Transcription
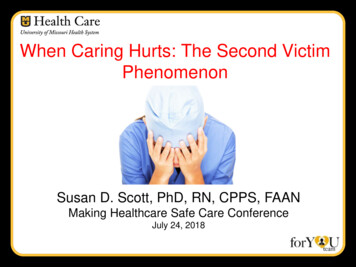
When Caring Hurts: The Second VictimPhenomenonSusan D. Scott, PhD, RN, CPPS, FAANMaking Healthcare Safe Care ConferenceJuly 24, 2018
ObjectivesUpon completion of this presentation, participants shouldbe able to1. Understand the second victim phenomenon.2. Describe what you can do differently tomorrow to help acolleague who is suffering as a second victim.
WARNINGRatedE Professional RatingThis content may contain EmotionalLabor!!!!!
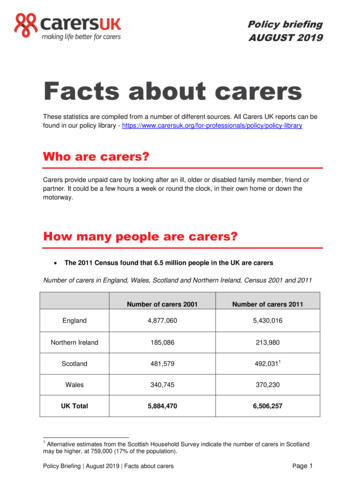
An Epidemic?44,000-98,000 deaths/year in U.S. due to preventableadverse events (Kohn et. al, 2000).Revised estimates at least 210,000 (and possibly morelike 400,000) die in U.S due to preventable harm (James,2013).With revised estimates: At least 4 clinicians/patient 840,000 to 1.6 million clinicians impactedKohn, LT, Corrigan, JM, & Donaldson, MS. (2000). To err is human: building a safer health system. Washington, D.C.:National Academy ofSciences Press.James, J.T. (2013). A new, evidence-based estimate of patient harms associated with hospital care. Journal of Patient Safety, 9(3), 122-128.
“Medicine used to be simple,ineffective and relatively safe. now itis complex, effective, and potentiallydangerous"Sir Cyril ChantlerLancet 1999; 353:1178-91
History of the PROBLEMAdverse event reviews – individuals at the ‘sharp end’noted to be experiencing ‘predictable’ behaviors post event
Review of the LiteratureAlbert Wu, MD“Virtually every practitioner knows the sickening realization of making a bad mistake.You feel singled out and exposed .You agonize about what to do Later, the eventreplays itself over and over in your mind”Wu, A. (2000). Medical error: the second victim. The doctor who makes the mistake needs help too. British Medical Journal, 320, 726-727.
Commonly Heard PhrasesThiseventshook meto mycore.”“This hasbeen aturningpoint in mycareer.”“It just keepsI’m going to checkreplaying overout my options asa Walmart greeter.and over inI can’t mess thatmy mind.”up.”“I’ll never bethe same.”.”
Second Victims Defined “Healthcare team members involved in anunanticipated patient event, a medical errorand/or a patient related injury and becomevictimized in the sense that they are traumatizedby the event.”Scott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M. M., Brandt, J., & Hall, L. W. (2009). The natural history of recovery for thehealthcare provider second victim after adverse patient events. Journal of Quality and Safety in Health Care, 18, 325-330.
What is a Second Victim?A Qualitative Research Project is Initiated
Qualitative Research OverviewParticipants 31Females 58%Average Years of Experienceo MD7.7o RN15.3o Other 17.7Average Time Since Event 14 monthso Range – 4 weeks to 44 months
High Risk Scenarios Patient ‘connects’ staff member to familyPediatric casesMedical errorsFailure to rescue casesFirst death experienceUnexpected patient demise
Stages of Healing: The Second VictimRecovery TrajectorySurvivingChaos nalFirst AidMovingOnImpact RealizationScott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M. M., Brandt, J., & Hall, L. W. (2009). The natural history of recovery for thehealthcare provider second victim after adverse patient events. Journal of Quality and Safety in Health Care, 18, 325-330.
“ I will never forget this experience This patient willalways be with me – I think about her often Becauseof this, I am a better clinician! ”
What Second Victims Desire
Second Victim InterventionsSecond victims want to feel.AppreciatedRespectedValuedUnderstoodLast but not least .Remain a trustedmember of the team!
