [12]. These reviews areoutdated and there is a need for an up-to-date systematic review. The purpose of our systematic review was todetermine the reliability and validity of manual palpationused to assess adult patients with LBP.MethodsEligibility criteriaPopulationWe included studies of adults ( 18 years) with LBP. LBPrefers to pain or discomfort below the costal margin andabove the inferior gluteal folds and can be with or without referred leg pain [14]. Our systematic review includes patients with non-radicular low back pain,radicular low back pain, spinal stenosis, degenerative oristhmic spondylolisthesis, and failed back surgerysyndrome.DefinitionsOur review focuses on studies assessing the reliability orvalidity of manual palpation for the assessment of patients with LBP. Reliability describes the consistency ofmeasurements across people or instruments [15]. Validity is the degree to which a test measures what it isintended to measure [15].Manual palpation is a diagnostic procedure where theexaminer feels with their hands to assess the mobilityand state of the soft and boney tissues [16]. Palpationtechniques include both static and dynamic (motion)methods, which are often used to identify areas of tissuepain and dysfunction, target manual and manipulativetherapies and determine effectiveness of the intervention[9]. Static palpation is used to identify bony asymmetryof bony landmarks, tender points, and trigger points toevaluate tissue texture, temperature and tone [17]. Motion palpation is used to assess the quantity and qualityof movement through the lumbar spine and pelvis [17].Motion palpation assessment can be continuous withinthe normal range of motion with joint play, or dynamicsoft tissue palpation or end range assessment for endfeel or joint springing [17]. Palpation involving devicessuch as pressure algometry were excluded.OutcomesWe aimed to evaluate clinical outcomes assessed by palpation. Outcomes include pain, segmental mobility andstiffness for static joint palpation; joint movement andPage 2 of 20position assessed for motion joint palpation; and pain,tenderness, trigger points, muscle contraction assessedfor static soft tissue palpation.Study characteristicsEligible studies met the following inclusion: 1) Englishor French language; 2) published in peer reviewed journals between January 1, 2000 to July 11, 2019; 3) assessing the reliability or validity of manual palpation.Previously published systematic reviews on this topicwere included in our review. Comparing our systematicreview with previous systematic reviews examined findings of studies published before 2000. We excluded: 1)letters, guidelines, editorials, commentaries, unpublishedmanuscripts, dissertations, reports, book chapters, conference proceedings and abstracts, lectures, addresses,and consensus statements; 2) cadaveric and animal studies; 3) literature reviews and case studies; 4) studies targeting individuals with serious pathology (e.g., fractures,dislocations, systemic disease, myelopathy, neoplasm andinfection; and 5) studies with sample size 20 per group.Search strategy and data sourcesThe search strategy was developed in consultation witha health sciences librarian and a second librarian wasconsulted to ensure accuracy and completeness usingthe Peer Review of Electronic Search Strategies PRESSchecklist [18]. We systematically searched the followingelectronic databases: MEDLINE, CINAHL, PubMed,Cochrane Central Register of Controlled Trials, andSPORTDiscus. Search terms consisted of subject headings specific to each database (e.g. MeSH in MEDLINE)and free text words relevant to LBP, diagnosis, reliability,validity, and palpation (Additional file 1).Study selectionIdentified citations were exported into EndNote for reference management and tracking of the screeningprocess. We screened articles in two stages. In stage one,titles and abstracts were screened for their relevance bypairs of independent reviewers (NL, PN, ALM). Stagetwo involved screening the full text article of all possiblyrelevant citations from stage one. Disagreements onscreening stages were discussed between reviewers toreach consensus. When consensus could not be reached,a third reviewer independently screened the citation anddiscussed with the two reviewers to reach consensus.Assessment of risk of BiasThree reviewers (NL, PN, ALM) critically appraised allrelevant studies (Tables 1 and 2) using the modifiedQuality Appraisal Tool for Studies of Diagnostic Reliability (QAREL) [33] criteria to assess the internal validity of the diagnostic reliability studies and the modified
