Transcription
CBT TreatmentObsessive‐Compulsive Disorder1
OCD DEFINITION AND DIAGNOSIS NORMAL WORRIES & COMPULSIONS DYSFUNCTIONAL/ABNORMAL OBSESSIONS DSM IV DIAGNOSIS2
OCD DIAGNOSISDSM IV & ICD 10A significant source of distress and/or interferenceOBSESSIONSRecurrent, persistent thoughts, images or Impulsesexperienced, at some point, as intrusive and senselessAttempts to ignore and/or suppress and/or neutralise.Recognition of ownership of thoughts, yet perceived as ego‐dystonic; content unrelated to another Axis 1 diagnosis.3
OCD DIAGNOSISCOMPULSIONSRepetitive, purposeful and intentional behaviourPerformed in response to an obsession or according tocertain rulesDesigned to neutralise or prevent discomfort and/orcatastrophe.Awareness of their unrealistic and/or excessive nature.4
OCD: DIFFERENTIAL DIAGNOSISMAJOR DEPRESSIVE DISORDERGENERALIZED ANXIETY DISORDERHYPOCHONDRIASISSPECIFIC ILLNESS PHOBIAANXIETY DUE TO A GENERAL MEDICAL CONDITIONAPPETITIVE DISORDERSBODY DYSMORPHIC DISORDERDELUSIONAL DISORDER5
OCD DIFFERENTIAL DIAGNOSISOBSESSIVE‐COMPULSIVE PERSONALITY DISORDERABSENCE OF OBSESSIONS AND/OR COMPULSIONSPERVASIVE PATTERN OF:– ORDERLINESS– PERFECTIONISM– CONTROL– ONSET BY EARLY ADULTHOOD6
BEHAVIOURAL MODEL OF ANXIETYBEHAVIOURAL TREATMENT INVOLVES EXPOSURE TO FEAREDSTIMULI/SITUATIONS (CS) WITHOUT THE MALADAPTIVE RESPONSE TO PERMITTHE EXTINCTION OF THE CONDITIONED RESPONSE (CR)ADVANTAGES EXPLICIT PREDICTIONS DEMONSTRABLE PLAUSIBLE PRACTICAL/DIRECT TREATMENTDISADVANTAGES PREPAREDNESS INDIVIDUAL DIFFERENCES DEVELOPMENTAL INFLUENCES LACK OF TRAUMATIC ONSET SOCIAL & SYMBOLIC ACQUISITION OFANXIETY7
OCD TREATMENT APPROACHESBEHAVIOUR THERAPYRationale & Behavioural Assessment – see Figure 1Exposure and Response PreventionMaintenance and GeneralizabilityRelapse Prevention8
Typical Steps in the Behavioural Assessment ofOCDSpecify the rituals and obsessions in detailWhat situations evoke the rituals or obsessions (e.g., do the ritualsoccur only at home)?Are there any fluctuations in the symptoms (e.g. are they worse ifthe patient is alone)?What situations does the patient avoid as a result of OCD?Fig. 19
Typical Steps in the Behavioural Assessmentof OCD (Contd.)Do any thoughts, images, or impulses trigger (eg sacrilegious images, aggressiveimpulses) rituals or obsessions ?Construct hierarchy of target situations based on the amount of anxiety (SUDS scale),ritualising, or obsessing they evoke.What does the patient believe will occur if he or she does ritualise? How strong isthis belief?Are the patient’s symptoms being maintained by family interactions?Is the patient severely depressed? If so, consider trial of medication.Fig. 110
Typical OCD Fear Hierarchy
OCD: Client Exposure Guidelines
ERP Session by Session Habituation
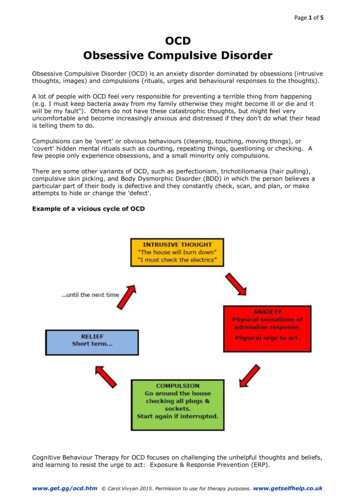
Stimuli and situations(Internal or external)Including external triggers,intrusive thoughts and informationCOGNITIONDANGER, THREATSafety seekingBehaviours (includingAvoidance, escape, andneutralising)Biological andPsychophysiologicalreactions14
CBT Model of OCD from Salkovskis (1985)Potential StimuliExtrinsic Mood DisturbanceAvoidanceTriggering Stimuli(Internal/External)Schematic Activation:accessibility of loss, threat orblame ideationIntrusion Ego DystonicIncreased AcceptanceAutomatic Thoughts EgosyntonicPerception ofResponsibilityRewardingNon-punishmentMood Disturbance,discomfort, dysphoria,anxietyExpectancyNeutralising ResponseEscape BehaviourReduced Discomfort15