Benefits of Clinician SupportStaff have a way to get their needs meet after goingthrough a traumatic eventHelps reduce the harmful effects of stressProvides some normalization and helps theindividual gett back to their routine after a traumaticeventPromotes the continuation of productive careerswhile building healthy stress management behaviors
Challenges to Providing Support Stigma to reaching out for help Intense fear of the unknown Fear of future legal woes - HIPAA,Confidentiality ImplicationsHigh acuity areas have little time to integratewhat has happenedFear a compromise of collegial relationshipsbecause of event
Support Basics Donot try to fix it Bea good listener! Avoidsecond-guessing performance Provide Letemotional first aidthem know you care
Thoughts About SupportClinicians have unique support needs.Health care facilities have unique culture.Both should be considered when designing anetwork of support for second victims.Two types of supporto One on oneo Group20
Second Victims Need SupportA systematic literature review of secondvictimization findings:1) Significant emotional toll on care providers2) Need for institutional support programs3) Varied approaches for support“Unethical not to have a clinician support program as the evidencesupported the emotional toll that being a second victim takes on aclinician and then in turn, their patients as well.”Butler, S. (2015). The Just Culture, Second Victimization, and Clinician Support: An Educational/Awareness Campaign. University ofMassachusetts-Amherst. Doctor of Nursing Practice Capstone.
Guidelines for Clinician CareInstitute for Health AEsWhitePaper.aspx
Guidelines for Clinician Care (continued)National Quality Forum – Safe Practice8: Care for the CaregiverProvide care to the caregivers(clinical providers, staff, andadministrators) involved in seriouspreventable harm to patients,through systems that also fostertransparency and performanceimprovement that may reducefuture harmful events.
Guidelines – Regulatory InsightsLD.04.04.05 – EP 9The leaders make support systemsavailable for staff who have been involvedin an adverse of sentinel event.http://www.jointcommission.org/improving Patient Worker Safety/
The forYOU Team is FormedAddresses research findingsPeer to peer support modelReferral systems coordinated to facilitateprompt careTwo Types of Supportive InterventionOne-On-OneGroup Debriefings
forYOU Team Objectives . Minimize the human toll when unanticipated adverseevents occur. Provide a ‘safe zone’ for faculty and staff to receivesupport to mitigate the impact of an adverse event. an internal rapid response infrastructure of ‘emotionalfirst aid’ for clinicians and personnel following anadverse event.
Support Strategies Interventions
Lessons Learned . Not all clinicians respond the same - everyone is unique Watch for isolation Many hidden ‘pearls’ within health care systems – Tier 3inventory Cast a big net - look for ‘hidden’ staff Consider building surveillance into existing practices(i.e. huddles, post code critique, disaster drills, etc.) Team briefings help to build team resilience andenhanced teamwork
A Point to Ponder .Wu, A.W., Shapiro, J., Reema, H., Scott, S.D., Connors, C., Kenney, L. and Vanhaecht, K.(2017). The impact of adverse events on clinicians: What’s in a name? Journal of PatientSafety. DOI: 10.1097/PTS.0000000000000256.
The Aftermath of No SupportNegative Impact onTeamworkLow MoraleImpaired JobPerformance
What Can You Do DifferentlyTomorrow? Understand the concept of Second Victims Talk about the Second Victim concept and spreadthe word – Awareness is the first intervention! Determine a way that you can make an individualdifference. If you have a ‘personal story’ about your experienceas a second victim, share it with a colleague in need. ‘Be there’!
AHRQ – CANDOR or
www.mitss.org
Questions “The longer we dwell on our misfortunes, the greater istheir power to harm us.” /foryou
References Butler, S. (2015). The Just Culture, Second Victimization, and Clinician Support: AnEducational/Awareness Campaign. University of Massachusetts-Amherst. Doctor ofNursing Practice Capstone.James, J.T. (2013). A new, evidence-based estimate of patient harms associatedwith hospital care. Journal of Patient Safety, 9(3), 122-128.Kohn, LT, Corrigan, JM, & Donaldson, MS. (2000). To err is human: building a saferhealth system. Washington, D.C.:National Academy of Sciences Press.Scott, SD. Second victim support: Implications for patient safety attitudes andperceptions. Patient Safety & Quality Healthcare. 2015. 12(5),26-31.Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural historyof recovery for the healthcare provider "second victim" after adverse patient events.Qual Saf Health Care. 2009 Oct;18(5):325-30.Scott SD, Hirschinger LE, Cox KR, McCoig M, Hahn-Cover K, Epperly KM, et al.Caring for our own: deploying a system-wide second victim rapid response team. JtComm J Qual Patient Saf. 2010 May;36(5):233-40.Wu, AW. Medical error: The second victim. The doctor who makes the mistake needshelp too. BMJ. 2000 Mar 18;320(7237):726-7.Wu, A.W., Shapiro, J., Reema, H., Scott, S.D., Connors, C., Kenney, L. andVanhaecht, K. (2017). The impact of adverse events on clinicians: What’s in aname? Journal of Patient Safety. DOI: 10.1097/PTS.0000000000000256.
To err is human: building a safer health system. Washington, D.C.:National Academy of Sciences Press. Scott, SD. Second victim support: Implications for patient safety attitudes and perceptions. Patient Safety & Quality Healthcare. 2015. 12(5),2631.- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history