YYYYYYYYYYYDowneyet al., 2003[21]Hebertet al., 2015[22]Hicks et al.2003 [23]Jensenet al.2013 [24]Ravennaet al., 2011[25]Schneideret al., 2008[26]Tong et al., Y2006 [27]YArab et al.,2009 [20]Walshet al., 2009[28]Weineret al., 2006[29]YYYYYYYYYYYRepresentativeratersN No, N/A Not applicable, ref. std. reference standard, UC Unclear, Y YesYYYYYYYYYAlyazediet al. escribedAuthor,YearYYYYYYYYYYYBlinded YN/AN/AN/AN/AN/AYN/AN/AN/ABlinded to Blinded toownresults offindingsref stdYNNYNUCUCUCUCYYBlinded toclinicalinformationTable 1 Risk of bias for scientifically admissible reliability studies based on the modified QAREL criteriaUCUCUCYUCUCUCUCUCYYBlinded toadditionalcluesUCNUCYYYUCYYYUCOrder ofexamvariedYYUCYYYYYYYYYYYYYYYYYYYAppropriate Testtime interval easuresNolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 3 of 20
NNNYNHebert et al.,2015 [22]Koppenhaveret al., 2013[31]Soleimanifaret al., 2017[32]Walsh et al.,2009 [28]Weiner et al.,2006 [29]YYYYYN/AYNYYYBlinded toref stdresultsN No, N/A Not applicable, ref. std. reference standard, UC Unclear, Y YesNYYYYYYAdelmaneshet al., 2016[30]YCase-control AvoideddesigninappropriateavoidedexclusionsAuthor, Year holdN/AYYYYYDescribedref stdN/AUCYYYYAppropriateref stdTable 2 Risk of bias for scientifically admissible validity studies based on the modified QUADAS-2 criteriaN/AYNYYYBlinded toindex testresultsN/AUCYUCYYN/AYYYYYN/AYYYYYAppropriate All patients All patientstime interval received ref received samestdref stdUCYYYUCYAll patientsincluded inanalysisNolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 4 of 20
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33Quality Assessment of Diagnostic Accuracy Studies-2(QUADAS-2) [34] criteria to assess diagnostic accuracy/validity studies (Additional files 2 and 3). The originalQAREL and QUADAS-2 instruments were modified toinclude: 1) not applicable options; 2) a question regarding the clarity of the study objective; and 3) the Sackettand Haynes classification (phases of validity studies inQUADAS-2 instrument). If a study was judged as “low”on all domains relating to bias or applicability then itwas appropriate to have an overall judgment of “low riskof bias” or “low concern regarding applicability” for thatstudy. If a study was judged “high” or “unclear” on oneor more domains then it may be judged “at risk of bias”or as having “concerns regarding applicability” [33, 34].We included low risk of bias studies in our best evidencesynthesis.Validity studies with low risk of bias were classifiedinto one for four phases of investigation following therecommendation of Sackett and Haynes [35]. The purpose of phase I studies is to determine if test results aredifferent for LBP patients and healthy controls. The purpose of Phase I studies is to determine whether test results differ between LBP patients and healthy controls.This information is useful to justify Phase II studies.Phase II studies aim to determine whether patients witha positive palpation result are more likely to have decreased functions, severe disability or structure changes(e.g., spinal stenosis) than patients with a negative result.Phase I and II studies provide preliminary evidence thata test should to be tested in phase III studies. On theirown, results from phase I and II studies cannot be usedto confirm the validity of tests. However, according toSackett and Haynes classification, phase I – II justify thata test should be further investigated. Phase III studiesaim to determine whether a test result can distinguishbetween LBP patients with suspected conditions (e.g.,radiculopathy). Finally, Phase IV studies aim to determine whether patients who undergo a manual palpationtest have a better prognosis than similar patients whowere not tested [35]. Phase IV studies are a unique typeof studies that differ from phase I-III studies in examining