A COGNITIVE THEORY OF .g.:SinfulDisgustingAlarmingINTERPRETATIONe.g.: Revealing about meWarning signsLosing controlGoing insaneI am dangerousDISTRESS/FEARI will cause harmPeople will reject meI will be locked upCONSEQUENCESe.g. Intense resistanceto obsessionsAttempts to block themNeutralisationsAvoidance BehaviourA postulated sequence of descriptions, interpretations and actions (from S.J. Rachman)16
Cognitive Obsessions and Covert RitualsIntrusive ThoughtNegative AppraisalIncreased Anxiety and WorryOvercontrolVigilance (Could I really do it?)Covert RitualsTestingTemporary Anxiety ReductionCycle starts all over again17
EXAMPLE OF THOUGHT/ACTION FUSION AND OCMETACOGNITION“I’m having a bad thought – that must mean I’m bad.”“I wouldn’t be having these thoughts if I wasn’t truly bad!”“The more bad thoughts I have, the more proof I have that I’m bad.”“Because I’m thinking so much about doing bad things, it must mean that I’m highly likely to do somethingbad.”“If I don’t try hard to prevent harm from happening, it is as bad as doing something bad on purpose.”“Since it is likely that I’m going to do something bad, I’d better watch out for it. I may even have to make surethat others are protected from my bad actions.”18
OCD: COGNITIVE TREATMENT APPROACHES– Psychoeducation of CBT Model of OCD– Shared Formulation– Identification of Intrusions & Appraisals– Cognitive Restructuring of Appraisals & Beliefs– Role of Compulsions, Neutralization & Avoidance: ERP– Behavioural Experiments– Modifying Metacognitive Beliefs20
OCD: Examples of Behavioural Experiments
OCD: Relapse Prevention
Susan: OCD Case FormulationExternal Triggerse.g. bathrooms, ‘dirty’ pupils, marking schoolwork,sharp objects, bathing the babyDysfunctional Beliefs--Intrusive Obsessional ThoughtsIdeas: e.g. I am contaminatedDoubts: e.g. I might assign the wrong markImages: e.g. Stabbing and drowning baby-Overestimates ofthe probability andseverity of dangerInflated sense ofresponsibility fordangerCertain thoughtsshould becontrolledCatastrophic Interpretations of ObsessionsHypervigilanceIncreasespreoccupation andsalience of cues-I will get ill & make my family illI can’t take the chance this will happenThe more I think it the more likely it is.I can & should control my thoughts or I amfully responsible for the outcomeThese thoughts mean that I’m a terriblemotherObsessional Anxiety/FearNegativeReinforcementOf safetybehaviours bydistressreduction-Safety-Seeking BehavioursAvoidance: e.g. pupils, public toilets, babyRituals: e.g. washing, checking, mentalhealthNeutralising: e.g. concealment, suppressionShort-Term Anxiety/Fear ReductionLack of Correction of BeliefsSafety behaviours preventcorrection of catastrophicbeliefsThought SuppressionLeads to more unwantedthoughts
Susan: An Exposure Hierarchy
OCD: Client Ratings25
Obsessive Compulsive Inventory (OCI)26
Responsibility InterpretationsQuestionnaire (RIQ)27
The Responsibility Attitudes Questionnaire(RAS)28
OCD for CBT: Some TipsUse Multi‐faceted AssessmentPsychoeducation & Motivational InterviewingWork to an AgendaStay focussed and calmHomework, homework, homework!Recognise Roadblocks‘The perfect is the enemy of the good’29
OCD Specify the rituals and obsessions in detail What situations evoke the rituals or obsessions (e.g., do the rituals occur only at home)? Are there any fluctuations in the symptoms (e.g. are they worse if the patient is alone)? What situations does the patient avoid as a result of OCD? 9. Fig. 1