diagnostic accuracy. Low risk of bias of phase IVstudy would be assessed using the Scottish Intercollegiate Guidelines Network (SIGN) criteria [36].Data extraction and synthesis of resultsOne reviewer (PN) extracted data from low risk of biasstudies and built evidence tables (Tables 3 and 4); andtwo reviewers (NL or HY) verified the accuracy andcompleteness of the data extraction. The reliability andvalidity studies were stratified according to targeted bodystructures (joint or soft tissue), technique (static or motion palpation), and clinical outcome (pain provocation,mobility, or stiffness). We used qualitative synthesis toPage 5 of 20synthesize the best evidence [37]. Eligible statistics include 1) means, median and/or percent in phase I studies; 2) correlations, sensitivity, specificity, positivepredictive value, negative predictive value and/or likelihood ratio in phase II or III studies; and 3) prevalence inphase III studies.No arbitrary classification was used to report thestrength of reliability or validity findings. Such classification used arbitrary cut-points that do not take intoaccount the level of misclassification that can be acceptable in specific context. Rather, values of kappa coefficients, sensitivity, specificity etc. were reported. Theauthors interpreted the kappa and measurement errorsaccording to clinical settings and purposes of palpationtests in their context. Kappa scores of 0.6 are considered to have no, minimal or weak agreement and kappascores of 0.6 are considered to have moderate, strongor almost perfect agreement [38]. This should be used asa rough guide when interpreting the kappa and measurement errors according to clinical settings and purposesof palpation tests in individual context.Statistical analysesWe computed kappa coefficients (k) and 95% confidenceintervals (CI) to determine the inter-rater reliability ofour screening methodology of articles. We computedthe percentage agreement between reviewers for theclassification of articles into high or low risk of bias.ReportingThis review complies with the Reporting Items forSystematic Reviews and Meta-Analyses (PRISMA) statement (Additional file 4) [39]. The Statement for Reporting Studies of Diagnostic Accuracy (STARD) was usedto inform in the critical appraisal with the QAREL andQUADAS-2 [40].ResultsStudy selectionWe identified 2307 citations (plus 3 citations from otherresources) removed 287 duplicates, and reviewed 2023articles for eligibility (Fig. 1). In stage 1 screening, 1976citations were ineligible. Forty-seven papers werereviewed in stage 2, and 31 were excluded: ineligiblestudy population (n 11) [41–51], inappropriate outcome measure (n 6) [52–57], ineligible publicationtype (n 4) [58–61], ineligible sample size (n 3) [62–64], study design (n 3) [65–67] and did not investigatemanual palpation (n 4) [68–71]. Two authors werecontacted for publication type and age range, bothresponded [27, 59].We critically appraised 16 articles and 14 articles hadlow risk of bias and were included in our evidence synthesis [19–32] (Fig. 1). Over the 16 articles appraised, 14
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 6 of 20Table 3 Evidence table for low risk of bias studies assessing the reliability of manual palpation tests in patients with low back painAuthors,YearCountryDesignSample Size(n)Case DefinitionIndex TestReliabilityStatic Joint Palpation (n 262)Alyazediet al.2015[19]USAInter-raterreliability(n 40)Recurrent LBP or chronic LBP ( 3months), 21–71 yrs. old.Prone instability test was done in two parts: 1)relaxation phase: the subject was lying prone onthe examination table with feet on the floor. Theexaminer performed PA mobility testing to identifypainful lumbar segments with the subject’s musclesrelaxed. 2) co-contraction phase: the subjects thenraises their feet off the floor. If pain identified in therelaxation phase subsides at the co-contractionphase the test is considered positive.PA glide test: Subjects were lying prone andexaminers performs PA glide on the lumbar spinousprocesses. Lack of segmental hypomobility, isconsidered a positive test.Examiners: two physical therapists who werecertified as Orthopaedic Clinical SpecialistsTime between inter-rater assessments was at least15 minInter-rater reliabilityProne instability test forpain (relaxation phase);k (95% CI)k 0.41 (0.18, 0.63)Prone instability test forpain (co-contractionphase);k (95% CI)k 0.71 (0.45, 0.98)PA glide test forhypomobility; k (95% CI)k 0.02 ( 0.22, 0.18)Downeyet al.,2003[21]AustraliaInter-raterreliability(n 60)[n 20/pair]Non-specific LBP 7 weeks duration, 18 yrs. old.Palpation for the spinal level contributing most tothe patients’ LBP symptoms (abnormal end-feel, abnormal quality of resistance to motion, andreproduction of pain, local or referred); patientprone, posterior to anterior pressure applied tospinal process and verbal communication betweenexaminer and patient about reproduction of pain.Examiners: three pairs of manipulativephysiotherapists with 7–15 yrs. experience and 3yrs. experience after postgraduate qualifications inmanipulative physiotherapy.Time between inter-rater assessments unknown.Inter-rater reliabilityPalpation to locate thespinal level; k (95% CI):Overall: k 0.37 (0.20,0.54)Pair 1: k 0.54 (0.26, 0.82)Pair 2: k 0.45 (0.18, 0.72)Pair 3: k 0.23 (0.00, 0.46)Palpation to name thespinal level; k (95% CIlower band):Overall: k 0.09 (0.00,0.18)Pair 1: k 0.41 (0.12, 0.70)Pair 2: k 0.10 (0.00, 0.20)Pair 3: k 0.13 (0.00,0.26)Hickset al.,2003[23]USAInter-raterreliability(n 63)[pair 1 n 20,pair 2 n 28,pair 3 n 15]Low back pain without radiation ofpain past the knee, symptomduration unknown, 20 to 66 yrs. old.Prone instability test: The subject lies prone on theexamination table with their feet on the floor. Theexaminer performs passive intervertebral motiontesting for pain. The subject then lifts their feet offthe floor. A positive test is when pain provokedduring the first part of the test disappears when thelegs are lifted up.Passive intervertebral motion testing: with thesubject lying prone the examiner applied PApressure with their hypothenar eminence on eachlumbar spinous process. Segmental mobility isjudged as normal mobility, hypomobility (moremotion than normally expected) and hypermobility(less motion than normally expected). Painprovocation is judged as manual pressureproducing pain or not producing pain.Examiners were 4 physical therapists with a least 2yrs. experience. Examiners were placed in 3 separatepairs.Time between inter-rater assessments was at least15 minInter-rater reliabilityProne instability test; k(95% CI):k 0.87 (0.80, 0.94)Pair 1 (n 20): k 1.0(1.0–1.0)Pair 2 (n 28): k 0.81(0.80–0.94)Passive intervertebralmotion tests; k (95% CI):Segmental mobility(dichotomous):Hypermobility k 0.30(0.13, 0.47)Hypomobility k 0.18(0.05–0.32)Segmental mobility(hypo/normal/hyper):L1 k 0.26 ( 0.01, 0.53)L2 k 0.17 ( 0.13, 0.47)L3 k 0.02 ( 0.25, 0.28)L4 k 0.11 ( 0.26, 0.35)L5 k 0.18 ( 0.03, 0.49)Pain provocation(positive/negative):L1 k 0.36 (0.12, 0.59)L2 k 0.45 (0.26, 0.63)L3 k 0.30 (0.12, 0.47)L4 k 0.25 (0.11, 0.40)L5 k 0.55 (0.43, 0.67)
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 7 of 20Table 3 Evidence table for low risk of bias studies assessing the reliability of manual palpation tests in patients with low back pain(Continued)Authors,YearCountryDesignSample Size(n)Case DefinitionIndex TestReliabilityRavennaet al., 2011[25]USAInter-raterreliability(n 30)Chronic and recurrent LBP, 18 to 60yrs. Old.Prone Instability Test: patient prone with legs overthe edge and feet resting comfortably on the floor.The examiner palpates for pain. The patient thenraises their legs off the floor and examiner palpatesagain for pain. A positive test is when painprovoked during the first part of the test disappearsor decrease when the legs are lifted up.Examiners were a second-year Doctor of PhysicalTherapy student and a licensed physical therapistwith two years clinical experience.Time between inter-rater assessments was 20 min.Prone Instability Test; k(95% CI), PABAK (95%CI)0.10 ( 0.27, 0.47), 0.27 ( 0.08, 0.61)Schneideret al., 2008[26]USAInter-raterreliability (n 39)Low back pain, symptom durationunknown, 18–65 yrs. old.Palpation for lumbar segmental mobility, painprovocation and prone instability: patient pronewith 1) Prone mobility testing: posterior to anteriorjoint springing palpation by examiners of SIJs, alllumbar spinous processes and all lumbar facet jointsbilaterally; normal or restricted mobility was noted;2) prone pain provocation testing: patient notifiespain or discomfort provoked while repeating pronemobility test; 3) prone instability test: patient pronewith legs over the edge and feet restingcomfortably on the floor. The examiner palpates forpain. The patient then raises their legs off the floorand examiner palpates again for pain. A positivetest is when pain provoked during the first part ofthe test disappears when the legs are lifted up.Examiners: two doctors of chiropractic with 25 and10 years of clinical experience.All the examinations performed in one day.Prone Mobility Testing;k (95%CI); PABAKLeft L4–5, and L5-S1 facetmobility: k 0.17 ( 0.41,.06); PABAK 0.08Right L4–5, and L5-S1facet mobility: k 0.12( 0.41,0.18); PABAK 0.09Spinous L4–5 and S1mobility: k 0.05 ( 0.36,0.27); PABAK 0.11Left L1–4 facet mobility:k 0.17 ( 0.14,0.48);PABAK 0.44Right L1–4 facet mobility:k 0.01 ( 0.33,0.30);PABAK 0.44Spinous L1–4 mobility:k 0.02 ( 0.27,0.32)PABAK 0.07Sacroiliac mobility L: k 0.11 ( 0.21,-0.01);PABAK 0.54Sacroiliac mobility R: k 0.10 ( 0.18,-0.02);PABAK 0.64Prone Pain ProvocationTesting; k (95%CI):PABAKLeft L4–5, and L5-S1 pain:k 0.73 (0.51,0.95);PABAK 0.74Right L4–5, and L5-S1pain: k 0.52 (0.25,0.79);PABAK 0.54Spinous L4–5 and L5-S1pain: k 0.57 (0.32,0.83);PABAK 0.58Left L1–4 pain: k 0.46(0.17,0.75); PABAK 0.48Right L1–4 pain: k 0.38(0.06,0.69); PABAK 0.54Spinous L1–4 pain: k 0.21 ( 0.10,0.53);PABAK 0.34Right Sacroiliac pain: k 0.14 ( 0.19,0.47);PABAK 0.38Left Sacroiliac pain: k 0.33 (0.0,0.66); PABAK 0.54Prone Instability Test; k
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 8 of 20Table 3 Evidence table for low risk of bias studies assessing the reliability of manual palpation tests in patients with low back pain(Continued)Authors,YearCountryDesignSample Size(n)Case DefinitionIndex TestReliability(95%CI). PABAKTest 1: k 0.54 (0.27,0.81);PABAK 0.58Test 2: k 0.46 (0.15,0.77);PABAK 0.58Weineret al., 2006[29]USAInter-raterreliability (n 30)Chronic LBP, 3 months duration, 60 yrs. old.Palpation of the SI joints and lumbar spinousprocesses to identify pain: 1) SI joints: patientstanding on floor with shoes removed, examinerstanding behind patient exerts firm pressure oversacroiliac joint, palpation of right joint with rightthumb while standing to left side of patient; 2)lumbar spinous processes: examiner behind patient,firmly palpate spinous processes L1–L5 usingdominant thumbThe examiners underwent training in the protocolwith an expert physical therapists to refine andstandardize the physical examination proceduresTime between intra-rater assessments 5 minSI palpation; k (95% CInot reported)k 0.59Lumbar spinouspalpationk 0.47Standing flexion test: The subject is standing andthe examiner palpates the movement of PSIS as thesubject bends forward.Sitting flexion test: The subject is sitting and theexaminer palpates the movement of PSIS as thesubject bends forward.Gillett test: The subject is standing with theexaminer palpating the movement of PSIS as thesubject raises that knee toward their chest.Examiner: two physiotherapists with 1 yearexperience.Time between intra-rater assessments: 15 min.Inter-rater reliability; k(95% CI). PABAKStanding flexion testR- k 0.51 (0.08–0.95);PABAK 0.68L- k 0.55 (0.2–0.9);PABAK 0.60Sitting flexion testR- k 0.75 (0.42–1.08);PABAK 0.84L- k 0.64 (0.32–0.96);PABAK 0.68Gillet testR- k 0.41 (0.03–0.87);PABAK 0.60L- k 0.34 ( 0.06–0.7);PABAK 0.44Intra-rater reliability; k(95% CI). PABAKStanding flexion testRater 1: R- k 0.68 (0.35–1.01); PABAK 0.76Rater 1: L- k 0.61 (0.27–0.96); PABAK 0.68Rater 2: R- k 0.60 (0.18–1.02); PABAK 0.76Rater 2: L- k 0.51 (0.08–0.95); PABAK 0.68Sitting flexion testRater 1: k 0.73 (0.45–1.01); PABAK 0.76Rater 1: k 0.65 (0.34–0.96); PABAK 0.68Rater 2: k 0.65 (0.29–1.02); PABAK 0.76Rater 2: k 0.56 (0.21–0.90); PABAK 0.60Gillett testRater 1: k 0.42 ( 0.01–0.87); PABAK 0.60Rater 1: k 0.49 (0.09–0.89); PABAK 0.60Rater 2: k 0.25 ( 0.20–0.77); PABAK 0.52Motion Joint Palpation (n 49)Arabet al.,2009[20]IranIntra-rater andinter-rater reliability (n 25)LBP around posterior superior iliacspine and buttock, symptomduration unknown, 20–65 yrs. old.
Nolet et al. Chiropractic & Manual Therapies(2021) 29:33Page 9 of 20Table 3 Evidence table for low risk of bias studies assessing the reliability of manual palpation tests in patients with low back pain(Continued)Authors,YearCountryDesignSample Size(n)Case DefinitionIndex TestReliabilityRater 2: k 0.23 ( 0.02–0.67); PABAK 0.36Tong et al., Inter-rater2006 [27]reliability (n USA24)LBP, symptom duration unknown, 32 Seated flexion test: the evaluator palpates theto 81 yrs. old.cephalad movement at PSISs. As the subject bendsforward, the evaluator’s thumbs follow the motionof the PSIS cephaladStanding stork test: the evaluator’s thumb palpatesthe unilateral movement of left PSIS, and the otherthumb palpates the midline of the sacrum. Thesubject then flexes the left hip and knee to aminimum of 90 degrees. The same is repeated onthe right PSIS with the subject flexing the right hip.Standing flexion test: the evaluator palpates themovement of unilateral PSIS. As the subject bendsforward to touch the floor, the evaluator’s thumbsfollow the PSIS cephalad. The test is repeated oneach side.Sacral base position: the subject is sitting, theevaluator palpates the sacral base with the subject’strunk forward flexed and backward flexed. Apositive test is when one side of the sacrum ismore anterior or posterior when compared to theother side of the sacrum on the spine motions.Examiners: four physicians.Time between inter-rater assessments unknown.k (95% CI not reported);p valueSeated flexion test: k 0.06; p 0.68Standing stork test: k 0.27; p 0.07Standing flexion test:k 0.14; p 0.37Sacral base position:flexion k 0.37; p 0.002extension k 0.05; p 0.74Static Soft Tissue Palpation (n 150)Hebertet al.,2015[22]USAInter-raterreliability(n 32)Low back pain with 20/100 onmodified ODI, median duration ofsymptoms 205 days, 18 to 60 yrs.old.Multifidus lift test: to identify lumbar multifiduscontraction; participants prone and contralateralarm lifted with/without a hand weight whilemultifidus muscle palpated immediately lateral andadjacent to the interspinous space of L4–L5 andL5–S1.Examiners: 10 yrs. clinical experience andapproximately 5 yrs. research experience.Time between intra-rater assessments unknown.Inter-rater reliability; k(95% CI)L4–L5 no weight: k 0.75(0.52,0.97)L4–L5 weight: k .0.79(0.57, 1.00)L5-S1 no weight: k 0.81(0.62, 1.00)L5-S1 weight: k 0.80(0.59, 1.00)Jensenet al.,2013[24]DenmarkIntrarater andinter-rater reliability (n 43)LBP with or without radiculopathy,variable duration of symptoms, 16–60 yrs. old.Palpation of gluteal tender points: patient seated,tender points tested from right to left with 4 kgdigital pressure on upper outer quadrants ofbuttocks.Examiners: two consultants in rheumatology andrehabilitation.20 min between inter-rater assessments and 7 daysbetween intra-rater assessments.Intra-rater reliability(95% CI not reported)Rater A: R k 0.78; L k 0.69Rater B: R k 0.79; L k 059.Inter-rater reliabilityDay 1: R k 0.68; L k 0.53Day 2: R k 0.51; L k 0.50Walshet al.,2009[28]IrelandInter-raterreliability (n 45)Unilateral low-back related leg pain,mean duration of symptoms 5.6months, 18–70 yrs. old.Palpation of sciatic nerve: With the patient
Keywords: Manual palpation, Reliability, Validity, Assessment, Low back pain, Systematic review Introduction Low back pain (LBP) is the most prevalent musculoskel-etal condition in the general population [1, 2]. The point prevalence of LBP ranges between 1 to 58.1% and one-year prevalence ranges between 0.8 to 82.5% [3] depend-